Abstract
Vitamin D acts as a steroid hormone possessing important functions in calcium and phosphorus balance and bone health. The presence of vitamin D receptors (VDRs) in many tissues in the human body shows that this vitamin might have effects other than its role in maintaining bone health. Hence, many studies in the last two decades have reported an association between vitamin D deficiency and many musculoskeletal and extra-skeletal diseases. Despite the presence of clear evidence suggesting a causative relationship between musculoskeletal pain and osteomalacia developing as a result of long-term and severe vitamin D deficiency, a putative relationship between vitamin D deficiency and chronic widespread pain (CWP) has recently been an exciting area of discussion. The hypothetical role of vitamin D in the pathophysiology of pain, the availability of VDRs in the muscle tissue and central nervous system, particularly in the hypothalamus, and the reports on the development of muscle hypersensitivity associated with vitamin D deficiency, have provided a basis for a putative relationship between CWP and vitamin D status. This review will discuss these two problems that commonly occur within the general population, and endeavour to reveal this relationship in light of currently available studies.
INTRODUCTION
Vitamin D has been known to have a significant function in calcium (Ca) and phosphorus (P) balance and bone metabolism since the 1920s, when it was first discovered.1 Although there is not a widely accepted cut-off level, a serum 25-hydroxy vitamin D (25-OH D) level <20–25 ng/mL is considered to indicate vitamin D deficiency.1-4 It has been established that vitamin D deficiency is common, with a prevalence of 25–50% among the general population.1,3,5,6 The most widely recognised consequences of vitamin D deficiency are rickets in children and osteomalacia, osteoporosis, and increased risk of fractures and falls in adults.7-10 The availability of vitamin D receptors (VDRs) in many tissues of the human body shows that vitamin D might have other effects apart from its role in maintaining bone health.2,10 Indeed, many recent studies have reported a relationship of vitamin D deficiency with musculoskeletal disturbances, neuromuscular function disorders, infections, autoimmune diseases, metabolic syndrome, diabetes mellitus, cardiovascular diseases, respiratory diseases, cognitive function disorders, psychiatric disorders, and an increased risk of many types of cancer.2,3,6,9-11
Chronic widespread pain (CWP) is a global musculoskeletal disorder causing physical and psychological symptoms. Both the pathophysiology and effective therapies for CWP have yet to be identified. In the American College of Rheumatology (ACR)-1990 definition,12 CWP was defined as the pain lasting ≥3 months, both above and below the waist, on the right and left sides of body, and in the axial skeleton (cervical spine, thoracic spine, anterior chest, or lower back). CWP is very common (4.2–13.3%) in the general population.3 As two health problems that are commonly occurring in the general population, the relationship between vitamin D deficiency and CWP is a significant area of research that needs to be elucidated.
VITAMIN D DEFICIENCY
Sources, Synthesis, and Metabolism of Vitamin D
Vitamin D, which is one of the most important physiological regulators of Ca, P, and bone metabolism, is considered a steroid hormone as it is synthesised in the body, exerts effects through receptors in remote organs, possesses a biofeedback mechanism, and its structure resembles a cholesterol molecule.5 There are three main sources of vitamin D: cutaneous synthesis with sunlight, diet (natural or fortified), and supplements (prescription or over-the-counter).13 Vitamin D (D represents D2 or D3) is structurally related to two precursors: vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol). 7-dehydrocholesterol (provitamin3), which is naturally found in the skin, is converted to previtamin D3 through exposing the skin to solar ultraviolet B (UVB) radiation, and previtamin D3 is rapidly converted by heat to vitamin D3.5,13 This natural endogenous production is the most important and main source of vitamin D for the body.13-15
