Abstract
The benefits of pulmonary rehabilitation (PR) diminish over 12–24 months following programme completion. A repeat PR programme may potentially prevent or reverse this decline in gains and may provide additional benefits. The aim of this narrative review was to discuss the current available evidence regarding repeat PR programmes and provide perspectives on unresolved questions, future areas of inquiry, and suggestions for clinical practice. Randomised controlled trials showed PR repeated at 6, 12, or 24 months after the initial PR programme resulted in similar short-term improvements in exercise capacity and quality of life; however, they did not result in long-term benefits beyond 12–24 months. In uncontrolled studies, the improvements in exercise capacity achieved following repeat PR were of a smaller magnitude than after the initial PR programme, but the improvements were still clinically significant. There is limited evidence to guide the optimal timing and characteristics of a repeat PR programme, such as frequency, duration and content, as well as which patients may benefit. There are ethical factors to consider in offering repeat PR programmes, including availability and access, the impact on resources and capacity of PR programmes, and patient-related factors such as financial burden and difficulties with transport. Alternate means of delivering a repeat PR programme should be explored, especially with emerging evidence for home-based PR and telerehabilitation programmes. A modular approach to a repeat PR programme by offering only certain elements rather than a comprehensive programme may also address the aspects of access, resources, capacity, and patient burden.
Key Points
1. Pulmonary rehabilitation (PR) is used as a treatment for patients with chronic obstructive pulmonary disease to optimise functional exercise capacity and to improve quality of life.2. In this literature review, the authors looked into previous studies, some of which indicated that repeat PR had less success in some patients, however, the improvements were still clinically significant.
3. Unless patients engage in regular exercise, the improvements made during the initial PR will decline; but, there is no consensus on when PR should be repeated.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) may progress over time, resulting in a gradual worsening of symptoms and decline in functional capacity and quality of life.1 Pulmonary rehabilitation (PR) aims to reduce symptoms and optimise functional capacity in people with COPD via a comprehensive intervention of exercise training, education, and behaviour change.2 However, the benefits of PR appear to diminish over time3 and seem to be time-limited to 12–24 months.4
A repeat PR programme at a future point after completion of the initial PR programme may prevent or reverse the decline of the initial training effects and may provide additional benefits. Whilst repeating a PR programme appears worthwhile considering the positive benefits of PR reduce over time, there are no strong recommendations for repeating a PR programme in current clinical practice guidelines. Therefore, the aim of this narrative review was to discuss the current evidence regarding repeat PR programmes and to provide perspectives on unresolved questions and future areas of inquiry.
METHODS
A literature search was performed in February 2022 using PubMed, Medline, PEDro, and Google Scholar. Initial keywords searched included “repeat” and “pulmonary rehabilitation.” An additional search using the keyword “refresher” found no further studies. Another search using the keyword “booster” found three extra studies. The reference lists of all reviewed literature were handsearched for additional references. There was no limitation applied to study design for a study to be reviewed. Only studies written in English and full-text were considered.
EVIDENCE OF REPEAT PULMONARY REHABILITATION PROGRAMMES
A modest number of studies examining the benefits of repeat PR programmes have been published since 2001. Two small randomised controlled trials with a combined total of 96 participants demonstrated that PR repeated at 6, 12, or 24 months after the initial PR programme resulted in similar short-term improvements in exercise capacity and quality of life; however, did not result in long-term benefits beyond 12–24 months.5,6 In uncontrolled studies, the overall results demonstrated that the improvements in exercise capacity achieved following a repeat PR programme were of a lower magnitude than after the initial PR programme, but the improvements were still clinically significant.7-11 There also appeared to be a reduction in the number of exacerbations per year6,11 and a reduction in days spent in hospital5 in people with COPD who received a repeat PR programme. However, the small number of exacerbations and hospitalisations limited the generalisability of these findings. Evidence suggests that people with more severe disease and those on long-term oxygen therapy may be less likely to respond to a repeat PR programme,7 although this requires further investigation.
