Abstract
Background: Persistent cough is one of the most common conditions affecting quality of life. The aim of this study was to assess people’s beliefs regarding the impact of, and changes in the prevalence of, persistent cough in the Italian general population over a 10-year time period.
Methods: Two telephone surveys were conducted in 2006 and 2015, and the answers were compared. In 2015, the same questionnaire was also randomly distributed in paper form to another cohort. Sample sizes were precalculated for their representativeness and comparability (Chi-square test).
Results: In total, 1,251 subjects in 2015 and 1,334 in 2006 completed the interviews. The corresponding completion rate for the interviews was 23.0% and 21.8%, respectively; 5,056 individuals completed the paper-form questionnaire. A substantial proportion of respondents stated that persistent cough should be regarded as a disease and not merely as a symptom. This belief increased from 38.8% to 46.4% (p<0.03) over the study decade. The prevalence of persistent cough recorded through computer-assisted telephone interview was 14.2% and 18.4% in the 2006 and 2015 surveys, respectively (p<0.02), and 35.5% in individuals answering the paper-form questionnaire (p<0.01). General practitioners (69.6%) and lung physicians (16.2%) were among the most frequently consulted medical professionals for cough. The majority of respondents disagreed with first-line antibiotic and/or systemic steroid use, while antitussive drugs and mucolytics were highly valued. The willingness of the patient to pay for their own treatment increased, with >40% of responders willing to pay >€10 at the pharmacy in 2015.
Conclusion: These surveys showed the prevalence of persistent cough is increasing, together with the willingness of the patient to pay out of their own pocket for treatment. However, the methodology for data collection should be carefully considered before data are generalised.
INTRODUCTION
Persistent cough is one of the most frequent respiratory symptoms causing patients to seek a medical consultation worldwide; thus, the condition represents a true challenge in daily practice.1 Acute cough (cough lasting for <3 weeks) is often due to the common cold or upper respiratory tract infections and, in the vast majority of cases, results in life-limiting effects in the absence of significant comorbidities. Chronic cough (cough lasting >8 weeks) has several different causes.2-4
Persistent cough, which is a cough lasting 3–8 weeks or longer,5 represents a grey area that is difficult to define because it can have an aetiology similar to that of acute or chronic cough.2 The most frequent causes of persistent cough include bronchial asthma, tobacco smoking, inhalation of pollutants and environmental irritants, gastro-oesophageal reflux disease, post-nasal drip, and the use of some antihypertensive drugs.2-4 Other possible causes include subacute infections, airway cancer, mediastinal occupation of different aetiology, chronic bronchitis, chronic obstructive pulmonary disease, bronchiectasis, foreign bodies, cystic fibrosis, lung fibrosis, extrathoracic causes, obstructive sleep apnoea, laryngeal dysfunction, and psychological disorders.4-17
While the impact of persistent cough on a patient’s life ranges from minimal discomfort to disabling symptoms, physical impairment is a frequent complication of the condition, together with depression, school or work absenteeism, and a substantial economic burden.18-20 The prevalence of persistent cough has been estimated in different international studies and ranges from 11–18%, with higher values reported in Europe than in the USA.21-24 The impact of persistent cough was specifically assessed in episodic studies,18,21,24 but, to the authors’ knowledge, the prevalence of persistent cough has not been investigated in Italy to date.
AIM
The aim of this study was to assess and compare the prevalence and the impact of persistent cough among Italian adults from the general population over a 10-year time period and to monitor the beliefs of the patients regarding the condition. The parallel use of a paper-form questionnaire and a telephone survey was to compare the characteristics of responses from respondents reached by the two different tools of investigation.
METHODS
A cross-sectional telephone survey was conducted between 21st and 29th July 2015 in individuals aged ≥18 years. The results of this 2015 survey were compared to the results from an identical survey carried out between July 17th and 25th July 2006.
The investigational tool for collecting data was the same validated, anonymous questionnaire consisting of 20 predetermined questions on cough: 16 of the 20 questions were closed (80.0%), while Questions 5, 6, 16, and 20 were open questions (Box 1).
