BACKGROUND AND AIM
Patients with axial spondyloarthritis (axSpA) who are more physically active experience less pain and better physical functioning.1 It is also known that psychological factors such as anxiety and depression are associated with physical functioning and reduction of quality of life (QoL).2 Furthermore, evasive coping strategies are commonly used in health-related coping.4 However, to the best of the authors’ knowledge, no data are available regarding the influence of coping strategies, anxiety, and depression on daily physical activity in axSpA. The aim of this study was to determine if coping strategies, anxiety, and depression are associated with daily physical activity in patients with axSpA.
MATERIALS AND METHODS
Consecutive outpatients from the Groningen Leeuwarden AxSpA cohort (GLAS) participated in this study. In addition to the standardised follow-up assessments, patients completed the axSpA-Short Questionnaire to Assess Health-enhancing physical activity (axSpA-SQUASH), the Coping with Rheumatic Stressors (CORS), and the Hospital Anxiety and Depression Scale (HADS). Univariate and multivariate linear regression analyses were performed to explore associations of copings strategies, anxiety, and depression, and patient- and disease-related factors with daily physical activity. Additionally, patients were stratified into three tertiles of physical activity: low, intermediate, and high. To identify group differences, the Kruskal–Wallis or chi-square test were used with post hoc testing.
RESULTS
In total 85 patients were included; 59% were male, the mean age was 49±14, the median symptom duration was 19.5 years (interquartile range (IQR): 12.0–31.0), 71% were human leukocyte antigen-B27 positive, and the mean Ankylosing Spondylitis Disease Activity Score (ASDAS) was 2.1 (standard deviation: 1.0). (Table 1). Median axSpA-SQUASH total physical activity score was 9,406.3 (IQR: 5,538.8–12,081.3). Scores of HADS-Anxiety (scale 7-28) and HADS-Depression (scale 7-28) had median scores of 5.0 (IQR: 3.0–7.0) and of 3.0 (IQR: 2.0–5.5). The most used coping strategies was comforting cognitions (for pain; range: 9–36) with a median of 25.5 (IQR: 22.0–28.0).
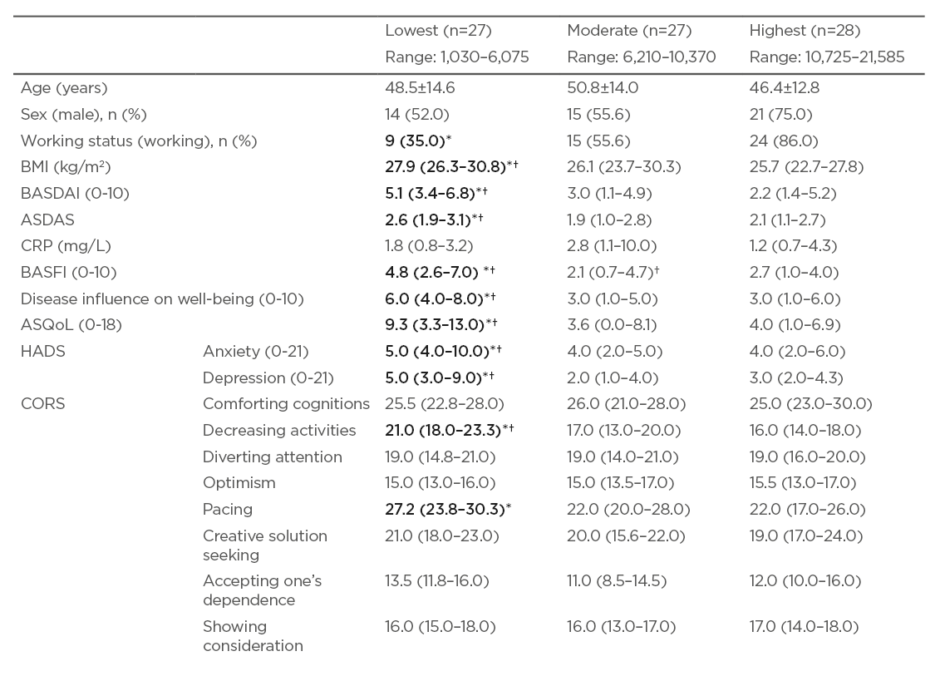
Table 1: Differences between the low-, intermediate-, and high-physical activity tertiles.
Data presented as number of patients (%), mean ± standard deviation, or median (interquartile range).
* p≤0.05 for highest group compared to lowest group.
† p≤0.05 for intermediate physical activity group compared to lowest physical activity group.
ASQoL: Ankylosing Spondylitis Quality of Life; ASDAS: Ankylosing Spondylitis Disease Activity Score; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; BASFI: Bath Ankylosing Spondylitis Functional Index; CORS: Coping with Rheumatic Stressors; CRP: C-reactive protein; HADS: Hospital Anxiety and Depression Scale.
Univariate analysis showed that lower daily physical activity was significantly associated with female sex, higher disease activity (Bath Ankylosing Spondylitis Disease Activity Index [BASDAI]), worse physical function (Bath Ankylosing Spondylitis Functional Index [BASFI]), worse QoL (Ankylosing Spondylitis Quality of Life [ASQoL]), coping strategies such as ‘decreasing activities’ and ‘pacing’, higher depression score (HADS), and higher perceived influence of axSpA on general well-being. In the multivariate linear regression model, the coping strategy of decreasing activities (β: -376.4; 95% confidence interval: -621.9 to -130.8; p=0.003) and BMI (β: -235.5; 95% confidence interval: -450.9 to -20.0; p=0.03) were independently associated with physical activity. The multivariate model explained 22% of variance (R2: 0.2197; p=0.001). Additionally, patients in the highest physical activity tertile were significantly more often male, had higher working status, lower BASDAI and ASDAS, better BASFI and ASQoL, and scored lower on the coping strategy of decreasing activities.
CONCLUSIONS
In this cross-sectional study in patients with established axSpA disease, multiple patient- and disease-related factors were associated with daily physical activity. The evasive coping strategy of decreasing activities and BMI were independently associated with the level of physical activity. These findings suggest that to improve daily physical activity in patients with axSpA, attention should be paid not only to targeting disease activity, but also to other patient- and disease-related aspects, especially coping strategies used.








