INTRODUCTION
The use of multiparametric-magnetic resonance imaging (mpMRI)-guided intraoperative frozen-section analysis showed its effectiveness in reducing positive surgical margin (PSM) rates during nerve-sparing (NS) robotic-assisted radical prostatectomy (RARP) for organ-confined prostate cancer.1
The aim of the current study was to investigate the subgroup of patients with PSM occurring in a different site respective to the mpMRI index lesion (IL) location and to determine potential predictors of this event.
METHOD
From January 2014–April 2017, a total of 1,788 consecutive patients were subjected to RARP for prostate cancer. A preliminary mpMRI was performed on 98% of these patients. All patients received intraoperative frozen-section analysis to determine possible PSM. All data were prospectively collected in a customised database and retrospectively analysed. The primary outcome investigated was the concordance between PSM side and the location of the IL, as detected by the mpMRI. Univariable and multivariable analyses were used to identify potential predictors for PSM occurring distant to the mpMRI-IL position.
RESULTS
PSM were found in 187 (10.67%) patients with available preoperative mpMRI having received RARP. We considered a subgroup of 56 (29.90%) patients for analysis, in whom PSM occurred in a different site respective to the mpMRI IL location. In 76.80% of this subgroup, patients presented a Prostate Imaging Reporting and Data System (PI-RADS) score of 4 or 5 IL, while 11 patients (19.60%) had evidence at mpMRI of multifocal significant disease (secondary lesion PI-RADS >3). Out of 56 patients, the procedure was carried out as non-NS in 3 patients (5.10%); monolateral NS surgery was performed in 14 patients (25.00%), and bilateral NS in 39 (69.90%) patients.
In 85.80% of the cohort, a PSM occurred posterolaterally, and in the remaining 14.20% anteriorly.
Twenty (35.70%) patients of these 56 had evidence of PSM at the FSA, but in 17 (85.00%) the PSM was described as focal (<1 mm of extension).
Patient distribution according to the tumour staging, the IL Gleason score (GS), and the GS assessed at the level of the PSM (analysed for 22 out of 56 patients) is reported in Figure 1. At multivariable analysis, low (3+3) and intermediate (3+4) preoperative GS were significantly associated with the occurrence of PSM on a different site respect to the IL location (p<0.05).
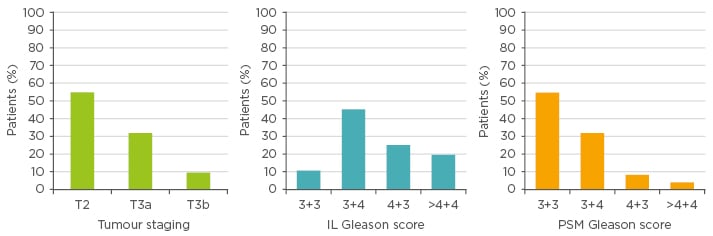
Figure 1: Patient distribution according to the tumour staging, the index lesion Gleason score, and the Gleason score assessed at the level of the positive surgical margins (analysed for 22 out of 56 patients).
IL: index lesion; PSM: positive surgical margins.
CONCLUSION
The results of this study demonstrated that the introduction of the mpMRI in the preoperative workout had lowered the rate of PSM. However, in some patients subjected to NS, discordance between the site of PSM and MRI lesions still exists. This issue has been described, in particular, for low–intermediate risk patients due to a more aggressive NS procedure performed distant from the mpMRI IL.