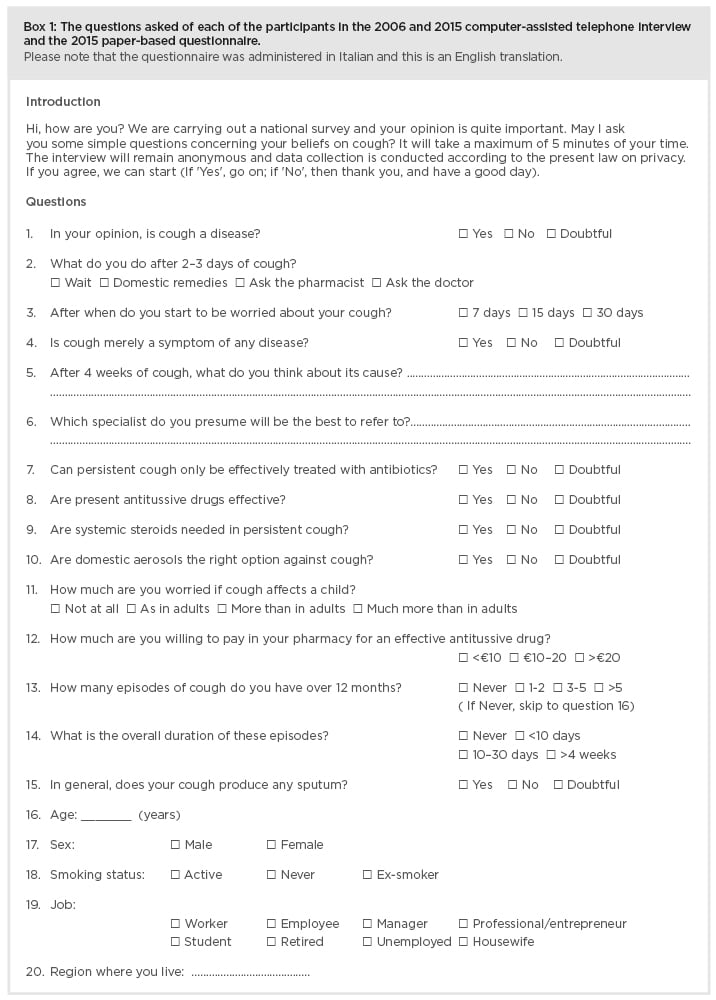
Box 1: The questions asked of each of the participants in the 2006 and 2015 computer-assisted telephone interview and the 2015 paper-based questionnaire.
Please note that the questionnaire was administered in Italian and this is an English translation.
Possible answers for closed Questions were ‘Yes’, ‘No’, and ‘Doubtful’. For Questions 5 and 6, respondents had to indicate their own opinion, while Questions 16 and 20 asked the patients for their age (in years) and the region where they lived, respectively. According to consolidated validation procedures, the original version of the questionnaire was previously given to a sample of 25 randomly selected individuals with varying educational levels (the usual sample size for a pilot test) to check the comprehension of the questions included. When linguistic errors and/or misunderstandings occurred, the corresponding items were reworded until full comprehension was obtained.25
In both editions of the survey, all interviews were performed according to the computer-assisted telephone interview (CATI) methodology26 by the same agency of professional interviewers. The distributions of all answers were calculated in the overall samples. The interviewers were provided with one work station consisting of a personal computer connected to a central processing unit. The central unit was also equipped with specific software for the random selection of individuals to contact. Compared to a conventional telephone interview, the CATI technique allowed the randomisation of question order. Moreover, this system worked as a supervisor of the interviewer’s activity: if the interviewer forgot some questions or even an entire section of the questionnaire, the software would alert them, thus avoiding errors due to missed questions.
As previously mentioned, the sampling strategy adopted in the present survey was the computerised random selection of an adequate number of subjects from the national pool of home and mobile telephone numbers. A minimum number of 1,226 respondents in 2006 and 1,178 respondents in 2015 were required to achieve an accurate representation of the Italian population in terms of age, sex, education, smoking habit, and geographical distribution (by 3% maximum error and 95% probability).
A short explanation, with a mean duration of 5 minutes, concerning the aim of the survey preceded all interviews. Interviews were only conducted after having recorded the respondent’s informed consent to the interview itself and to the possible use of their information for scientific purposes.
