Abstract
Recently, there have been enormous developments in the endoscopic management of central airway obstruction secondary to benign or malignant processes. Airway stents are an essential component of such management. They provide rapid relief to patients with central airway obstruction. However, like any other foreign object introduced into the body, airway stents have their own complications. These can range from benign, such as increased coughing, to fatal, due to massive haemorrhage. Placement of a stent is a temporary bridging therapy to allow the patient to undergo chemotherapy or radiotherapeutic management. Airway stents should not be left in situ for long, as they themselves can become a disease in patients who already have life-limiting diseases. Hence, the motto at our centre is ‘no stent left behind’, with the only caveat being that they are left behind when the removal itself could cause death. In this paper, we will review the recent literature covering the removal of airway stents. We also describe our experience with airway stents removal. We conclude that efforts should be made to remove all airway stents when the primary disease is controlled. No stent left behind!
INTRODUCTION
Over the last few decades, there has been enormous development in the endoscopic management of central airway obstruction secondary to benign or malignant conditions.1 Airway stents have become an integral part of the endoscopic management of inoperable conditions causing central airway obstruction.2,3 They are specifically designed to mimic the airway, in order to restore patency.4
Previous reports have described certain features of an ideal airway stent: re-establish the airway; minimal morbidity and mortality; limited migration, while being easily removable if necessary; maintain luminal patency without causing ischaemia or erosion into adjacent structures; minimal granulation tissue (GT) formation; easy to place; and affordable.5,6 Unfortunately, the perfect stent has yet to be found; every stent available has its own advantages and disadvantages. Similar to any device introduced into the body, stents have their own complications and indications to be removed.7 Due to an increase in the use of stents, in 2005 the U.S. Food and Drug Administration (FDA) published an advisory on the use of metallic stents in patients with benign airway diseases.8 The advisory clearly recommended that in patients with benign airway compression, self-expandable metallic stents (SEMAS) should only be used after thoroughly exploring all other treatment options and the insertion and removal of SEMAS, if this is the only option available, should be done by a physician trained or experienced in metallic tracheal stent procedures. The stent of choice for these patients continues to be silicone stents.
Removal of stents is not without complications. There are reports of hospitalisations and intensive care unit admissions in 78% and 39% airway stent removal cases, respectively. The estimated median total cost per stent removal in the same study was $10,700 (range: $3,700–69,800).8 This paper reviews the recent literature for the removal of airway stents. As there are numerous reviews on stent insertion, they will not be discussed in this paper.5,9 We also describe our experience with airway stent removal.
METHODOLOGY
A search on PubMed and Google Scholar was performed in November 2016, using the keywords ‘airway stents’, ‘tracheobronchial stent’, and ‘stent removal’. Relevant articles were reviewed from 1990 until November 2016. There were 42 articles published that discussed airway stents. Eight were excluded as they discussed surgical removal and reconstruction of the tracheobronchial tree.
At our centre, we use partially and fully covered stents, as well as silicone stents. Table 1 outlines our experience with stents, and Figure 1 outlines our protocol for the evaluation for stent placement and its subsequent removal. We recently removed a tracheal stent from a patient that was inserted 26 years ago for trauma-related tracheomalacia and resulted in obstruction of the trachea with GT (Figure 2A and 2B). Figure 3 shows a CT scan image of a patient before and after stent removal. Figure 4 depicts a migrated stent.
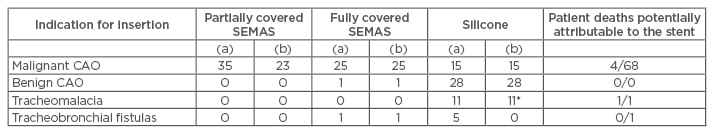
Table 1: Our overall experience with airway stents.
(a) Deployed; (b) Removed; (*) Removed and replaced.
CAO: central airway obstruction; SEMAS: self-expandable metallic stents.
