BACKGROUND AND AIMS
Raynaud’s phenomenon (RP) in systemic sclerosis (SSc) can lead to chronic digital ischemia, ulcerations, and necrosis with significant pain and hand function loss. Not only the most common and earliest SSc manifestation, SSc-RP also has the highest patient-reported disease impact on quality of life. Early interventions for RP can have an important impact on altering the disease course by preventing ischemia-reperfusion injury and subsequent oxidative stress with further endothelial dysfunction and fibrosis in SSc.
METHODS
This study describes the practices for SSc-RP management among community-based rheumatologists in the US. Rheumatologist- diagnosed adult patients with SSc who were enrolled in the FORWARD study1 between 1999–2023 were assessed for the use of vasoactive medications for RP as well as medications worsening RP. Data were collected semi-annually with comprehensive questionnaires and validated using medical records. Medications for RP included calcium channel blockers (CCB), renin-angiotensin system inhibitors (losartan or lisinopril), fluoxetine, topical nitroglycerin, phosphodiesterase 5 inhibitors (PDE5i), endothelin receptor antagonists (ERA), prostaglandin analogs (PGA), and others (pentoxifylline, dipyridamole, and prazosin).
RESULTS
Overall, the study included 270 patients with SSc (approximately 83% diffuse), with a mean (standard deviation) symptom duration of 12.1 (10.6) years (30%; ≤5 years of symptoms) at enrolment. The median (interquartile range) follow-up was 3.4 (1.3–7.8) years in the cohort. During follow-up, 61% of patients used medication for RP, whilst 80% of patients received treatment for gastroesophageal reflux (p<0.001). The most frequently chosen group was CCBs (48%), followed by renin-angiotensin system inhibitors. About 13% and 20% of patients received RP-worsening medications while receiving or not receiving medications for RP, respectively. Advanced therapies such as PDE5i, ERA, and PGA were utilized in only 15% of the patients. The maintenance rate of RP medications was unfortunately low, and only approximately 29% of the patients remained on medications for RP throughout their follow-up.
While patients who had hypertension or who were on immunomodulatory medications were more likely to be on RP medications, patients who were at higher risk for worse vascular outcomes (such as those with early disease (≤2 years), current smokers, or patients who were Black) were less likely to be on RP medications (Figure 1A).
When looking at the medication choices from 2000–2023, CCBs remained stably the most common RP medication prescribed. However, PDE5i use has been increasing since 2019 despite remaining <10% overall (Figure 1B).
Lastly, the RP medication use based on US climate zones showed that RP medications were used more frequently in warmer climate zones like the West or Southwest US (Figure 1C), which could be driven by more frequent air conditioning use and rapid temperature changes.
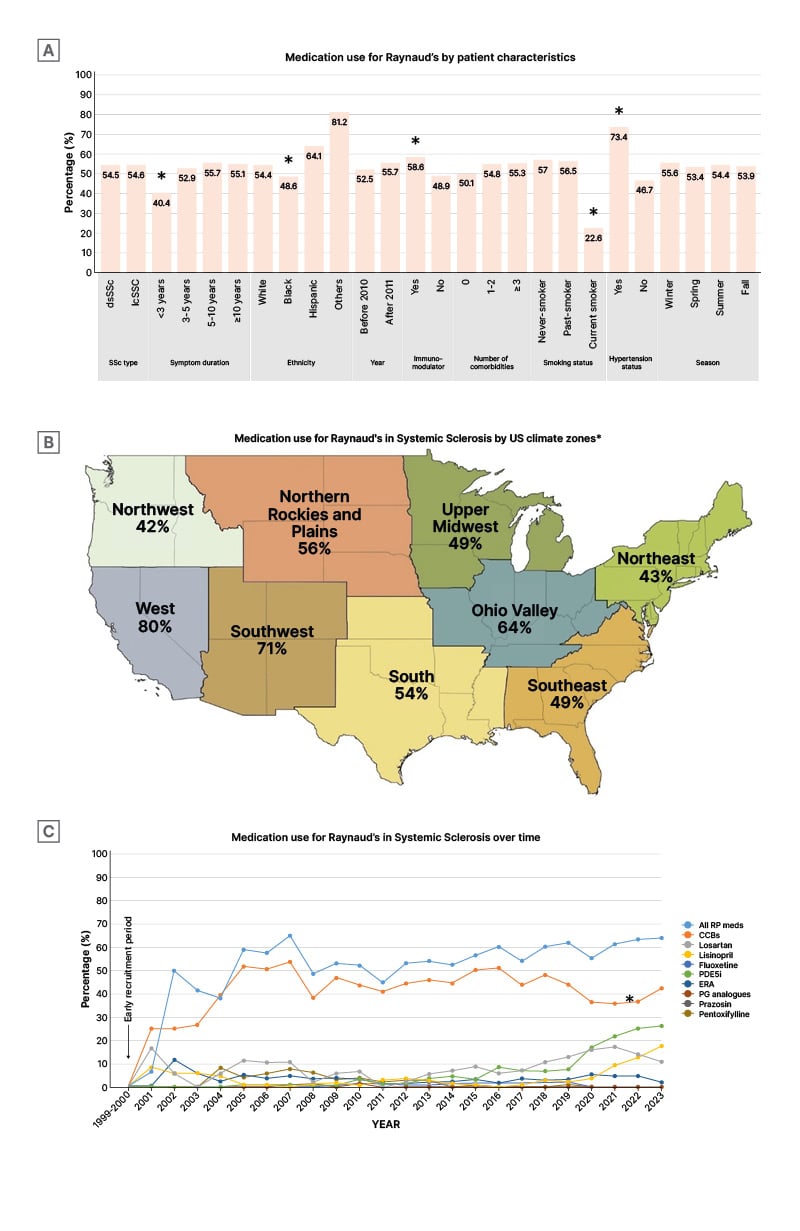
Figure 1: Medication use for patients with Raynaud’s phenomenon.
A) Medications for SSc-RP by patient characteristics. B) Frequency of RP medication use in SSc by US climate zones based. Adapted from National Centers for Environmental Information.2 C) Medication use for SSc-RP by type over time.
*p<0.05.
CCB: calcium channel blockers; ERA: endothelin receptor antagonists; PDE5i: phosphodiesterase 5 inhibitors; PG: prostaglandin; RP: Raynaud’s phenomenon; SSc: systemic sclerosis.
CONCLUSION
These findings suggest that, although CCBs are commonly used for SSc-RP among community-based rheumatology practices, overall SSc-RP management appears neglected (even worse than gastroesophageal reflux disease management) with low maintenance rates, low advanced therapy use rates, and significant concomitant use of RP-worsening medications. The increase in PDE5i use beginning in 2019, and corresponding to generic PDE5i availability, provides face validity to this real-world data. Besides FDA non-approval of advanced therapies (PDE5i, ERA, or PGA) for SSc-RP or its complications, lack of experience and guidelines for the management of SSc-RP and its complications play a significant role in the care gap of SSc-vasculopathy in community-based rheumatology practices. More education is needed to improve outcomes in SSc, especially in the setting of workforce deficits in rheumatology.