Exposure of arms and legs or face, arms, and hands to direct sunlight for 5–15 minutes at least three-times a week (suberythemal dose) is recommended for the synthesis of a sufficient amount of vitamin D in the skin.15 Vitamin D synthesis in the skin varies depending on the angle of the sun (maximum in the zenith angle), hour of the day (maximum at noon), and latitude and seasons. With ageing (especially >65–70 years), vitamin D synthesis decreases by 75% due to a decreased amount of 7-dehydrocholesterol, endogenous precursor in the skin.2 Dark skin directly decreases vitamin D synthesis as melanin absorbs UVB light. Also, sunscreen, obesity, smoking, and air pollution unfavourably affect skin synthesis to a great extent.2,16 The fact that many factors play a significant role in the skin synthesis of vitamin D, in contrast to the traditional approach, reveals that restricting the effect of clothing or skin tone alone cannot be placed at the forefront (Table 1).1,2,6,15,16
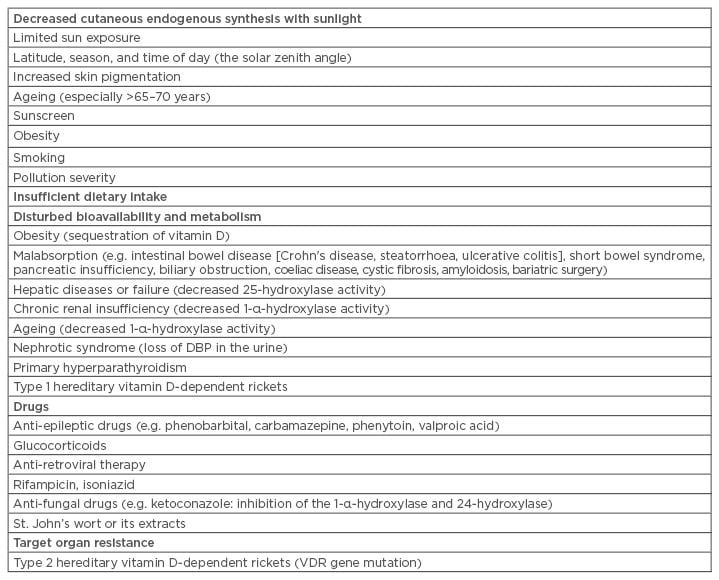
Table 1: Major causes of vitamin D deficiency.
DBP: vitamin D-binding protein; VDR: vitamin D receptor.
The amount of vitamin D supplied with natural food is extremely low.2,6 Vitamin D2, which is produced from ergosterol found in cell membranes of fungi through exposure to UV radiation, is a more limited source than vitamin D3. Vitamin D2 can only be supplied through certain foods (e.g. shiitake mushrooms, egg yolk) or supplements.2,6,15 Vitamin D3 can only be supplied through food of animal origin (e.g. cod liver oil, oily fish, egg yolk), fortified foods, and supplements.6 Once synthesised in the skin (vitamin D3) or taken with the diet (vitamin D3 or D2), vitamin D enters circulation in its biologically inactive form, which can be stored in the fat tissue or released upon demand.17 Vitamin D is transported by vitamin D-binding protein in the circulation and converted to 25-OH D by 25-hydroxylase in the liver and then to the active form 1,25-(OH)2D (calcitriol) by 1-α-hydroxylase enzyme in the kidneys. 25-OH D, although biologically inactive, is the major form of vitamin D in the circulation. Vitamin D synthesis is a self-limiting process and is regulated through a negative feedback mechanism involving serum Ca, P, parathyroid hormone (PTH), and fibroblast growth factor 23.5,13 Biliary excretion of inactive forms (1,24,25-OH D and 24,25-OH D) generated by 24-hydroxylation of 1,25-(OH)2D and 25-OH D represent the first step of inactivation in vitamin D metabolism.13
Biological Effects of Vitamin D
Through its receptor-dependent effects, 1,25-(OH)2D promotes sufficient bone (osteoid) mineralisation by increasing intestinal Ca and P absorption, decreasing Ca excretion from the kidneys, and inducing alkaline phosphatase and osteocalcin synthesis. PTH increases the level of 1,25-(OH)2D by increasing the activity of 1-α-hydroxylase enzyme.5 Both 1,25-(OH)2D and 25-OH D suppress PTH synthesis.6 In vitamin D deficiency, decreased levels of ionised Ca in the serum increase the PTH levels. PTH induces 1,25-(OH)2D synthesis, decreases renal Ca reabsorption, and decreases P reabsorption. As a result, vitamin D deficiency results in secondary hyperparathyroidism with normal or increased 1,25(OH)2D levels. Increased PTH and 1,25-(OH)2D levels cause bone resorption.5,6 1,25-(OH)2D exerts its effects not only on the kidney tissue, but through VDRs that are widely distributed throughout the body.6,10,13 With a multitude of targets in many tissues and ~200 genes (transcriptional regulation), 1,25-(OH)2D is known to regulate cell proliferation and differentiation, induce apoptosis, and inhibit angiogenesis and malignant transformation through VDRs.6,10