In 2015, the same questionnaire was randomly distributed in a self-managed, anonymous paper form to individuals from the general population. A minimum of 5,010 respondents were required to achieve representativeness of the general population (by 3% maximum error and 95% probability). maximise the national distribution and completion rate, the National Centre for Respiratory Pharmacoeconomics and Pharmacoepidemiology (CESFAR) and the Italian Cough Association (AIST) involved their affiliate members actively in the distribution and collection of the questionnaires across Italy. The organisations also shipped the questionnaires to the operational centre for calculations.
In the present paper, only data concerning persistent cough were considered, reported as frequencies. Statistical comparisons were calculated by a Chi-squared test, and p<0.05 was assumed the minimum level of statistical significance. Each survey was approved by the CESFAR Ethical Committee, Verona, Italy, in 2005 and 2016, and all subjects were required to provide their informed consent to the interview before participating.
RESULTS
A total of 1,251 individuals (mean age: 49.0 years; 44.2% females) completed the interview in 2015, while 1,334 individuals (mean age: 47.8 years; 43.7% females) took part in 2006. The overall telephone contacts were 5,362 and 6,109 in 2015 and 2006, respectively. The corresponding interview completion rate (e.g., the proportion of calls properly completed and providing reliable data for the investigation) was 1 in every 4.3 calls (23.3%) in 2015, and 1 in every 4.6 calls (21.8%) in 2006. A total of 5,056 paper-form questionnaires were also collected. The data that characterise the respondents from the two telephone surveys and the paper survey are reported in Table 1. The data proved comparable over the 10-year period and equally representative of the general population.
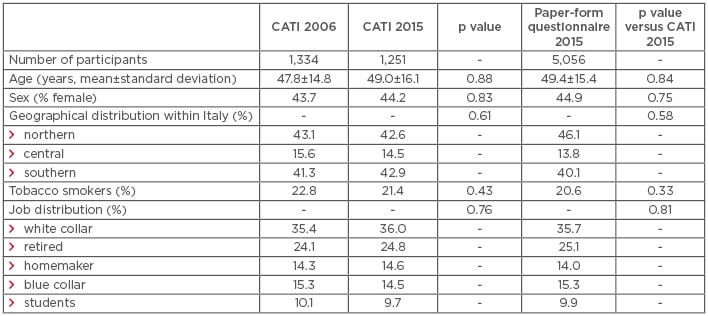
Table 1: General characteristics of the 2006 and 2015 cohorts investigated via computer-assisted telephone interview, and of the 2015 cohort investigated via paper-form questionnaire.
Dashed boxes indicate where data are not applicable. CATI: computer-assisted telephone interview.
The questions included in the questionnaire were originally divided according to five main sections: basic opinion on cough, the general impact of cough on life, approach to cough, therapeutic expectations, and willingness to pay for treatment.
Respondents’ Basic Beliefs
The majority of respondents in both surveys had the opinion that cough should be considered a symptom of several diseases, but 46.4% of respondents in 2015 and 38.8% in 2006 claimed that persistent cough should be regarded as a disease. This proportion increased significantly over the 10 year time period (p<0.03). Moreover, the number of survey non-responders dropped by >50% over the same period (p<0.01). Data from the 2015 paper-form questionnaire showed different results to the 2015 CATI, such as a lower belief of cough as a disease (36.6%, similar to that seen in the 2006 CATI survey) (p<0.02) and a much higher proportion of non-responders (p<0.01) (Figure 1A).
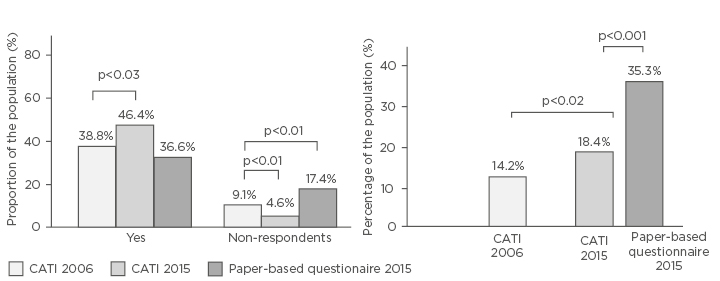
Figure 1: A) The proportion of respondents perceiving persistent cough as a disease. B) Prevalence of persistent cough (lasting >4 weeks) identified by the three surveys.
CATI: computer-assisted telephone interview.
