Abstract
Objective: To determine the correlation between colposcopic and final histopathologic results amongst patients undergoing a colposcopic evaluation in cervical dysplasia clinics in Western Kenya.
Methods: This was a cross-sectional study, conducted among 164 females undergoing colposcopic evaluation across several cervical dysplasia clinics in Western Kenya. Colposcopy and histopathology were performed. Colposcopy findings were graded using modified Reid’s Colposcopic Index (RCI). Bayes’ theorem model was used to determine the sensitivity, specificity, positive predictive value, and negative predictive value. An overall ĸ value was calculated as an estimate of the strength of correlation between colposcopy and histopathology.
Results: Mean age of the study participants was 40.6 years. Modified RCI classified 20.7%, 40.2%, and 39.1% between a score of 0–2, 3–5, and 6–8, respectively. Colposcopy classified 0.6%, 38.4%, and 60.1% as normal, cervical intraepithelial neoplasia (CIN) 1 (low risk), and CIN 2–3 (medium–high risk), respectively. Histopathology classified 16.5%, 26.2%, 53.3%, and 3.0% as having normal, CIN 1, CIN 2–3, or carcinoma in situ, respectively. Sensitivity, specificity, positive predictive value, and negative predictive value were 85.3%, 69.7%, 80.3%, and 69.7%, respectively. The estimated strength of correlation between colposcopy and biopsy was relatively strong (ĸ=0.55).
Conclusion: There is an association between the discriminatory powers of colposcopy and histology, but colposcopy had a lower specificity when compared to histopathology.
Key Points
1. Using modified Reid’s Colposcopic Index (RCI) in evaluating the cervix gives a systematic and objective method of colposcopically grading the severity of premalignant cervical lesions.
2. The findings from this study provide information on the sensitivity and specificity of colposcopy in Western Kenya.
3. This study reports an association between the discriminatory power of the two methods; however, colposcopy had a lower specificity when compared to histopathology.
BACKGROUND
Cervical cancer is a consequence of long-term infection with human papillomavirus. It is ranked fourth in both incidence and cancer-related mortality amongst females, with an estimated 569,847 new cases and 311,365 global deaths per annum. This accounts for 13.1% of all new female cancers worldwide. In Eastern Africa, cervical cancer remains the most common cancer in females, with estimated age standardised incidence and mortality rates of 40.1 and 30.0 per 100,000 people.1
Cervical cancer contributes 5,250 (12.9%) of the new cancer cases annually, and 3,286 (11.84%) of all cancer deaths annually in Kenya. It is the leading cause of cancer-related deaths in Kenya, and the second most common cancer among females.1
Colposcopy is the examination of the epithelia of the cervix, lower genital tract, and anogenital area using magnified illumination, after the application of specific solutions to detect abnormal appearances consistent with dysplasia or neoplasia, or to affirm normality. Integral to the procedure is targeting biopsies to areas of greatest abnormality.2 It is also well documented that colposcopy has significant interperformer variability, and poor reliability. The American Society for Colposcopy and Cervical Pathology (ASCCP) published colposcopy standards to address these, and other concerns.3
Cervical cancer has high morbidity and mortality. In Kenya, it is the second in prevalence, and the first cause of cancer-related mortality.1 Cervical cancer has a long latent phase, and can be prevented and cured if detected early. The primary method for cervical cancer prevention is through vaccination against human papillomavirus, while the secondary method of cervical cancer prevention is through cervical cancer screening.4
Cervical cancer initially presents as cervical dysplasia, which may transform into cervical cancer. The diagnosis of cervical dysplasia utilises both colposcopy and histopathology to inform patient management. Although histopathology is the gold standard for diagnosing cervical cancer, its access and utility is limited, due to both cost and limited expertise. There is also a paucity of data on the sensitivity and specificity of colposcopy locally, hence the need to determine the sensitivity and specificity of colposcopy.
OBJECTIVE
The objective is to determine the sensitivity and specificity of colposcopy findings among patients undergoing colposcopy and biopsy in several cervical dysplasia clinics across Western Kenya.
