Interview Summary
More than 3.4 million people worldwide are affected by systemic lupus erythematosus (SLE), a chronic, complex, and unpredictable autoimmune condition that can take years to diagnose. SLE, the most common form of lupus, frequently has a profoundly negative impact on the quality of life for patients, with many reporting chronic fatigue, anxiety, and pain as symptoms. Inadequate disease control, and associated side effects of current treatment for people with SLE, lead to recurrent flares in symptoms and high risk of organ damage. Fifty percent of people with SLE have irreversible organ damage within 5 years of diagnosis due to long-term oral glucocorticoid (GC) use, disease flares, and persistent disease activity. SLE mortality remains unacceptably high and is one of the top 10 causes of death in young women in the USA. Although the speed of innovation has accelerated in recent years, there is still a great need beyond symptom management to tackle the underlying cause of the disease and achieve clinical remission for patients. In 2023, the European Alliance of Associations for Rheumatology (EULAR) updated its recommendations for SLE management, elevating the importance of treating to target remission or low disease activity with elimination of steroids, where possible, to reduce the risk of organ damage and adverse outcomes in patients. EULAR defines remission in SLE, according to the Definition of Remission in SLE (DORIS) criteria, as having no disease activity while receiving treatment, but GC ≤5 mg/day. Two leading SLE experts, Ian Bruce, Queen’s University Belfast, UK, and Julia Weinmann-Menke, Medical Center of the Johannes Gutenberg University, Mainz, Germany, discuss why remission is now a realistic goal in SLE, and how aiming for early and sustained remission can help to improve patient outcomes and address urgent unmet medical needs.INTRODUCTION
SLE is a chronic and complex heterogeneous autoimmune disease in which the immune system dysfunctions and inappropriately attacks healthy tissue within the body.1 Over 3.4 million people worldwide are affected by SLE, but it can take years to diagnose.2,3 The disease primarily affects women of childbearing age,2 disproportionately affecting those of African, Asian, or Hispanic ethnicities.1,4,5 Both environmental and genetic factors may influence SLE development. The disease typically follows a chronic relapsing and remitting course, but in severe cases it can be fatal,1 such that SLE mortality remains high and is among the top 10 causes of death in young women in the USA.6 Whilst SLE can manifest differently in each person, an estimated 50% of patients develop organ damage, with accumulated damage attributed to disease activity, flares, and treatment-associated side effects.7,8
The long-term impact of GCs is a major clinical challenge in SLE. While these treatments help to provide relief from symptoms of SLE, they do not target the underlying drivers of the disease.9 Approximately 80% of people with SLE are treated with GCs to provide symptom relief and control flares; however, GC use contributes to irreversible organ damage.7,9 As a result, many patients have an inadequate response to treatment and few achieve lasting remission.10
In recent years, advances in scientific research have resulted in an increasing number of new and targeted strategies and options available for SLE, as reflected in the updated recommendations from EULAR in 2023 that pave the way for healthcare professionals (HCP) to elevate their treatment goals and ultimately improve outcomes.11 To learn more about the implications of these updated recommendations, and how they can transform patient care for those living with SLE, EMJ sat down with two leading experts in SLE care, Bruce from Queen’s University Belfast, UK, and a member of the EULAR recommendations taskforce, and Weinmann-Menke, an SLE Outpatient Clinic Working Group Leader at the Medical Center of the Johannes Gutenberg-University, Mainz, Germany.
THE UPDATED EULAR RECOMMENDATIONS FOR THE MANAGEMENT OF SYSTEMIC LUPUS ERYTHEMATOSUS
The 2023 EULAR recommendations for SLE management include five overarching principles (Figure 1), elevating the need for early detection and early treatment to target SLE remission or, at least, low disease activity.11 As explained by Bruce, the evidence-based recommendations assist HCPs to set SLE care standards within their practices, encouraging a multidisciplinary and individualised approach to care that will ultimately lead to better patient outcomes and reduced long-term health consequences. Weinmann-Menke discussed how the EULAR recommendations seek to encourage HCPs to think about individual patient goals,11 for example: “When you have a patient who already has organ damage, who is not taking their medication, or who has a lot of side effects, then you have to think, ‘can I change, can I do something different?’”
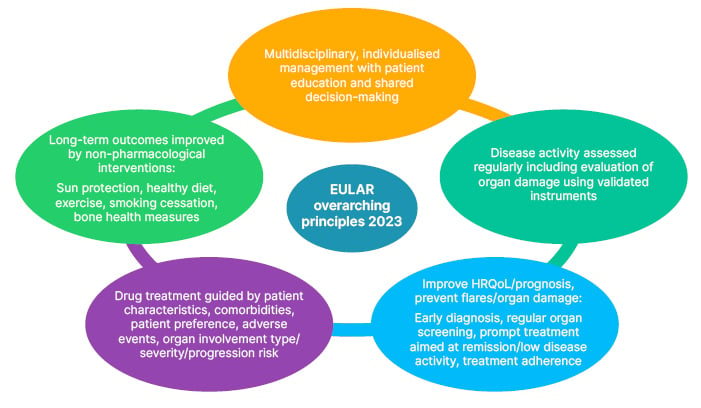
Figure 1: Overarching principles of EULAR recommendations for management of patients with systemic lupus erythematosus.11
EULAR: European Alliance of Associations for Rheumatology; HRQoL: health-related quality of life.