EVIDENCE GAPS
The British Thoracic Society (BTS) guideline on PR recommends that repeat PR programmes should be considered in patients who have completed a course of PR more than 1 year prior and that repeat PR programmes should be considered sooner in individuals with accelerated physiological decline.12 The American Thoracic Society (ATS)/European Respiratory Society (ERS) statement on PR examined the evidence regarding repeat PR programmes to prevent decline in PR outcomes and/or following a decline in function, and identified the optimal duration and frequency of repeat PR programmes over time to be a key area for future research.2 Despite this, little progress has been made in this research area, and no randomised controlled trials have been published since 2009. Of note, evidence emerging in more recent years includes uncontrolled studies reporting real-world PR programme data, where clinicians have identified a clinical need for repeat PR programmes in their patients and have been offering these programmes for many years.7-10
Although there is a paucity of high-quality trials regarding repeat PR programmes, expert consensus appears to mirror that of PR clinicians, with repeat PR programmes likely suitable for patients at risk of decline.12-16 The authors hypothesise that other research priorities in clinical practice have overshadowed the need to further investigate repeat PR programmes. These research priorities include the effect of PR in diseases other than COPD,17-19 particularly the severe acute respiratory syndrome coronavirus 2 infection20,21 and the identification of post-COVID-19 condition,22,23 and different models of PR delivery, including home-based PR24 and telerehabilitation.25
In clinical practice, the authors further hypothesise that there are growing numbers of actual and perceived barriers to offering repeat PR programmes, including increased demands on PR programmes to deliver PR to a larger population of people living with chronic respiratory disease beyond COPD; increased referral to PR programmes due to an increase in awareness and diagnosis of COPD, along with a greater understanding of the evidence and benefits of PR; a lack of availability of PR programmes or limited/no change to historical funding models for PR, which has led to difficulty offering repeat PR programmes in some countries; perceived reduced value of repeat PR programmes in some people attending PR with advancing age, disease progression, and an increasing number of comorbidities; cost–benefit considerations with an impetus to use limited healthcare resources on new patients referred to PR rather than returning patients, as it may be difficult to financially justify additional healthcare resource utilisation on people who have already accessed a service; and finally, an ethical consideration of offering a place in a PR programme to patients who never attended over those who previously attended in the context of waiting lists and accessibility to an evidence-based programme.
DEFINING REPEAT PULMONARY REHABILITATION PROGRAMMES: COMPONENTS AND DURATION
In clinical practice, it is unclear if repeat PR programmes should be the same or different to the initial PR programme. To date in literature, repeat PR programmes have been reported to consist of the same components as the initial PR programme (i.e., exercise training, education, and support).6,7,9,11,26 The reported duration of the repeat PR programmes ranges from outpatient programmes of 8–12 weeks,6,7,9-11 to inpatient programmes of 4 weeks.27
With this limited evidence, one key question arises: should repeat PR programmes be the same as the initial PR programme (i.e., consist of the same components and duration)? Repeat PR programmes have the opportunity to provide a different approach to the initial PR programme, including consideration of shorter programmes with or without the education component, as people with COPD may not require all aspects of the repeat PR programme. Heng et al.10 demonstrated that a repeat PR programme achieved greater gains in disease mastery than the initial PR programme, suggesting that more time and support was required to help patients achieve these gains. A personalised and individualised repeat PR programme seems intuitive, yet the repeat PR programme duration and required components remain unclear.
OPTIMAL TIME TO REPEAT A PULOMARY REHABILITATION PROGRAMME
How often should PR programmes be repeated? In clinical practice, the time between completion of an initial PR programme and a repeat PR programme varies, and is frequently dependent on available resources, waiting lists, and patient needs. Patients may be re-referred by the general practitioner or respiratory specialist but may also self-refer to the PR programme if they need assistance. However, not all PR programmes have the ability to offer a repeat PR programme due to programme demands and waiting lists.
Following the completion of the initial PR programme, repeat PR programmes have been offered at 6 months,26 12 months,10 10–24 months,7 24 months,27 and five times over 7 years,11 indicating that there is no clear consensus about the ideal duration between the initial PR programme and repeat PR programme, or the frequency of repeating a PR programme. Therefore, determining the time point and frequency of repeat PR programmes is important in future research.
REPEAT PULMONARY REHABILITATION PROGRAMMES AS A MAINTENANCE PROGRAMME
Following the completion of an initial PR programme, benefits in exercise capacity, dyspnoea, and health-related quality of life begin to decline unless the person continues to engage in regular exercise.28 Supervised maintenance exercise programmes may be offered, but the ideal frequency of maintenance exercise is unclear,17 and many PR programmes are unable to provide supervised maintenance exercise classes because of programme demands and staffing constraints. Instead, patients are encouraged to engage in regular supervised community exercise classes or exercise independently. However, if patients do not engage in regular exercise, or if a maintenance exercise programme lacks the appropriate intensity, and patients experience a decline in the initial PR programme benefits, a repeat PR programme may be indicated to address this. Encouraging people to continue to regularly exercise following the completion of the initial PR programme is best practice2,12 and may negate the need for a repeat PR programme. However, repeat PR programmes may be an option for people who have not engaged in ongoing exercise or if maintenance exercise programmes have been unable to maintain gains from the initial PR programme.
WHO SHOULD BE OFFERED A REPEAT PULMONARY REHABILITATION PROGRAMME?
