BACKGROUND AND AIMS
Axial spondyloarthropathy (axSpA) is a form of inflammatory arthritis that primarily affects the axial skeleton and sacroiliac joints but can also be associated with peripheral arthritis. Rapid advances in the field of axSpA have led to faster detection, diagnosis, and treatment of this disease. This improved management has led to enhanced level of function and quality of life for patients; however, despite this, a proportion of patients are still requiring joint replacement surgery.
The Ankylosing Spondylitis Registry of Ireland (ASRI) is a source of epidemiological data on patients with axSpA in Ireland. Given the large size of the ASRI to date, it provides a prime opportunity to analyse patients with axSpA requiring joint replacement surgery. A detailed analysis was undertaken to determine trends in disease and baseline demographics of patients with axSpA requiring joint replacement surgery.
MATERIALS AND METHODS
Patients requiring joint replacement surgery were compared to the rest of the ASRI cohort. Baseline demographics, as detailed in Table 1, were compared between the groups. In addition, scores of disease activity and functional impairment (Bath Ankylosing Spondylitis Disease Activity Index [BASDAI], Bath Ankylosing Spondylitis Functional Index [BASFI], The Health Assessment Questionnaire [HAQ], the Ankylosing Spondylitis Quality of Life questionnaire [ASQoL], and Bath Ankylosing Spondylitis Metrology Index [BASMI]) were analysed.
An independent, two-tailed t-test was used to determine statistical significance between the groups. Further analysis on sex, human leukocyte antigen (HLA)-B27 status, comorbidities, and medication exposure was performed using a chi-squared test for independence. A p value of <0.05 was deemed significant.
RESULTS
In total, 33 (3.8%) of the 860 ASRI patients underwent joint replacement surgery. These patients were noted to be significantly older than the rest of the cohort (55.3 versus 45.1 years; p<0.01), with a longer disease duration (31.6 versus 18.3 years; p<0.01) and higher rates of HLA-B27 positive tests (94.7% versus 80.2%; p<0.01). No significant differences were found between the sexes (Table 1).
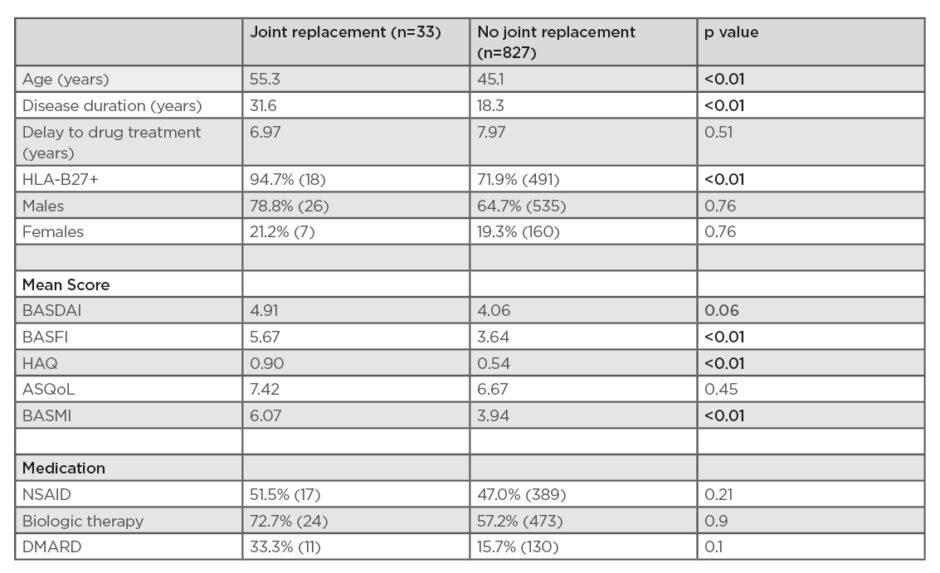
Table 1: A comparison of patients with axial spondyloarthropathy requiring/not requiring joint replacement surgery, using The Ankylosing Spondylitis Registry of Ireland (ASRI) dataset.
ASQoL: The Ankylosing Spondylitis Quality of Life questionnaire; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; BASFI: Bath Ankylosing Spondylitis Functional Index; BASMI: Bath Ankylosing Spondylitis Metrology Index; DMARD: disease-modifying antirheumatic drugs; HAQ: Health Assessment Questionnaire; HLA-B27: human leukocyte antigen-B27; NSAID: nonsteroidal anti-inflammatory drugs.
A number of comorbidities were analysed: patients requiring joint replacement had higher rates of all test comorbidities, with the exception of tuberculosis, chronic lung disease, and depression. No significant difference was found between medication exposure rates, although the joint replacement population did have higher rates of nonsteroidal anti-inflammatory drugs, synthetic disease-modifying antirheumatic drugs (sDMARD), and biologic therapy usage than the rest of the population; however, this did not reach significance.
These patients also achieved poorer scores for all measures of disease activity, although this only reached significance in the BASFI (5.67 versus 3.64; p<0.01), HAQ (0.9 versus 0.54; p<0.01), and the BASMI (6.07 versus 3.94; p<0.01).
CONCLUSION
Patients requiring joint replacement surgery, although few in number, represent a cohort with significantly impaired function and quality of life.
This is likely because these patients were older with more established disease. It is therefore not surprising that this cohort had higher rates of several comorbidities and significantly worse spinal mobility.
As registries continue to develop, it will be interesting to see if rates of joint replacement surgery will decline with increased use of biologic therapy at an earlier stage of disease. This will help to differentiate patients requiring joint replacement surgery caused by underlying inflammatory arthritis and osteoarthritis.