Vitamin D Deficiency and Insufficiency
Although 1,25-(OH)2D is the functional form of vitamin D, the serum 25-OH D level is the most frequently used parameter in clinical practice to reflect vitamin D status in the body. 25-OH D is the main form of vitamin D in the circulation and has a longer half-life (~3 weeks versus ~2 days) and only a certain portion of 25-OH D in the circulation is converted to 1,25-(OH)2D.1,6 However, optimal vitamin D levels that have gained wide acceptance have not been established. Although many studies have reported a cut-off level of 20–25 ng/mL, in the current approach, a 25-OH D level of ≥30–32 ng/mL is considered to be the lower limit for sufficient calcium absorption, PTH suppression, and optimal health status (skeletal and extra-skeletal).1-6,13
In the classification of vitamin D status, most authors have preferred to classify a 25-OH D level of <20 ng/mL as ‘vitamin D deficiency’, a level of 20–29 ng/mL as ‘vitamin D insufficiency’, and a level of >30 ng/mL as ‘sufficient’ vitamin D status.2,6,13,17 Vitamin D insufficiency can be regarded as the mild form of vitamin D deficiency, which causes bone loss, secondary to hypocalcaemia and secondary hyperparathyroidism. However, the definition of vitamin D insufficiency in current practice is used to consider the possible benefits of vitamin D, particularly on optimal extra-skeletal health, regardless of PTH level or suppression.
Vitamin D deficiency is a considerably is a common condition and the studies have yielded variable results as they were performed in populations with different characteristics, different age groups, different geographic areas, and using different cut-off levels. The studies have reported a prevalence rate ranging from 23–93% for vitamin D deficiency.1,6,16 Considering these prevalence studies and risk factors, it is estimated that 25–50% of the world’s general population and >1 billion people have vitamin D deficiency or insufficiency.1,5,6
CHRONIC WIDESPREAD PAIN
The widely known and accepted reference description of CWP was suggested for the first time by the ACR-1990 in diagnostic criteria of fibromyalgia (FM).12 In this diagnostic criteria, CWP was defined as pain lasting ≥3 months, both above and below the waist, on the right and left sides of body, and in the axial skeleton (cervical spine, thoracic spine, anterior chest, or lower back). In the latest FM preliminary diagnostic criteria published by the ACR in 2010, the definition of CWP in the ACR-1990 criteria was revised and the generalised nature of pain was included in the FM diagnostic criteria based on the examination of 19 anatomical areas.18 CWP differs from localised pain not only through its distribution, but also with higher pain intensity, longer pain duration, greater disability, more psychosocial problems, and lower quality of life.3 While the prevalence of CWP in the general population varies between the studies depending on methodological differences, it is reported to range from 4.2–13.3%.3 In a recent systematic review and meta-analysis (that included 25 articles) the prevalence of CWP was reported to range from 0–24%, and a level of 10% was reported to be the most accurate estimate.19
CWP is a clinical condition that could be caused by or associated with many diseases (Table 2),20,21 but it primarily originates from the musculoskeletal system, in most cases without an underlying organic pathology. CWP including FM is an important health problem without a known aetiology and definitive treatment. Whether CWP is related to vitamin D deficiency is an active area of research.
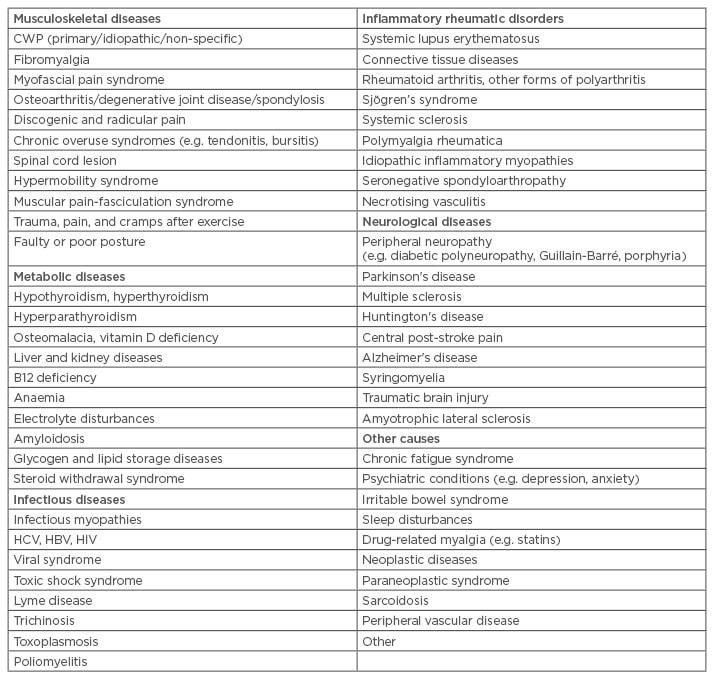
Table 2: Conditions and diseases causing chronic widespread pain.
