BACKGROUND AND AIMS
Exposure to pollen has been associated with an increased risk of respiratory symptoms in both allergic1 and nonallergic individuals.2 However, the association of pollen exposure with respiratory symptoms during infancy, a particularly vulnerable period for lung development,3 remains unclear. The goal of this study was to examine whether pollen exposure is associated with respiratory symptoms (cough, wheezing, and dyspnoea) during the first year of life and to test if maternal atopy, infant’s sex, and air pollution modify this association.
MATERIALS AND METHODS
In total, 14,874 repeated measures from 401 healthy infants of the prospective Basel Bern Infant Lung Development (BILD) cohort were analysed. Generalised additive mixed models were used to assess the association between weekly exposure to tree and grass pollen estimated for each child’s address and weekly respiratory symptom scores. The scale for respiratory symptom scores ranged from 0–4, with 0 indicating no symptoms and scores ≥1 indicating symptoms with increasing severity. Effect modification by maternal atopy, infant’s sex, and air pollution (nitrogen dioxide and fine particulate matter with a diameter ≤2.5 μm [PM2.5]) was assessed with interaction terms.
RESULTS
Per infant, 37±2 (mean±standard deviation) respiratory symptom scores were assessed during the analysed months of the first year of life (from January up to and including September due to operation time of pollen traps). The symptom severity was overall rather low with a mean±standard deviation respiratory symptom score across all years (2005–2016) of 0.13±0.13 for daytime respiratory symptoms and 0.12±0.14 for night-time respiratory symptoms. Significant associations were found for grass and tree pollen exposure, both combined and separately, with respiratory symptoms during the first year of life (Figure 1). An increase in pollen exposure was associated with an increased risk of respiratory symptoms during daytime (combined risk ratio [RR]: 1.006 [95% confidence interval (CI):1.002, 1.009]; tree RR: 1.005 [95% CI: 1.002, 1.008]; and grass RR: 1.009 [95% CI: 1.000, 1.23] per 10% pollen/m3) and night-time (combined RR: 1.003 [95% CI: 0.999, 1.007]; tree RR: 1.003 [95% CI: 0.999, 1.007]; and grass RR: 1.014 [95% CI: 1.004, 1.024] per 10% pollen/m3). Results remained significant after the exclusion of observations from the first 6 months of life, when the infant’s blood could potentially be contaminated by maternal Ig. The effect of pollen on respiratory symptoms was not modified by maternal atopy and infant’s sex. However, a complex crossover interaction between exposure to combined pollen and PM2.5 was found (p=0.003). For low pollen concentrations, the risk of respiratory symptoms increased with increasing levels of PM2.5, while the risk of respiratory symptoms decreased with increasing levels of PM2.5 for high pollen concentrations.
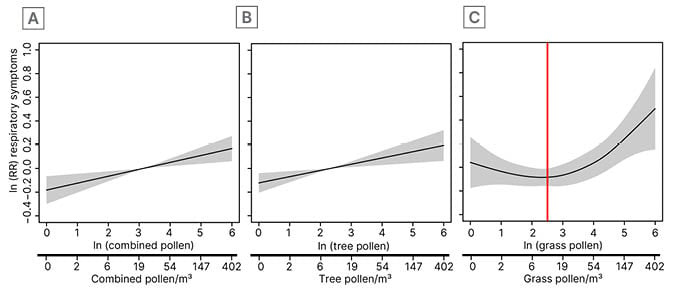
Figure 1: Marginal effects of pollen exposure on the risk of daytime respiratory symptoms.
Pollen exposure is shown on transformed scale and back-transformed scale. The shaded areas represent the 95% CI. Models were adjusted for NO2, PM2.5, siblings, childcare, sex, breastfeeding, age, maternal smoking during pregnancy, temperature, and month. A) Shows an association between combined pollen and daytime respiratory symptoms, while B) highlights an association between tree pollen and daytime respiratory symptoms. C) Association between grass pollen and daytime respiratory symptoms. The red line indicates the cut-off used to assess linear relationship between grass pollen and respiratory symptoms.
CI: confidence interval; ln: natural logarithm; NO2: nitrogen dioxide; PM2.5: particulate matter with a diameter ≤2.5 μm; RR: risk ratio.
CONCLUSION
This study provides first evidence that, even as early as during the first year of life, increased exposure to grass and tree pollen, both combined and separately, is associated with an increased risk of respiratory symptoms. While PM2.5 modified the effect of pollen in a complex manner, maternal atopy and infant’s sex did not affect the association of pollen with respiratory symptoms. As infancy is a particularly vulnerable period for lung development, the observed association should be further investigated. This includes an evaluation of the underlying mechanism linking pollen exposure with respiratory symptoms in infants.