General Clinical Impact
The prevalence of persistent cough was 18.4% in 2015 and 14.2% in 2006 (p<0.02), and increased to 35.5% among respondents to the 2015 paper-form questionnaire (p<0.01) (Figure 1B). Productive cough was consistently slightly more frequent than persistent cough: 55.9% in the 2015 CATI; 58.8% in the 2006 CATI; and 57.1% when data were collected via the 2015 questionnaire paper-form. The majority of respondents (71.7%) started to worry about their own cough 1 week after cough initiation, while a greater number of respondents (76.9%) stated that they were much more concerned when persistent cough affected a child.
Respondents’ Approach to Cough
General practitioners (69.6%), lung physicians (16.2%), and otorhinolaryngologists (10.6%) were consulted most often following the initiation of persistent cough. Moreover, chronic airway disease (48.2%), pneumonia (25.7%), persistent allergic troubles (7.8%), and cancer (2.3%) were the four most feared causes of persistent cough.
Respondents’ Therapeutic Expectations
The majority of respondents stated that antibiotics are not the only effective treatment for persistent cough and that steroids were not needed in the treatment of persistent cough (56.4% and 51.6% in 2006, and 61.2% and 58.2% in 2015, respectively), while antitussive drugs were generally perceived as an effective option. Data from the 2015 paper-form questionnaire further confirmed these beliefs (62.8% concerning antibiotic use, 60.1% concerning steroid use, and 68.6% concerning the perceived therapeutic value of antitussive drugs).
Willingness to Pay
The willingness of a patient to pay out of their own pocket for their treatment increased significantly over the 10-year survey. While 63.4% of respondents agreed to pay up to €10, 26.8% up to €20, and 1.0% >€20 for an effective antitussive remedy in 2006 (8.8% non-responders), the corresponding willingness to pay in the 2015 CATI was 46.3% up to €10, 27.8% up to €20, and 13.3% >€20 (12.6% non-responders). The willingness to pay out of their own pocket proved even higher when calculated via the 2015 paper-form questionnaire: 20.7% up to €10; 51.5% up to €20, and 27.8% >€20. The role of inflation was considered. Under the assumption of gamma distribution, the mean willingness of patients to pay out of their own pocket was €8.51 in 2006 and €14.01 in 2015 (also including the results of the paper-form questionnaire). As the willingness to pay in 2006 cannot be compared directly with that of 2015 due to inflation, it was inflated to 2015 applying a discount rate of 1.235 (Harmonised Indices of Consumer Prices).27 Taking this correction for inflation into account, the willingness to pay out of pocket was still considerably higher in 2015 than in 2006 (€14.01 and €10.51, respectively).
DISCUSSION
Persistent cough is one of the most frequent events reported in respiratory medicine; nevertheless, its impact remains difficult to define in real life. The beliefs of the general public do not always fit the aetiology or the severity of cough, and subjects tend to be equally worried about their cough even if it is not disabling, particularly when long-lasting. From this point of view, the widespread lack of specific knowledge19 is a contributing factor to these beliefs. On the other hand, only 50% of patients with persistent cough receive a diagnosis and care.18,26
Despite the consolidated belief that cough represents a non-specific symptom shared by several diseases, >38% of respondents in 2006 and >46% of respondents in 2015 believed that persistent cough may represent a disease. This opinion increased significantly over the 10-year period, in parallel with a substantial drop in non-respondents or doubtful subjects. This unexpected result is particularly interesting because it corresponds to the recent scientific view on cough, which regards persistent cough as the clinical effect of a cough hypersensitivity syndrome, such as a condition due to the exalted status of airway sensory nerves occurring independently of the aetiology of cough.28,29 It is highly presumable that the vast majority of the public were unaware of this scientific view of cough by experts.
Persistent cough showed a significantly elevated prevalence in the general population over the 10-year interval between the two phone surveys (14.2% in 2006 versus 18.4% in 2015; p<0.02), by an increase of 29.6%. Although these data may be biased by the method for collecting data and may overstate the true prevalence of persistent cough, they are in general agreement with other European and extra-European studies on the global epidemiology of chronic cough in adults.21-24,26,30-32
Despite the good concordance of the CATI surveys, the proportion of respondents to the 2015 paper-form questionnaire who agreed with the hypothesis of cough being a disease was much lower, while the prevalence of persistent cough (35.3%) was much higher compared to the CATI interview results (18.4%). These large differences are likely due to the different methods for collecting data. In other words, even if comparable for age, sex, and national distribution, it is probable that the CATI responders operated in a different setting (with a more limited time for their responses) than those individuals who completed the paper-form questionnaire, meaning that their psychological approach to the questions was different.