CWP: chronic widespread pain; HBV: hepatitis B virus; HCV: hepatitis C virus.
RELATIONSHIP BETWEEN VITAMIN D DEFICIENCY AND CHRONIC WIDESPREAD PAIN
The presence of VDRs and 1-α-hydroxylase activity in the central nervous sytem, particularly in the hypothalamus, and functioning of vitamin D as a neuroactive steroid, points to a relationship between vitamin D and central hypersensitivity in chronic painful states.9,22,23 Vitamin D has been shown to play a role in the pathophysiology of FM through autoimmune and neural regulation, modulation of neurotransmitters, and upregulation of inflammatory pathways in chronic pain (i.e. transforming growth factor-β-1 [TGF-β-1], interleukin [IL]-4, and inhibition of prostaglandin activity).22,23 TGF-β-1 upregulated by vitamin D suppresses IL-1 and IL-2 and cytokines that are involved in chronic pain, such as tumour necrosis factor-α and interferon-γ.22,23 Vitamin D has been found to reduce the levels of nitric oxide that play a role in central sensitisation through inhibition of nitric oxide synthase.23 Similarly, demonstration of a relationship between vitamin D status and myopathy, fatty infiltration, and muscle hypersensitivity, has provided the basis for hypothetical pathophysiological mechanisms of vitamin D-CWP interplay.22,24,25
When considering the role that inflammatory cytokines, activated by the infections, play in the aetiopathogenesis of FM by modulating central and peripheral pain perception, the role of vitamin D in the regulation of the immune system is a reasonable theory that could explain musculoskeletal pain associated with vitamin D deficiency.3,26 Briefly, vitamin D has a potential role in the aetiology and persistence of chronic pain through anatomical, hormonal, neurological, and immunological mechanisms.23 On the other hand, patients with chronic musculoskeletal pain can develop vitamin D deficiency secondary to spending less time in open environments due to depression, limited mobility, or increased fat tissue.3,26
In an uncontrolled cross-sectional study involving patient groups of different ethnic origins, Plotnikoff and Quigley16 reported vitamin D deficiency in 93% of 150 patients with persistent non-specific musculoskeletal pain, a rate which is approximately two-fold higher than the cited studies conducted in a similar latitude, and they suggested the evaluation of patients with persistent non-specific pain for the presence of vitamin D deficiency. Block27 inquired into this study and reported a prevalence rate of 38% for vitamin D deficiency in patients with non-specific CWP, including FM, a rate similar to that in the general population. Of 9 patients with 25-OH D level <10 ng/mL, only 1 out of 6 patients who completed an 8-week course of vitamin D 50,000 IU/week therapy benefited from the replacement therapy.
As a major global health concern, treatment of chronic pain with a simple and pleasant means of therapy as vitamin D replacement has excited clinicians and this therapy has become the focus of research during the last two decades. Some of the studies that evaluated the relationship between vitamin D deficiency and various types of chronic painful conditions have reported a relationship,28-34 whereas other studies did not report any relationship.4,35-37 The studies addressing this interplay have used different methodologies and terminology, making the results confusing.
Although not a systematic review, a PubMed search was conducted to establish the relationship between vitamin D deficiency and CWP, with the keywords “vitamin D” or “vitamin D deficiency” and “chronic widespread pain” or “fibromyalgia” for the period between 1997 and March 2017. Twenty-four original articles (cross-sectional, observational studies) were returned from this literature search in terms of their methodology evaluating the relationship between CWP or FM and vitamin D status. Of these, only two studies were randomised controlled trials (RCTs)38,39 and eight studies evaluated vitamin D supplementation. Of these eight studies, two RCTs reported conflicting results, and six uncontrolled studies reported a significant improvement with vitamin D supplementation in patients with CWP.3,40-44 Out of the 16 remaining studies, 1124,45-54 reported a relationship between vitamin D deficiency and CWP, and 5 studies55-59 reported no relationship.