POSITIONING EARLY INTERVENTION AND REMISSION AT THE FOREFRONT OF SLE TREATMENT
A key pillar of SLE management in the updated EULAR recommendations includes pursuing a treatment target, ideally remission and treatment adherence. In particular, the recommendations stress ‘prompt initiation of treatment aiming at remission or low disease activity state if this is not possible’.11 The definition of remission in SLE (DORIS), as used in the recommendations,11 is described as a clinical SLE Disease Activity Index (SLEDAI)12 score of 0; a Physician Global Assessment (PGA) score <0.5; use of antimalarials and/or stable immunosuppressives, including biologics; and on ≤5 mg/day prednisolone (or equivalent).13 Lupus Low Disease Activity state is described as ≤4 on the SLEDAI; ≤1 on the PGA; no major organ system activity; no new disease activity; using sustained immunosuppressive therapy and approved biologicals; and on ≤7.5 mg/day prednisolone (or equivalent).14
“We’re in a position now where we can actually control disease better,” Bruce discussed. “Therefore, we want people to aim to treat to target, and that means aiming for remission.”15-18 He explained that patients who achieve remission, particularly prolonged remission, experience “less damage over time, their quality of life improves, and [they have fewer] hospitalisations.”11 Weinmann-Menke agreed, saying that “when a patient is diagnosed early with no or minimal damage or activity, physicians should consider treating intensely for a short time to try to give their patients the best chance at remission, and to avoid organ damage that will impact their future.” 19,20
Achieving early remission, Weinmann-Menke noted, could require “more therapy in the first weeks and months, [which] might be harder for the patient due to increased side effects, and general feelings of malaise preventing them from daily activities… but then they are in remission and can have a much better quality of life, improved health outcomes, and a better lifespan. That’s the most important part, that you aim to prevent organ damage when you start early with intense, strong immunosuppression.”19,20
THE ROLE OF NEW APPROACHES IN SLE MANAGEMENT
Patients often rely on prolonged use of treatments, such as GCs, that offer some relief from symptoms but may not target the underlying drivers of SLE.9,10 The updated EULAR recommendations advocate for earlier introduction of immunosuppressive therapies, without the need for prior failure to one or more ‘conventional drugs’, to achieve remission or low disease activity state with lower use of GCs.11
Treating to target, Bruce stated, “means you should consider being much more proactive in the way you add treatments.” The essential message in the EULAR recommendations, he explained, is that in some cases “it’s better when you use a combination of therapies than when you use traditional approaches. This is where the move towards early diagnosis and rapid early suppression of disease and disease control comes in.” Bruce highlighted how a number of “trials have demonstrated better outcomes with targeted therapeutic options compared to standard therapy alone, supporting the combination of therapies from the outset for improved outcomes, which allows you the possibility of getting closer to these target states.”18,21
One goal of the updated recommendations, said Weinmann-Menke, is to “recommend early use of immunosuppressive drugs to avoid long-term exposure to GC, so you don’t need, one, two, three steps and use all conventional drugs before you start with biological therapies. It’s similar to the approach in rheumatoid arthritis, detect early and treat early with a sufficiently specific drug to reduce patients’ risk of organ damage, and hopefully achieve remission.” Bruce agreed, discussing how the EULAR recommendations11 have “opened the possibility of using targeted treatments much earlier in the disease course, instead of them just being for people several years into their disease who’ve cycled through multiple different drugs and not had a good response. If you consider that your patient hasn’t improved sufficiently to reach your target state, despite standard care, or if you’ve not been able to get them off steroids, that will reveal itself within the first 6−8 months, then one of those considerations should be to review alternative treatments.”
Non-pharmacological management and self-management strategies, including sun protection, smoking cessation, a healthy diet and exercise, and measures to promote bone health, can help enhance health-related quality of life and are progressively substantiated through growing evidence. A dedicated set of EULAR recommendations on non-pharmacological management of SLE were also recently published to promote use of such interventions alongside pharmacotherapy to improve the overall quality of care.22
Both experts concluded that networks of expert groups, multidisciplinary teams, and linking with other colleagues and centres can all be useful to increase understanding of available treatment approaches and counter misconceptions surrounding the use of more recent therapeutic options.
WHY IS IT IMPORTANT TO LIMIT GLUCOCORTICOID USE?