METHODS
This was a cross-sectional, comparative diagnostic study conducted among 164 females undergoing colposcopic evaluation across several cervical dysplasia clinics in Western Kenya, between August 2019–August 2020. Institutional ethical approval was sought, and informed consent obtained from each participant. A colposcope was used to examine the cervix, and findings were graded using the modified Reid’s Colposcopic Index (RCI).5 A colposcopy-guided punch biopsy was then taken for histopathological evaluation when the abnormal area was sighted. Descriptive statistical analysis of mean, with corresponding standard deviation for continuous variables; and frequencies, with corresponding proportions for categorical variables were calculated, to determine whether differences across groups were statistically significant (P≤0.05). Bayes’ theorem model was used to determine the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV), with a corresponding 95% confidence interval. A receiver operating characteristic curve was plotted as sensitivity against 1-specificity, and the area under the curve was computed. An overall ĸ value was calculated as an estimate of the strength of correlation between colposcopy and histopathology.
Permission to conduct the research was sought and obtained from the Institutional Ethics and Research Committee (IREC) of Moi University School of Medicine and Moi Teaching and Referral Hospital, Eldoret, Kenya.
RESULTS
Sociodemographic Characteristics of the Study Participants
The mean age of the study participants was 40.6 years. The majority were married (79.9%), and 51.8% were educated to primary level. Of the participants, 134 (81.7%) were not post-menopausal, and 106 (64.6%) were HIV-negative.
Colposcopy Findings Using Modified Reid’s Colposcopic Index Among Patients Undergoing Colposcopy in Cervical Dysplasia Clinics in Western Kenya
Modified RCI classified 20.7%, 40.2%, and 39.1% between a score of 0–2, 3–5, and 6–8, respectively (Table 1). Colposcopy classified 0.6%, 38.4%, and 60.1% as normal, cervical intraepithelial neoplasia (CIN) 1, and CIN 2–3, respectively. Histopathology classified 16.5%, 26.2%, 53.3%, and 3.0% as having normal, CIN 1, CIN 2–3, and carcinoma in situ, respectively.
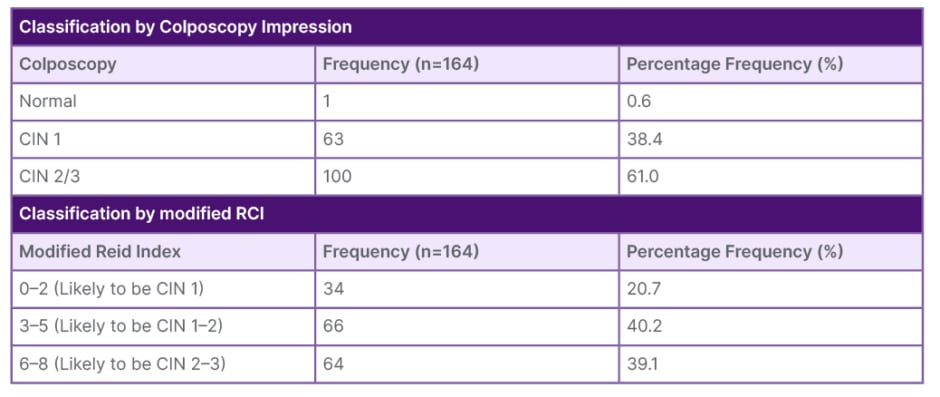
Table 1: Classification by colposcopy impression and classification by modified Reid’s Colposcopic Index.
CIN: cervical intraepithelial neoplasia; RCI: Reid’s Colposcopic Index.
DISCUSSION
This study involved 164 patients who were subjected to both colposcopy and biopsy diagnostic techniques, to compare the accuracy of the former in approximating the results obtained by biopsy. Biopsy results were considered as the gold standard in this sensitivity–specificity study. A total of 32 subjects were dropped from the analysis, as histopathology results classified 27 patients as having a normal cervix. On the contrary, patients who had normal colposcopy results were never subjected to histopathology examination. Comparing the two methods based on this category would have introduced bias by design. Likewise, histopathology results classified five patients as having a carcinoma. Colposcopy was never used to determine carcinoma. Comparing the two diagnostic methods based on this category would have also introduced design bias.
Sensitivity analysis for colposcopy as a diagnostic method was based on its ability to discriminate CIN 2–3 from CIN 1 (Table 2). A χ2 test conducted on the outcome from 132 patients revealed a highly significant association between colposcopy and biopsy in discriminating CIN 2–3 from CIN 1 (p<0.0001; χ2: 37.7; degree of freedom: 1). There was a fairly strong resemblance in the results from colposcopy and biopsy diagnostic techniques (ĸ: 0.55; 95% confidence interval: 0.40–0.70; p<0.0001). Aue-Aungkul and Suprasert6 compared the results obtained from RCI evaluation and biopsy results. Their study involved the comparison of diagnoses carried out by general and oncologic gynaecologists. They estimated the strength of the correlation (ĸ) between colposcopy impression and biopsy results on diagnoses carried out by the oncologic gynaecologists group to be equal to 0.34, while that of the general gynaecologist group was equal to 0.22.6 In both cases, the estimated strength of correlation was weaker than that which was obtained in this study (ĸ: 0.55).
