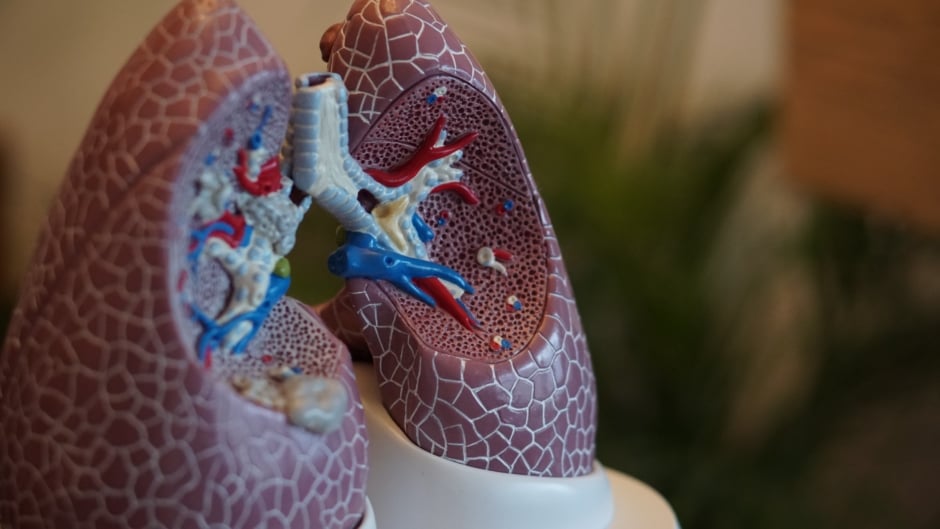
COVID-19 has been shown to significantly affect the lungs. To understand how the immune cells of the lung respond to viral infection, researchers at the Salk Institute, San Diego, California, USA have conducted a study with the hope of aiding scientists in the development of a vaccine.
Upon first exposure to a bacteria or virus, the immune-mediated killer T cells target and destroy the infected cells and thereby prevent the spread of the disease. Cleverly, T memory cells are retained in the body after the pathogen’s removal, which enables the body to rapidly respond to a second attack if the invading bacteria or virus should attempt to infect the body again. This is a fundamental concept behind vaccination but studies that analyse killer memory T cells specifically in the lung are lacking.
Prof Susan Kaech led the team of researchers at the Salk Institute where they studied various types of messenger cells in mice to determine whether killer memory T cells would recognise a second influenza infection. Surprisingly, the team found that the experienced T cells continued to recognise the virus without the aid of many different messenger cell types. By not being reliant on any single type of messenger cell, the T cells could identify the virus through various messenger cells, even nonimmune cells such as lung epithelial cells.
Contrastingly, the lymph nodes’ killer memory T cells were found to rely on dendritic cells to recognise a second viral attack. This challenges the notion that anatomical location of the experienced T cells does not dictate the way in which they are activated.
Ready to apply this information further afield, Prof Kaech stated: “We will take this knowledge into our next study, where we will examine whether lung-resident killer memory T cells form after a coronavirus infection.”