BACKGROUND AND AIMS
Pulmonary sequelae after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection range from limited abnormalities to major interstitial lung diseases (ILD). Bronchoalveolar lavage (BAL) and cryobiopsy findings, integrated with the clinical and radiological scenario, may help clinicians to correctly manage patients and aid researchers in better understanding the features and pathogenic mechanisms of post-COVID-19 fibrosis.
MATERIALS AND METHODS
The authors conducted PCOILS, a prospective, multicentre, national (Italian) study. In two centres, Florence and Forlì, subsequent patients seen at 4–18 months after the acute infection. They underwent transbronchial lung cryobiopsy and BAL if they showed a significant ILD on follow up with high-resolution CT (HRCT; progressive and/or symptomatic and/or with pulmonary function impairment). The authors enrolled 266 patients with follow-up HRTC at 6 months after infection. Patients underwent chest HRTC during follow-up (after 6, 12, and 18 months) and in anticipation of biopsy. Cryobiopsy was proposed to patients when the post-COVID-19 ILD was persistent and clinically significant.
RESULTS
In total, 19 patients were biopsied. Patients underwent cryobiopsy at different timings with respect to SARS-CoV-2 infection, with an interval that varied between 4 months and 18 months (median: 6 months). The median age of patients was 66 years (range: 39–76 years). Of the patients, 18 were male (95%) and one was female (5%). Eleven cases (58%) were former smokers. Eight out of 19 (42%) patients had occupational exposure that may result in ILD. The authors’ radiologists evaluated the cases and found a median extent of damage of 40% (range: 10–70%).
The patterns according to Solomon-Lynch were 10 cases of mixed ground-glass opacity (GGO) and fibrosis; five cases of GGO, three predominantly fibrotic; and one case of sarcoid-like reaction. Pulmonary function tests were performed in all patients with median forced vital capacity values of 89% (53–123), and median diffusing capacity of the lungs for carbon monoxide values of 66% (37–106). Once the histological preparations were acquired, three different pathologists (University Hospital of Careggi, Hospital of Reggio Emilia, and Hospital of Forlì, Italy) evaluated the images in blind, entering the data in the platform. Then, a multidisciplinary (pulmonologists, pathologists, and radiologists) evaluation was performed reaching a consensus.
As shown in Figure 1, the authors identified three post-COVID-19 phenotypes: prominent vascular changes, post-COVID-19 fibrosis, and persistent SARS-CoV-2 infection. The first phenotype (vascular) was detected in two cases that were biopsied early after acute COVID-19 (4 months and 5 months, respectively). Their HRCT showed pure GGO and the histology showed haemangiomatosis-like features (Figure 1). The patients were followed up without treatment.
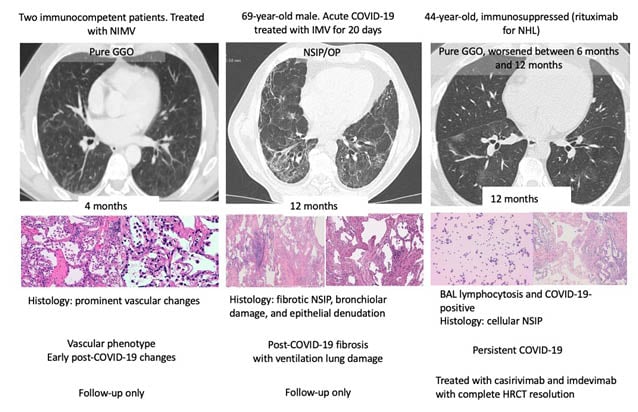
Figure 1: Three post-COVID-19 phenotypes were identified by the authors.
BAL: bronchoalveolar lavage; GGO: ground-glass opacity; HRCT: high-resolution CT; IMV: intermittent mandatory ventilation; NHL: non-Hodgkin lymphoma; NIMV: non-invasive motion ventilation; NSIP/OP: nonspecific interstitial pneumonia overlap organising pneumonia.
The second phenotype (post-COVID-19 fibrosis) was detected in seven patients, all with HRCT nonspecific interstitial pneumonia (NSIP) with organising pneumonia overlap features. Histology showed fibrotic or mixed NSIP, fibrotic organising pneumonia, fibrotic diffuse alveolar damage, and bronchiolar damage, possibly correlated with ventilation injury in one case (Figure 1). Patients were variably treated with steroids, depending on disease extent and symptoms. In the case with post-ventilation injury, which did not show inflammation on biopsy, corticosteroids were stopped.
The third phenotype (persistent COVID-19) was detected in a patient who was immunosuppressed (rituximab for non-Hodgkin lymphoma) and the HRCT showed GGOs that worsened between 6 months and 12 months. COVID-19 was detected by BAL (SARS-CoV-2 positivity and CD8+ lymphocytosis [53% total lymph; CD4/CD8: 0.1]) and biopsy showed cellular NSIP. This patient was treated with casirivimab and imdevimab with complete resolution.
The remaining nine patients were reclassified as known ILDs and treated according to current guidelines.
CONCLUSION
The authors identified three phenotypes of post-COVID-19 damage with heterogeneous pictures and leading to different treatment choices. The multidisciplinary evaluation was crucial to reach the most accurate diagnosis for the patient.