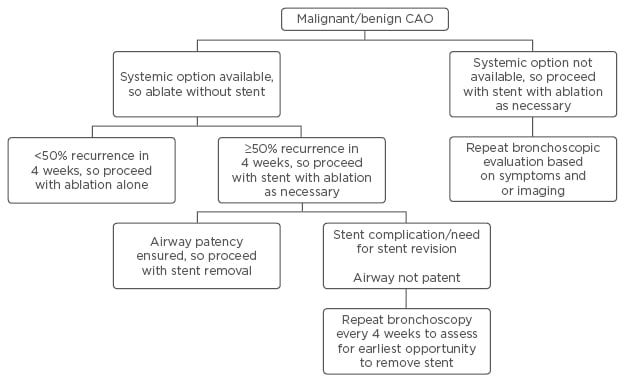
Figure 1: Our approach to central airway obstruction.
CAO: central airway obstruction.
Figure 2: Silicone stent.
A) The silicone stent is almost completely occluded with granulation tissue at the site of tethering suture. The stent was present within the patient for 26 years. B) The silicone stent ex vivo. The stent fragmented upon removal (to our knowledge, at 26 years this is the longest a stent has remained within a patient).
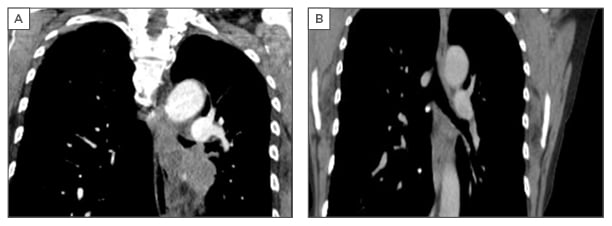
Figure 3: A) Computed tomography scan image showing recurrent obstruction secondary to adenocarcinoma of the lung. B) Computed tomography scan image after stent removal, after 4 months on erlotinib treatment.

Figure 4: A bronchoscopic image demonstrating a migrated, partially covered SEMAS obstructing the left main bronchus.
SEMAS: self-expandable metallic stent.
INDICATIONS FOR STENTS REMOVAL
As use of airway stents gains popularity, complications are subsequently becoming more frequent.6 Removal of stents is considered when they are either not necessary or a major complication is imminent. Incidences of complications vary widely, from 13–72% in various reports.10,11 The complications are related to stent type, location of stenosis, and type of stenosis. Chhajed et al.12 showed that patients who develop tracheobronchial stenosis after pulmonary transplantation had reduced survival rates in the event of tracheobronchial stent complications. Certain complications occur more frequently in one type of stent compared to others. For example, SEMAS are associated with higher rates of GT formation, stent fracture, erosion into adjacent structures, and bacterial colonisation compared to other types of stents.8,13-15
COMMON COMPLICATIONS SECONDARY TO AIRWAY STENTS
Migration
Migration is one of the most common complications associated with stents.6 Silicone stents are more likely to migrate than metal stents and can even be expelled from the airway. This complication can be explained by the nature of the stent. Silicone stents usually maintain their predetermined shape and diameter, whereas metal stents expand to fit the airway when deployed.6,16
Granulation tissue
Formation of GT is more likely to form at the proximal and distal end of a stent and, in severe cases, granulation can cause in-stent stenosis (Figure 2).17 In addition to causing obstruction, GT can serve as a nidus for bacterial growth.18 In a study conducted by Wang et al.,19 granuloma formation was found to be the most common complication of both covered metallic stents (CMS) and uncovered metallic stents (UCMS). It was also noted that the location of GT was different between the two groups. GT was common at the end of CMS, whereas it occurred as an in-growth in UCMS.19
Impaired Mucociliary Function
Similar to GT, lack of mucociliary clearance can lead to obstruction and infection of the stent. Unlike plastic stents, metallic stents permit mucosalisation through their interstices, which could preserve mucociliary function.20,21
Stent Fracture
Although stent fractures are an uncommon complication, when they do occur it is usually with metal stents. Stent breakage requires urgent removal to minimise the upper airway effects of stent collapse and subsequent distal fragmentation of metallic pieces.6,16
Patient Intolerance
Some patients do not tolerate long-term stent placement. Stiff, longer stents are not as well tolerated as short, flexible, compliant stents. In addition, proximally placed stents are not as well tolerated as distal trachea-bronchial stents.6 We once managed a patient who had a hybrid Y stent placed for tracheobronchomalacia with marked airway narrowing; the patient’s stent had to be removed the same day, as they could not tolerate the stent in situ and had suffered a persistent cough.
