BACKGROUND
Past research has repeatedly shown that patients with inflammatory rheumatic disease (IRD) experience restrictions in work participation. Times of crisis tend to bring out such vulnerabilities. The global COVID-19 pandemic is a prime example, and this event possibly widened the work participation gap between patients with IRD and the general population. On the other hand, some of the consequences of the pandemic, such as an increase in working from home, might also provide benefits for patients with IRD.
MATERIALS AND METHODS
Researchers from Maastricht, the Netherlands, aimed to compare several work participation outcomes during the COVID-19 pandemic between patients with IRD and population controls. A cross-sectional study was carried out within an ongoing Dutch, prospective COVID-19 cohort of patients with IRD and matched controls. In March 2022, participants provided information about their work outcomes and work characteristics in 2022 (‘current’) and in 2020 (‘pre-pandemic’, retrospective).
Two work outcomes were considered: adverse work outcome and work ability. Adverse work outcome was defined as any of the following in the 2020–2022 period: withdrawal from paid work, working hours reduction, or long-term sick leave. Work ability was rated on a scale of 0–10 (worst–best), and both current work ability in 2022 and the change during the pandemic from 2020–2022 were considered. These work outcomes were compared between patients and controls in multivariable logistic and linear regression analysis, respectively. In addition, stratified analyses were conducted to identify vulnerable groups. Finally, participants were asked to rate the influence of four typical remote work characteristics (care for children, absence of colleagues, employer support such as a desk or chair, reduced work commute) on their work performance while working at home.
RESULTS
In total, 992 patients and 443 controls were working pre-pandemic. From these, 227 patients (23%) and 79 controls (18%) experienced any-cause adverse work outcomes following pandemic onset (p=0.04). Both patients and controls attributed only 15% of these events to COVID-19 (personal COVID-19 illness or national pandemic measures).
In adjusted analyses, patients were more likely to experience any-cause adverse work outcomes, with odds ratios (OR) ranging from 1.6–3.3 for patients versus controls in various stratified analyses, but not COVID-related adverse work outcomes (Figure 1). Female patients (OR: 2.2), patients with comorbidities (OR: 3.3), and patients with physically demanding jobs (OR: 3.0) were particularly vulnerable for any-cause adverse work outcomes. While the change in work ability during the pandemic was small and very similar in groups, current work ability in 2022 was worse in female patients compared with controls. Of note, a history of COVID-19 was not associated with any of the work outcomes.
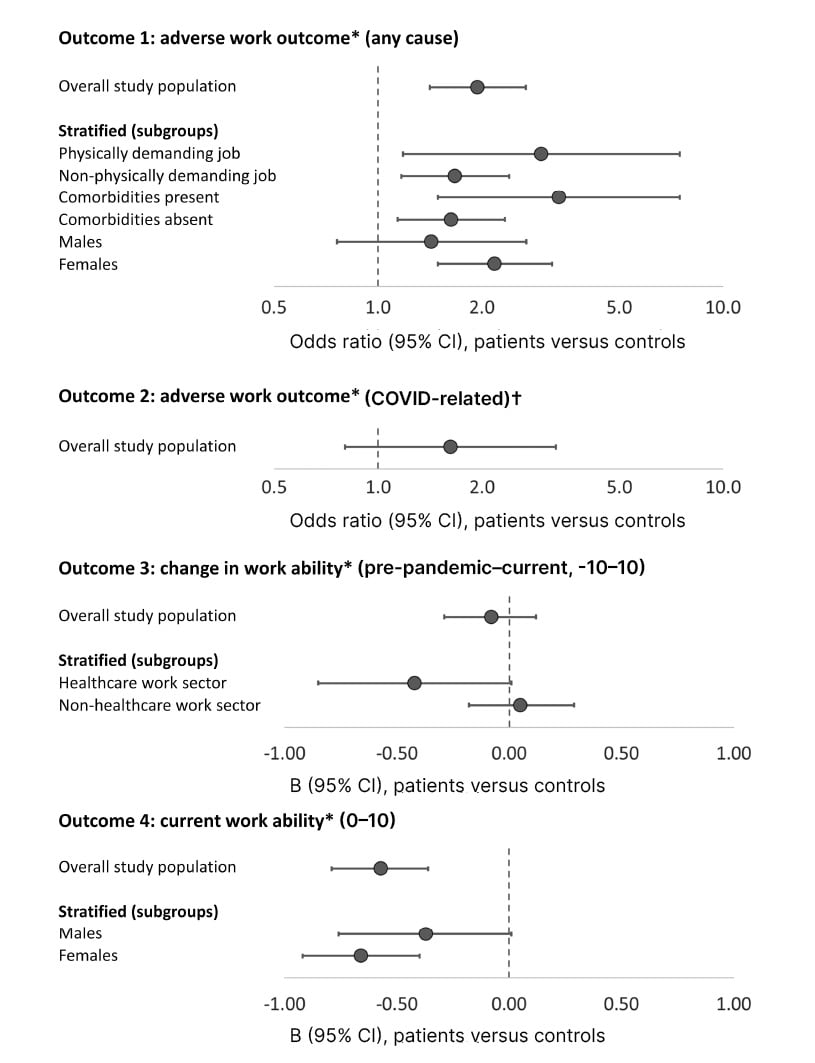
Figure 1: Association between group (patients versus controls) and adverse work outcome or (change in) work ability in multivariable regression analysis.
*Covariables explored in models (retained if confounder for group and outcome, or if significantly associated with outcome): age (outcomes 1 and 2), gender, education, comorbidities (outcome 4), past COVID-19 infection, COVID-19 vaccination, work sector, job demands, type of employment (outcome 2), working hours (outcomes 3 and 4), work location (outcome 4). Covariables marked in bold if significant.
†Defined as adverse work outcome attributed by the patient to either impact of COVID-19 on personal health or impact of national pandemic measures against COVID-19.
An odds ratio >1 or B <0 indicates a worse outcome in patients compared with controls (higher likelihood of adverse work outcome, a greater decrease in work ability, or lower current work ability).
B: regression coefficient; CI: confidence interval.
When working from home, care for children and absence of colleagues had varying effects on work performance (positive 19% and 24%, respectively; negative 34% and 57%, respectively), while employer support and reduced commuting had mainly positive effects (83% and 86%). These results were similar in patients and controls.
CONCLUSION
This study demonstrates that the work participation gap between patients with IRD and the general population persists. However, there was no clear indication that the gap increased due to the pandemic: patients did not have more COVID-related adverse work outcomes or a greater loss in work ability during the pandemic. Furthermore, although the observation that patients with a history of COVID-19 do not have worse work outcomes is reassuring, the long-term effects of past infection on work participation need further study.