A comprehensive review of eight RCTs concluded there were not sufficient data to suggest the use of vitamin D outside chronic pain states, and that further large-scale RCTs were required in this regard.60 Muscogiuri et al.11 reported that currently available evidence does not support the role of vitamin D in other chronic diseases except for bone health; however, they highlighted the need for vitamin D supplementation in vitamin D deficiency to reduce the risk of developing chronic disease. In recent narrative17,22,23,61 and systematic reviews,26,62,63 sufficient evidence was not found for the use of vitamin D supplementation in chronic pain conditions or CWP/FM and no causative relationship was suggested; further studies were suggested to prove possible benefits in some specific painful conditions. Even further to that, the essential role of vitamin D in bone health (bone mineral density, fractures) and preventing falls seems to have become controversial.13,64-67
In the RCT conducted by Warner and Arnspiger,38 184 patients with musculoskeletal pain (primary FM) and 104 patients with osteoarthritis (controls) were compared with respect to mean 25-OH D level (diffuse pain: 29.2 ng/mL, controls: 28.8 ng/mL; p=0.78) and the prevalence of vitamin D deficiency (<20 ng/mL) (diffuse pain: 29%, controls: 20%; p=0.09), and no significant difference was reported between the groups. When 50 patients with FM and vitamin D deficiency (9–20 ng/mL) were randomised to treatment and control groups, no significant improvement in pain was found in patients who received ergocalciferol 50,000 IU/ week for 3 months compared to the control group. Additionally, no significant decrease was noted compared to pretreatment state. However, Wepner et al.39 (second of the two aforementioned RCTs) randomised 30 patients with FM and reported a significant reduction in the pain and positive effect in the perception of pain (on the physical role functioning scale of the Short Form Health Survey 36) in the treatment group compared to the control group.
Hsiao et al.68 performed a meta-analysis of 12 observational studies conducted to establish the relationship between hypovitaminosis D and CWP including FM. They observed a positive crude association between hypovitaminosis D and CWP and suggested that a level of 8–10 ng/mL could serve as a cut-off level determining this relationship. In contrast, in the systematic review of one RCT and eight cross-sectional studies conducted by Daniel and Pirotta,26 the association between vitamin D deficiency and FM was found to be inconclusive and, according to the best evidence, vitamin D supplementation had no effect; however, it was highlighted that the treatment of vitamin D deficiency in patients with FM would be beneficial with respect to long-term bone health and muscle strength, rather than pain.
CONCLUSION
Vitamin D deficiency is expected to occur commonly worldwide considering the presence of multiple factors affecting skin synthesis of vitamin D, the infeasibility of consuming a sufficient amount of vitamin D in the diet, and the presence of other risk factors that could affect vitamin D status. However, there is no established standardised minimum 25-OH D level required for optimal musculoskeletal and extra-skeletal health that is widely accepted in the scientific milieu. Uncertainty regarding the cut-off level for vitamin D deficiency/insufficiency leads to the use of different cut-off levels, causing limitations in the synthesis and analysis of different studies. According to current evidence, along with the putative role of vitamin D in extraskeletal health, its better-established role in musculoskeletal health (osteoporosis, fracture, and risk of falls) is also weak and debatable. Under these circumstances, the value/discriminative power of currently used cut-off levels (20–25 ng/mL) yielding >25% prevalence rate for vitamin D deficiency, seems to be questionable in differentiating physiological status from a pathological finding. Therefore, normal serum 25-OH D levels must be clarified with powerful studies.
Considering the hypothetical role of vitamin D in the pathophysiology of pain and the wide distribution of VDRs throughout the body (including muscle tissue and CNS), an association is expected between CWP/FM and vitamin D deficiency. However, studies supporting this putative relationship are scarce and of low quality. Musculoskeletal pain that could be associated with vitamin D deficiency is expected to be a widespread pain rather than regional pain and should respond to replacement therapy. Large-scaled double blind RCTs by clinicians specialised in musculoskeletal pain are required with detailed/ clear classification of pain and using specific cut-off levels on a specific and homogeneous group of patients. In light of the current data, vitamin D has no place in routine treatment of patients with CWP. In view of the papers reporting musculoskeletal and extra-skeletal benefits for vitamin D and that it is a cheap, simple, ‘pleasant’ and non-toxic treatment, vitamin D supplementation can still be considered to have a role for patients with risk factors or deficiency.