The results of the study emphasise that the prevalence of persistent cough increased significantly over the 10-year study period in Italy, independently of the method adopted for the survey. Environmental conditions have contributed progressively to cough development over the same period in Western countries,32 including Italy,33 due to uncontrolled urbanisation and exposure to industrial, occupational, and traffic irritants. These factors support and explain the increasing prevalence of persistent cough observed during the last decade in Italy.
The effective treatment of persistent cough still represents a critical issue in many cases. With this in mind, a further interesting result was revealed from analysis of the beliefs of the respondents regarding the therapeutic approach to persistent cough. The majority of respondents disagreed with the first-line use of antibiotics and/or systemic steroids for managing persistent cough. Consequently, the general population, even if generally unaware, seem to share the same opinion of the most updated scientific community.28,29 Nevertheless, despite this widespread belief, the prescription of antibiotics and/or systemic steroids still remains diffuse and consolidated in Italy, even if not recommended by national and international evidence.3,33-35 However, it is important to note that around 40% of respondents were convinced of the primary role of antibiotics and steroids in the treatment of cough.
The attitude in favour of symptomatic drugs proved high within the Italian general population. Antitussives and mucolytics were confirmed as the most preferred and used drugs among the over-the-counter medications, either for self-medication or for regular prescription after a medical consult. If easy accessibility contributes to the widespread use of over-the-counter products, other factors can influence the high prescribing rates of antibiotics and steroids: doctors’ uncertainty on the causes of persistent cough, which are infrequently investigated in clinical practice; patients’ expectations (increasingly supported by the widespread attitude to the self-research for medical information via social media);36,37 the shifting doctor–patient relationship;38 and the ever-increasing role of defensive medicine.
According to the literature,3,4 a significant component of the cost of persistent cough is related to work or school absenteeism; therefore, the authors also assume this to be the case in the present study. The general dissatisfaction for the present therapeutic approach to treatment of persistent cough is clearly mirrored by the progressively higher and ever-increasing willingness of patients to pay out of their own pocket to obtain effective antitussive remedies in the pharmacy. Over the 10-year time period, the general population’s attitude regarding spending on medication changed dramatically, independently of the method for data collecting (the phone survey rather than the paper-form questionnaire), and clearly shifted in favour of a higher level of personal, direct expenditure (2–3-fold higher) compared to the last decade.
The present study has limitations. Firstly, it was not designed to define the aetiology of persistent cough, but instead focus on the overall crude prevalence of persistent cough in the general population. Secondly, individuals were questioned with the same questionnaire but using two different methods, via phone contacts (data of 2015 compared to those of 2006) and via a self-administered paper-form questionnaire. This study trait should not solely be considered as a weakness because this parallel procedure proved that results may be dependent of and affected by the method adopted for investigation; how carefully should the results obtained be considered and how can their generalisation be at risk. Finally, the precise expenditure of patients for the treatment of persistent cough was not calculated, despite data on the willingness of patients to spend out-of-pocket emphasising that several patient needs are still unmet. Further studies are needed for investigating this particular issue more deeply.
CONCLUSION
A large proportion of individuals regarded persistent cough as a disease and not as a symptom common to several diseases. This proportion has increased significantly over the last decade in Italy. The prevalence of persistent cough increased significantly from 2006–2015, independently of the different method of investigation. Usually, subjects’ concerns tend to increase when their cough lasts for >1 week, while persistent cough in children is much more feared than in adults. The majority of Italians oppose the first-line use of both antibiotics and steroids for the treatment of persistent cough, while symptomatic antitussive drugs are highly valued within the general population. Finally, the willingness to pay for an effective antitussive remedy has increased over the last decade. Data collected via different methods (CATI versus the paper-form questionnaire) can affect the homogeneity of results, likely due to the uneven targeting of individuals participating in the surveys. This difference in data gathering methodology should, therefore, be carefully considered before data are generalised.