It is important to try to distinguish those who would benefit from repeat PR programmes. Whilst repeat PR programmes may benefit people who are showing signs of physical decline since the completion of the initial PR programme9 or following an exacerbation,26 it is unclear from previous studies whether the repeat PR programmes were planned at certain time points or offered on an as-needed basis. Based on the studies to date, there is no clear guidance about what characteristics a patient may exhibit to indicate a need to repeat a PR programme. Further, there is no defined level of deconditioning or decline that would currently indicate a need for a repeat PR programme, for example, a percent decline in 6-minute walk distance since completion of the initial PR programme; a patient no longer achieving the minimal clinically important difference for improvements in exercise capacity, dyspnoea, or health-related quality of life; or an increase in the number of exacerbations or hospitalisations over a defined period of time (e.g., 12 months). Defining the repeat PR programme patient is an area for future investigation.
Repeating the PR programme implies that the patient attending the repeat PR programme has completed the initial PR programme. Therefore, it may be assumed that they are more likely to also complete the repeat PR programme. However, should every completer be offered a repeat PR programme at a specific time interval, e.g., 12 months following completion of the initial PR programme, or should they be empowered during an initial PR programme to continue to exercise and remain active? If a patient has not experienced a decline following the initial PR programme, then a repeat PR programme is unlikely to be required. This also raises an important issue that repeating a PR programme may only target a relatively small number of people who have completed the initial PR programme.
It is important to note that patients who complete the initial PR programme may or may not be responders (i.e., have achieved the minimal clinically important difference for one or more of the outcomes measured). In a recent study of 190 people with COPD who completed two PR programmes 10–14 months apart, 54% of non-responders following the initial PR programme become responders following the repeat PR programme. Of the 149 responders, 44 (30%) became non-responders.7 Perhaps unsurprisingly, the more severe patients (those on long-term oxygen therapy and with severe dyspnoea) often remained non-responders.7 This study raises important issues for clinicians as one cannot predict how a patient will respond to a repeat PR programme and whether they will or will not experience important and meaningful gains. It is suggested that patients should not be offered places in repeat PR programmes based on past performance but on current needs such as functional capacity or recent decline.7
Repeat PR programmes on a predetermined periodical basis may not be indicated for some people with COPD at that particular point in time. Rather, offering repeat PR programmes to people with COPD on an as-needed basis appears to be beneficial even after a prolonged period of time between the interventions.9 Clinically, it appears the reasons for a repeat PR programme are varied and locally tailored to individual programmes, ranging from yearly reviews where a worsening state indicates a need to repeat a PR programme27 to being re-referred by respiratory physicians “based on clinical necessity.”8 The element of patient desire and choice, which in the authors’ experience is a significant factor, has not been reported as a reason for repeating a PR programme. In summary, it is unclear which people are ideally suited to repeat the PR programme. Suggestions include patients (both responders and non-responders) who have shown decline,8,9,27 patients who have not achieved improvements or mastery in some aspects of the initial PR programme,10 and patients following an exacerbation.26
REPEATING A PULMONARY REHABILITATION PROGRAMME AFTER A HOSPITAL ADMISSION OR AN ACUTE EXACERBATION OF COPD
Patients who show a decline in function following an acute exacerbation of COPD (AECOPD) or hospital admission may need a short repeat PR programme, such as a booster PR programme of 3–4 weeks duration. An AECOPD within 6 months of an initial PR programme has been shown to significantly decrease health-related quality of life and exercise capacity.26 A 3-week repeat PR programme following an AECOPD compared with control (no exercise training) demonstrated that there was a greater reduction in dyspnoea and improved 6-minute walk distance compared with the control group.26 The results from this study support the concept of providing a booster PR soon after an AECOPD.
A Cochrane review recommended that access to PR within 28 days of hospital discharge could prevent readmission in people with COPD.29 This recommendation supports early attendance at PR to avoid readmission and the concept of a booster PR programme may provide an option to prevent readmission. Whilst in the authors’ experience, booster PR programmes following hospital admissions or AECOPD are frequently offered in the clinical setting, currently there is no evidence to support repeat PR programmes as booster programmes.
PATIENT PERSPECTIVE
There is a paucity of studies examining patient perceptions around repeating a PR programme. Storey et al.30 identified external drivers, such as hospitalisation, changes in health, and physical fitness or breathing, rather than personal motivation, to be key factors in a patient repeating a PR programme. Participants identified supervision within PR to be a key external motivator to maintaining regular exercise, with a repeat PR programme improving confidence and motivation. However, patient experiences varied with repeat PR programmes. Compared with the initial PR programme, some participants found the repeat PR programme similar or easier, whilst some participants were confronted by their decline in health status when repeating the PR programme. Further, re-referral to PR was predominantly led by health professionals (despite acknowledging numerous barriers to repeating a PR programme) rather than through self-referral, with no consensus reached on the optimal time to repeat PR. For those patients that self-referred, it remains unclear if they can be defined by particular demographics or characteristics. Whether patients that re-refer to a repeat PR programme have common characteristics, such as age, disease severity, personality traits, previous improvement or lack thereof in PR outcomes, psychosocial aspects and needs, or presence of comorbidities, poses an interesting future research question. Importantly though, through the understanding of patient drivers to re-engage in PR, it may assist in supporting and facilitating the offering of alternative modes of PR that align with patient requirements,31 including to those people repeating a PR programme.