GCs are used by approximately 80% of people with SLE to control flares, despite GC use contributing to irreversible organ damage.7,9 Numerous studies have shown how myriad long-term adverse events are associated with GC use, in a dose-dependent and cumulative manner, including venous thromboembolism, organ damage, weight gain, cardiovascular disease, cataracts, fractures, acne, and skin bruising.7,23-25 Reduction of even 1 mg/day of steroids can reduce the risk of organ damage.26
Adopting the steroid-sparing approach to treatment is critical to achieving treat to target goals in SLE. The 2023 EULAR recommendations encourage cautious use of GCs, stating that they should only be used if clinically required “in view of the detrimental effects of their long-term use and the approval of new agents with GC-sparing effects.” If GCs are used, once sustained remission is achieved, EULAR recommends gradual treatment tapering and complete withdrawal of steroids, if possible.11 “We pushed very hard to make sure that coming off steroids was a central pillar of the EULAR recommendations,” said Bruce.
While the recommendations do include the use of steroids if needed, they caution that they should be “dosed based on the type and severity of organ involvement.”11 “We [need to] think from Day 1 about people’s lifelong exposure to steroids,” said Bruce. “It’s very easy to put people onto steroids and have them in the background for a very long period of time. People will get to 5 mg and say, ‘that’s the job done’, but you have to keep pushing down.” If that is not possible, continued Bruce, “it raises the question, ‘why can I not get these patients off steroids? What should I be modifying?’” This requires, said Bruce, a measure of “being on the front foot with SLE treatment, trying to be proactive about planning what you’re doing.” Weinmann-Menke agreed, saying “we have to write down [in medical records] that ‘we want to reduce [glucocorticoids] to zero or the minimal tolerated dose, so that you remember every time [to ask] ‘can I reduce by 1 mg or something?’’’ She explained how early use of targeted immunosuppressive drugs can be one way to reduce the need for glucocorticoids.
IMPLEMENTING THE EULAR RECOMMENDATIONS INTO CLINICAL PRACTICE
While remission should be an achievable goal for many patients, regular clinical visits and assessments of patient care needs to remain an important area of focus. EULAR recommends that SLE disease activity should be assessed at each clinic visit (the frequency depending on physician’s discretion), with evaluation of organ damage at least annually, using validated instruments. Bruce stressed the importance of using instruments that include SLEDAI12 and the British Isles Lupus Assessment Group (BILAG) measure.27
The results from these assessments, along with blood tests, may point to high disease activity, even when a patient’s testimony indicates that their disease is under control. Bruce explained that “if you’re proactively monitoring patients from early on, particularly after a change of therapy, that will reveal how well the treatment is doing. If you’re seeing them every 3 months, you’ll get an idea of the pattern of improvement, and whether it’s getting toward low disease activity or remission, or whether they’ve still got ongoing, grumbling disease. The marker of that is their clinical symptoms and the amount of steroids they’re taking.” Treatment reviews should be carried out on a case-by-case basis, dependent on the type of treatment and the manifestations present, Weinmann-Menke outlined. With some drugs, she explained, “you may have to wait 6−9 months, sometimes a year, until you get the full response,” but with others, “I know after 3 months if it’s working or not.”
Another key challenge when it comes to managing SLE is the balance of achieving an improved, everyday quality of life for patients while focusing on long-term treatment. Both Weinmann-Menke and Bruce described how patients may have concerns about the impact that SLE will have on aspects of their life such as their careers and families. This may depend on disease severity, disease control, and treatment adherence.1,11 Weinmann-Menke explained how some patients may not be able to work in the first 3−6 months following initial diagnosis. Additionally, she added that, “when you reach remission, the patient needs to be aware that SLE is not gone forever, it can come back every day, every week. That is sometimes challenging for the patient in their daily life.”
Given the nature of SLE, frequent touchpoints with patients are critical to ensure that barriers such as treatment adherence are addressed. Weinmann-Menke stressed the importance of discussing certain aspects of SLE management with patients from the beginning. “Sometimes you need weeks, months, or years to convince the patient to take medication regularly because they are often young and want to live their life without visiting the hospital and taking medications. It’s hard sometimes to convince a patient that this is necessary, but when they make it through the first year, then it’s kind of normal after this.”
CONCLUSION
For many years, patient care and outcomes in SLE have been impacted by low awareness of this complex and unpredictable disease. However, recent advances in care and clinical recommendations for SLE management are encouraging and highlight that remission in SLE is now a realistic goal.11 Collaboration between patients, HCPs, and policymakers will help to put these new clinical recommendations into practice to enable optimised and consistent approaches to early diagnosis and treatment, to ultimately ensure more people living with this complex disease can reach remission. “We need to keep striving to manage people better,” concluded Bruce.
The 2023 EULAR recommendations for SLE management call for earlier diagnosis and earlier introduction of advanced and targeted immunosuppressive therapies, including biologics. This can limit disease activity and flares and prevent organ damage,11 which may also at times result from excessive GC use.7,8 The recommendations elevate the importance of treating to remission or low disease activity to improve disease outcomes, and of lowering GC use. Following these recommendations, Weinmann-Menke concluded that this could mean that, now, “[if we treat earlier] hopefully we do not see really severe patients with already established organ damage.”
Veeva ID: Z4-69824
Date of Preparation: October 2024