Colposcopy had a sensitivity of 85.3% and specificity of 69.7% (Table 3). In a prospective, cross-sectional study on the correlation of colposcopy using RCI and histopathology, Durdi et al.7 yielded comparable results on sensitivity. They found a sensitivity of 88.5% with CIN 1 as a disease threshold, and 85.2% with CIN 2 as a disease threshold, with a relatively high specificity of 76.2% with CIN 1 as a disease threshold, and 99.6% with CIN 2 as a disease threshold. The study was conducted in the colposcopy clinic at KLES Dr Prabhakar Kore Hospital & Medical Research Center, Belgaum, Karnakata, India, between January 2008–June 2009, with a sample size of 268. Aue-Aungkul and Suprasert6 estimated a comparable specificity of 70.2% in their study on RCI evaluation, with a sample size of 125 patients.5 The authors’ study shows that there is a probability of approximately 85.3% that the colposcopy test will return a positive CIN 2–3 result among a population with CIN 2–3. The authors’ study also shows that colposcopy has a 69.7% chance of returning CIN 1 among a population with CIN 1.
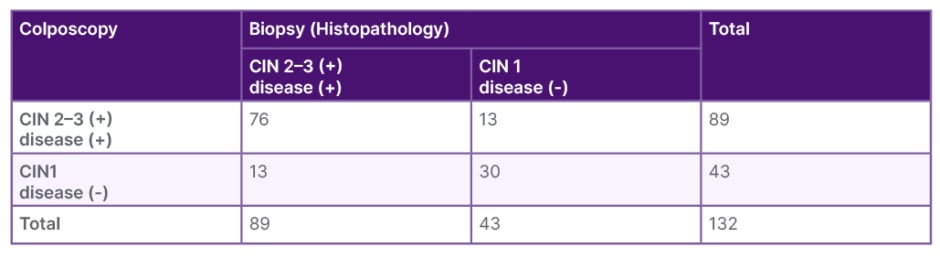
Table 2: Confusion matrix of colposcopy against biopsy.
CIN: cervical intraepithelial neoplasia.
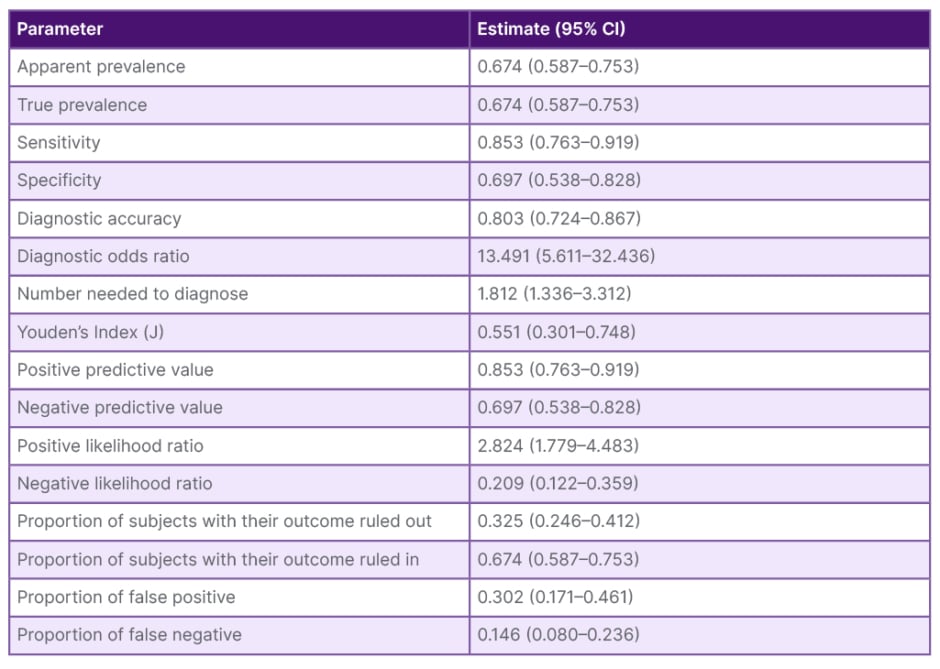
Table 3: Sensitivity analysis of colposcopy as a diagnostic alternative to biopsy.