AVAILABILITY AND ACCESS TO PULMONARY REHABILITATION PROGRAMMES
Availability of PR services has been reported to be as low as 1.2% of the estimated number of people with COPD, regardless of country.32 Ongoing accessibility issues with centre-based PR continue to prevail,33 raising three key issues to offering a repeat PR programme to those who have already attended the programme: will offering a repeat PR programme further impact on the capacity of PR services to deliver their programs by increasing demand and reducing availability, will offering a repeat PR programme exacerbate ongoing patient access issues such as cost of travel and difficulty with transport,34 and can alternative models of repeat PR programmes mitigate the increased demand on service delivery.
FUTURE MODELS OF REPEAT PULMONARY REHABILITATION PROGRAMMES
Over the last decade, especially since the emergence of COVID-19, alternative modes of delivering PR have increased availability and popularity. Home-based PR35 or home-based telerehabilitation delivered via different technologies, such as videoconferencing, mobile applications,25 or social media,36 have shown similar clinical outcomes compared to traditional centre-based PR programmes. Further, many people with COPD attending PR have reported a willingness to use telerehabilitation.37 With the emergence of innovative PR delivery models, it is conceivable that a repeat PR programme could be offered through similar alternate models to centre-based PR, thus minimising the impact on traditional centre-based PR programmes, and potentially appealing to a wider range of patients. Further research is needed to determine whether participants repeating a PR programme would consider or participate in repeat PR via alternate delivery modes.
If a PR programme cannot facilitate a repeat PR programme through alternate modes of PR or a patient does not want to engage in alternate models, modular repeat PR programmes,33,38 which are individualised to a patient’s needs and impairments where there is an indication of a decline in function or limitation, may be another possible alternative. Offering only the elements of PR that the patient requires, such as exercise training only, an aspect of self-management education (for example, inhaler devices, smoking cessation, or healthy eating), or a combination of a few elements,33 may reduce the burden on PR programme resourcing while simultaneously facilitating patient-centred repeat PR programmes. Modular repeat PR programmes are a further avenue of future research. Despite the lack of evidence supporting an optimal model of a repeat PR programme, the authors have some key suggestions that healthcare professionals working in PR can take away from this narrative review of the literature (Table 1) and contemplate when thinking about a repeat PR programme for their patients.
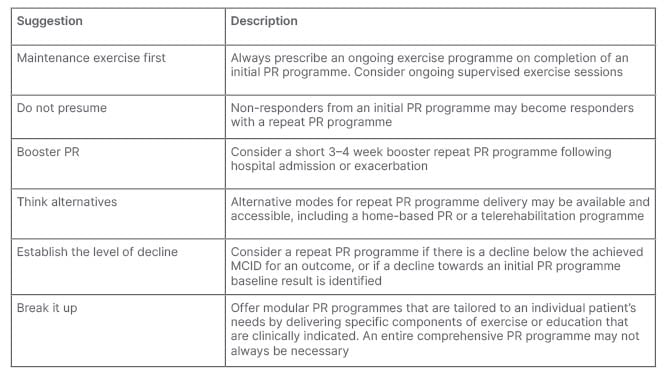
Table 1: Suggestions for repeat pulmonary rehabilitation programmes in clinical practice.
PR: pulmonary rehabilitation; MCID: minimal clinically important difference.
CONCLUSION
Following an initial PR programme, there is limited evidence to guide the optimal timing and characteristics of a repeat PR programme, such as frequency, duration, and content, as well as which patients may benefit. Further, patient perspectives have not been widely considered. There are ethical factors to consider in offering repeat PR programmes, including equity of access, the impact on resources and capacity of PR programmes, and patient-related factors such as financial burden and difficulties with transport and access.
Alternate means of delivering a repeat PR programme should be considered, especially in light of emerging evidence for home-based PR programmes and telerehabilitation programmes. A modular approach to a repeat PR programme by offering only identified elements rather than a comprehensive programme may also address the ethical aspects of access, capacity, resources, and burden to patients. It is exciting to consider the large number of research questions this review has posed and the potential for important findings identifying optimal models for repeat PR programmes.








