BACKGROUND AND AIMS
Histology is a key element for the multidisciplinary diagnosis of fibrotic diffuse parenchymal lung diseases (f-DPLD) when the clinical–radiological setting of f-DPLD with high-resolution CT features diagnostic of usual interstitial pneumonia (UIP) are not present.1
The author compared the diagnostic yield and safety of transbronchial lung cryobiopsy (TBLC) with cryoprobe sampling versus conventional transbronchial lung biopsy (TBLB) forceps sampling in the same patient.
MATERIALS AND METHODS
A prospective, single-centre clinical study of 135 patients with f-DPLD indicated for lung biopsy with histopathology. TBLB subsequently was followed by TBLC. Airway management with rigid bronchoscope was done according to protocol, and the procedure was performed using fluoroscopy and Fogarty occlusion balloon (Edwards Lifesciences, Irvine, California, USA).2
RESULTS
According to multidisciplinary committee results, the diagnostic yield for TBLC was 79.6% and 51.4% for TBLB (p<0.0001). The diagnostic yield was higher for TBLC compared with forceps TBLB for two groups: idiopathic interstitial pneumonias and interstitial lung disease of known cause or association (odds ratio: 2.5; 95% confidence interval [CI]: 1.4–4.2 and odds ratio: 5.8; 95% Cl: 2.3–14.3, respectively). Agreement between pathologists in the detection of UIP was very good, with a κ coefficient of 0.83 (95% CI: 0.69–0.97). Grade 3 (moderate) bleeding after TBLC occurred in 5.5% of patients compared with 0.8% after conventional TBLB, which confirms the need for safe airway management and prophylactic occlusion balloon use. Incidence of pneumothorax was seen in four patients when sampling two sites or when using a larger probe, while bleeding was not influenced by the site of the biopsy or by the size of the probe.3 No patient required intubation with invasive mechanical ventilation and there were no procedure-related deaths.
CONCLUSION
The advent of TBLC has generated enthusiasm and has provided a higher diagnostic yield than TBLB, with fewer complications than surgery. TBLC specimens are larger in biopsy size, with better parenchymal architecture preservation, contain more alveoli, and have fewer artefacts compared with TBLB (Figure 1).4
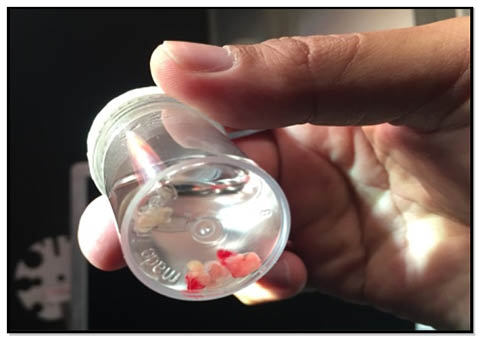
Figure 1: Freshly obtained transbronchial lung cryobiopsy specimens floating in formalin.6
The author has attempted to identify which patient may benefit from the use of combined techniques by performing both techniques in the same patients, which included idiopathic, connective tissue disease-related, and other disease process that have not been previously investigated with TBLC techniques. The diagnostic yield for TBLC was higher than TBLB, especially for idiopathic interstitial pneumonia and interstitial lung disease of known cause or association. The incidence of pneumothorax is mainly related to necessity of biopsy of the subpleural areas in patients with f-DPLDs. TBLC findings suggesting UIP, such as temporal heterogeneity, fibroblastic foci, and honeycombing, were strongly correlated with final diagnosis of f-DPLD.1
Patients with f-DPLD represent a diagnostic challenge and often limited by a smaller size and fewer artefacts; however, a clinician can be hesitant to pursue this surgical biopsy due to more acute exacerbations observed after procedure or due to intraparenchymal shear forces induced by mechanical unilateral ventilation, which is used when performing a surgical lung biopsy.5 Complications such as pneumonia, persistent pleural fistula, neuropathic pain, and empyema have been often observed in surgical lung biopsy studies.








