AIM
Dust load and oxidative stress play a leading role in the development of pneumoconiosis.1,2 The aim of this study was to examine the role of macrophages and oxidative activity in the development of pneumoconiosis in the rat model.
METHODS
Polymetallic dust (PD) from the grinder work place contained Fe (39.2%); SiO2 (21.3%); Mg 8.5%; Cr and Al (2.0%); C and Mn (1.0%); Zn, Ti, Co, Cu, Zr, and Pb (<1.0%); and traces of Cd and W. Morphology signs and cytology of bronchoalveolar lavage fluid (BALF) in 120 Wistar rats’ lungs after single (SII), double (DII), or triple intratracheal instillation (TII), with a 1-month interval of PD, were examined on the 3rd, 7th, 14th, and 30th day, and 3, 6, and 12 months after exposure. The phagocytic activity of alveolar macrophages (PAAM), and spontaneous (CLsp) and stimulated (CLst) luminol-dependent chemiluminescence were investigated.
RESULTS
Upon examination on the 3rd and 7th day after SII PD exposure, erosive bronchitis, bronchiolitis, pneumonia, and perivascular lymphocytic infiltration had developed. Granulomas of macrophages were numerous from the 14th. After 1 year DII and TII of PD resulted in pneumoconiosis, i.e., macrophage granulomas of foreign bodies, lymphocytic infiltration, focal sclerosis, and irregular emphysema, observed after 6 months.
After SII BALF neutrophilia, maximum levels of CLsp and CLst were observed on the third day (p<0.05 for all parameters), while lymphocytosis and maximum levels of PAAM were observed on the fourteenth day (both p<0.05) (Figure 1). PAAM and CLst continued to increase up to Month 3 (p<0.05). After DII and TII of PD, BALF lymphocytosis and increased PAAM, CLsp, and CLst levels were revealed up to Month 6 (p<0.05 to all parameters in TII cases).
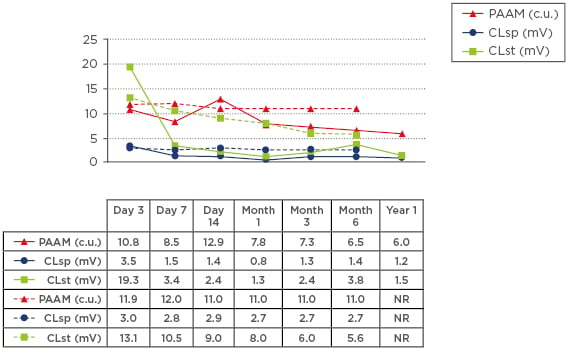
Figure 1: PAAM, CLsp, and CLst in rats’ BALF and SII (–) and TII (- -) of polymetallic dust.
BALF: bronchoalveolar lavage fluid; CLsp: spontaneous luminol-dependent chemiluminescence; CLst: stimulated luminol-dependent chemiluminescence; NR: not recorded; PAAM: phagocytic activity of alveolar macrophages; SII: single intratracheal instillation; TII: triple intratracheal instillation.
CONCLUSION
Only DII or TII of PD may result in experimental pneumoconiosis, which demonstrates the impact of prolonged dust exposure. Activation of macrophages and their oxidative activity is important in pneumoconiosis pathogenesis.