Haemoptysis
Balloon-expandable metal stents are more likely to erode the tracheobronchial tree and lacerate major blood vessels if they over-expand, or have a shear force that is being exerted at the bronchial wall.22
Another indication for stent removal is when it is no longer required. In a study performed by Wang et al.,19 35% of the CMS and 16.7% of the UCMS were removed when they had achieved their goal of allowing for therapy.19 In a separate series, it was reported that 21 of 48 prosthesis removals were justified by an apparent cure.23 However, Buiret et al.24 only reported two removals that were justified by an apparent resolution of the stenosis.
PREDICTORS OF STENTS REMOVAL
Buiret et al.24 performed a broad study evaluating several stent brands. It was found that the only significant predictive factor for prosthesis removal was the brand of the prosthesis.24 Contrary to the study by Saad et al.,25 this finding was independent of the benign or malignant nature and precise cause of the stenosis, and independent of the type of prosthesis (for example, non-expandable, expandable covered, or uncovered). Buiret et al.24 reported the stability of each separate brand of prosthesis (the hazard ratio [HR] represents the probability of maintenance of the prosthesis): Ultraflex (HR: 1), covered Wallstent (HR: 2.496), Cook (HR: 8.701), Hanarostent (HR: 9.372), Aboulker (HR: 10.424), Tracheobronxane (HR: 10.626), Novatech Silmet (HR: 17.750), uncovered Wallstent (HR: 57.8), Novatech Y (HR: 88.268), and Rush Y (HR: 122.902).24
Dasgupta et al.26 assessed 37 patients and reported that the longer a patient has an airway stent fitted, the greater the risk of complications. They noted a complication rate of 0.06 per patient month, with 19 complications in 318 months. Most of the complications encountered in the series were obstructive granulomas and non-obstructing GT (two patients).
TECHNIQUES AND CHOICE OF ANAESTHESIA IN STENT REMOVAL
Three basic steps have been described to remove a stent: a) assessing degree of incorporation, b) freeing the stent from the mucosa, and c) removing the stent from the airway.1 Nashef et al.27 reported their experience in removing four Gianturco stents and described the procedure as “…similar to that of rolling spaghetti on a fork, but much more difficult and at least equally messy.”
At our institute, we place silicone tracheobronchial stents, hybrid and silicone Y stents, and fully covered and partially covered SEMAS. After placement, as per Figure 1, we perform routine surveys of the airways with flexible bronchoscopy every 4–6 weeks, based on patient comfort and factors that may impact scheduling. The stents are evaluated for the presence of any criteria for removal, be it a complication or resolution of the disease that required a stent. Once the decision is made to remove, we plan the removal based on the difficulty level, judged by the stent and airway interphase.
Simple Removals
When the stent is fairly free in the airway or a ‘floating stent’, we intubate with the rigid bronchoscopy and grasp-roll-remove the stent. We re-intubate to clean the debris and determine that the patient does not need another stent. These removals have not been associated with any complication. Silicone stents and fully covered SEMAS are usually easy to remove.
Moderately Difficult Removals
These are usually partially covered stents.
- If the stent appears to have a significant ingrowth with GT, we treat the GT with cryo-therapy or heat ablative therapy (argon plasma coagulation or laser). This reduces the stent incorporation into the airway wall, making them easier to remove.
- If the stent’s edge could potentially cause airway injury, we slide the bevel of the rigid scope gently between the stent and the airway and remove. If injury occurs, we place a silicone stent across the breach and remove it in 2 weeks.
- Development of a tracheaoesophageal fistula has occurred once and was treated via removal of the offending stent, and replacement with a Y silicone stent.
Extremely Difficult Removals
These always occur with UCMS. We do not place them within our institute but have had referrals for incorporated stent removals. These stents should only be approached with multidisciplinary planning, including radiologic and bronchoscopic evaluation, in concert with cardiothoracic surgery backup. The stents have to be removed in a piecemeal fashion, with short segments removed at a time. Bleeding usually occurs and can lead to a breach in the airway or vascular system that may require emergent thoracic surgery. For indications that require a bare metal stent placement, the removal should be within 2 weeks.
Removal Based on Stent Types
Silicone stents
These tend to be the easiest to remove. We grasp the proximal end, roll the stent with the forceps, and then pull the stent out.
Self-expandable metallic stents
- Fully covered: these are reliably easy to remove, similar to the silicone stents. We use the same technique; the proximal end is grasped, the stent rolled, and then pulled through, using a rigid bronchoscope.
