BACKGROUND
Bronchiectasis is one of the differential diagnoses in the pediatric patient with chronic wet cough.1 Determining the etiology of the bronchiectasis is essential to initiate prompt and appropriate treatment, preventing further lung injury.2-4 Previous studies have revealed an association of childhood bronchiectasis and the presence of tracheomalacia and/or bronchomalacia, but causality has not been proven yet.5,6 It is hypothesized that impairment on airway clearance may lead to chronic inflammation and recurrent infections seen in these patients.7
CASE PRESENTATION
The authors’ case is an 8-year-old female who presented to the pulmonary clinic at age 3 years with poorly controlled asthma despite appropriate treatment, chronic wet cough, and mild clubbing. Initial workup revealed normal immune studies and sweat test. Chest CT with contrast showed right lower and middle lobe consolidations and narrowing of the proximal portion of the right main bronchi (right bronchomalacia). Given the findings on chest CT, a flexible bronchoscopy was performed, which revealed severe right bronchomalacia and purulent mucus plugging in the right main stem. The patient was admitted for intravenous antibiotics and initiation of airway clearance with intrapulmonary percussive ventilation. They were discharged on mucolytics and an airway clearance device (oscillatory vest). A year after the diagnosis of bronchomalacia, repeat CT revealed bronchiectasis in the same areas previous involved. The patient’s airway clearance regimen was intensified, establishing an outpatient sick plan with hypertonic saline, intrapulmonary percussive ventilation, and vest. Since, there has been a significant improvement on their clinical course as indicated by a decrease in airway secretions and improvement in the inflammatory pattern, as well as decreased neutrophils seen on subsequent bronchoalveolar lavage samples.
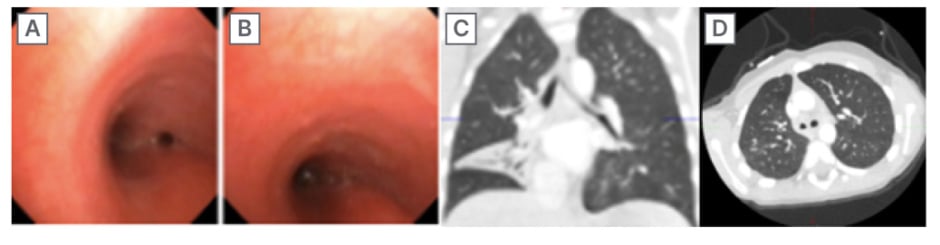
Figure 1: Right bronchomalacia (A and B); chest CT with right inferior and middle lobe consolidation (C); and chest CT at 1 year follow-up with right bronchiectasis (D).
CONCLUSION
Bronchiectasis is an important cause of morbidity in pediatric patients, especially in developing countries.8,9 Cystic fibrosis is the most common cause of bronchiectasis in the pediatric population; nevertheless, there are many other etiologies leading to bronchial dilatation.10
In the authors’ case, a pediatric patient with chronic wet cough was diagnosed with bronchomalacia and posteriorly developed bronchiectasis. Significant improvement was noticed after initiation of airway clearance.
Further studies should be performed in order to elucidate this hypothesis. Meanwhile, healthcare professionals should have a high index of suspicion for bronchiectasis in pediatric patients with tracheobronchial malacia and symptoms suggestive of bronchiectasis.