- Partially covered: these tend to be a little more difficult to remove after the first 28 days. However, we evaluate the stents every 4–6 weeks until the need for the stent is resolved. Once the decision is made to remove the stent, it is done either in a one-step method, for partially covered SEMAS that are free from any significant GT, or endothelialisation. Alternatively, if there is significant GT involvement of the uncovered part of the stent, we treat the GT with cryotherapy or ablation and then reevaluate within a week. We have been able to remove all but one stent completely intact when using the two-step method. For the one case where this was not possible, the distal end of the stent was unravelled, and took multiple attempts to remove all wires from the airway.
We recommend all stents be removed in operative rooms under general anaesthesia; any other site places the patient under undue risk. We have not yet had to admit or observe any of our stent removals ≥2 hours post operation. No major complications have been noted after the removal at our institution.
COMPLICATIONS OF STENT REMOVAL
Complications of stent removal include bleeding, mucosal tears with or without bleeding, re-obstruction requiring new stent placement, GT behind the stent, damage to the bronchoscope, damage to the pulmonary artery, pneumothorax, postoperative mechanical ventilation, retained stent pieces and unsuccessful removal, and death.1 In a retrospective analysis performed in 43 patients with 47 tracheobronchial stents, Wang et al.28 reported two major post-removal complications: profuse haemorrhage (n=4) and mucosal tear (n=15). In a report by Kao et al.,29 a critical airway obstruction occurred during the removal of a welded tracheal stent using rigid bronchoscopy, which required urgent use of cardiopulmonary bypass. The remaining pieces of the stents were removed successfully by directly opening the trachea.
FACTORS PREDICTING STENT REMOVAL-RELATED COMPLICATIONS
Many authors reported factors that predict complications of the stent removal. Murgu et al.30 reported three factors that can predict post-removal complications: type of stent, duration of indwelling stent, and initial indication for stent placement. Such data is important as it could prepare the physician for the complications. The type of stent was studied and was found to have prognostic significance in stent removal complications. Uncovered SEMAS have a higher removal complication rate than covered ones, due to tumour ingrowth, GT, or endothelialisation.30 Reports by Wang et al.28 and Chan et al.31 revealed a higher failure rate with uncovered versus covered stents. Wang et al.28 reported that the proportion of failed removal was 2.8-times higher for uncovered SEMAS than for covered SEMAS. Stent fracture during removal is more common with uncovered SEMAS, possibly due to stent embedding and/or GT.28
Duration of indwelling stent is another predictor of stent removal-related complications.8,30,32 Alazemi et al.8 noted no major complications in SEMAS that were removed within 30 days of insertion. A similar trend was observed by Thornton et al.33 Although only two patients (5%) in their series required additional therapeutic interventions within 30 days after their SEMAS placement, 15 patients (38%) developed significant complications after 30 days (mechanical stent failure and stent obstruction) requiring additional intervention. While Lunn et al.32 found that complications related to SEMAS removal increased for every additional month they had been in place, Shah et al.34 did not find a relation between the development of complications and length of stent placement.
Initial indication for stent placement can also predict post-removal complications. Patients who had their SEMAS initially placed for underlying benign diseases were more likely to experience complications, need for hospitalisation, longer hospital stay, and had higher total costs associated with their stent removal.8,30,32 The reasons are likely related to longer survival and thus more time for the development of the complications, including embedding in the airway wall, GT formation, stent fatigue, and fracture. Stent removal in such cases can be difficult and hazardous, as it can result in mucosal tears, severe bleeding, re-obstruction, and respiratory failure with the need for postoperative mechanical ventilation, and tension pneumothorax.32 Stents are a benefit for patients struggling with central airway obstruction; however, constant vigilance is required to ensure complications do not arise.
CONCLUSION
Removing a tracheobronchial stent can have significant risks that may lead to major complications. Once placed, constant vigilance is necessary to judge the correct time to remove the stent. Careful and strategic planning is required by the physician performing the initial stent placement and/or removal. No stent should ever be left behind once it is not needed. We eagerly await the development of biodegradable stents and custom designed stents. These could obviate some of the complications that are associated with airway stents, which, in turn, would decrease the burden on the healthcare system as well as the patients.