CI: confidence interval.
The PPV and NPV for colposcopy in discriminating CIN 2–3 from CIN 1 was 85.3% and 69.7%. Durdi et al.7 estimated a PPV of 77.0% and 95.8%, with CIN 1 and CIN 2 as disease thresholds. These estimates were relatively comparable, especially when CIN 2 was applied as the disease threshold. On the contrary, the study yielded higher NPVs, of 93.5% and 98.5%. Aue-Aungkul and Suprasert7 estimated higher PPV and NPV of 89.0% and 86.0%. The authors’ study estimates that, following a positive colposcopic classification of CIN 2–3 on a patient, there is an 85.3% chance that the patient is in CIN 2–3 stage. It further estimates that, given a colposcopic classification of CIN 1 on a patient, there is a 69.7% chance that the patient is in the CIN 1 stage of cervical cancer. This revelation is in agreement with the conclusion from a prospective, cross-sectional trial on the evaluation of RCI as a predictor of cervical intraepithelial lesion. Using a sample of 125 females aged >20 years, who were scheduled for a colposcopy at Chiang Mai University Hospital, Thailand, between August 2008–May 2014, the study concluded that the predictive accuracy of colposcopy increased with the increasing severity of the disease.8
Verma et al.8 also estimated the diagnostic accuracy of colposcopy, using RCI, to be 98.4%. This is much higher compared to 80.3%, which is the estimated diagnostic accuracy of colposcopy in discriminating CIN 2–3 from CIN 1 in this study. The authors’ study showed that colposcopy had a 80.3% chance of correctly classifying CIN 2–3 and CIN 1. This also means that it had a 19.7% chance of misclassifying CIN 2–3 as CIN 1, and vice versa. The odds of a positive CIN 2–3 test in those with disease was 13.491 times that of the odds of a positive CIN 2–3 test in those without disease. This further confirms that colposcopy has a higher chance of returning a positive CIN 2–3 among patients with CIN 2–3, as opposed to those who are not in that stage.
The Youden’s Index associated with colposcopy, using RCI to discriminate between CIN 2–3 and CIN 1, was 0.551 (0.301–0.748). This was relatively fair, as the Youden’s index can only take values between 0–1, signifying poor and good diagnostic tests. The number needed by colposcopy to differentiate between CIN 2–3 and CIN 1 was 1.182. The authors’ study, therefore, showed that colposcopy needed, at the utmost, two patients for it to correctly discriminate CIN 2–3 from CIN 1. This is a relatively good performance for a diagnostic test. This study also estimated an optimal Youden’s Index value of 0.776, with a true positive rate of 69.8%, and a false positive rate of 14.6%. This is synonymous to a sensitivity of 69.8%, and specificity of 85.4%. This also means that in a situation where an investigator deems both sensitivity and specificity as diagnostically important and desirable, the best performance of colposcopy would be noticed at these specificity and sensitivity thresholds.
This study also estimated a positive and negative likelihood ratio of 2.824 (1.779–4.483) and 0.209 (0.122–0.359). The platelet-to-lymphocyte ratio is an important estimate in diagnostics, because it gives the change in odds of having a diagnosis in patients with a positive test. This study revealed that there was a 2.824-times increase in the odds of having CIN 2–3 in a patient who was classified as having CIN 2–3 by colposcopy technique. These odds show that colposcopy has some discriminating ability on CIN 2–3 and CIN 1, hence it is informative. A platelet-to-lymphocyte ratio of 1 would mean the odds of a patient having CIN 2–3 do not change, whether colposcopy classifies them as CIN 2–3 or CIN 1.
On the other hand, the neutrophil-to-lymphocyte ratio (NLR) defines the change in odds of having a diagnosis in patients who produce a negative test. The NLR of 0.122 indicates an 8.3-times decrease in the odds of having CIN 2–3, in a patient who has been classified as having CIN 1 by colposcopy technique. The smaller the value of the NLR, the more informative the test is. An NLR of 0.122 further shows that colposcopy is an informative diagnostic alternative for biopsy.
CONCLUSIONS
There were nearly equal proportions of intermediate and high Grade disease when modified RCI was used to classify colposcopy findings. Histopathology reported that more than half of all the findings were high Grade disease (CIN 2/CIN 3). Finally, this study reports that there is an association between the discriminatory power of the two methods; however, colposcopy had a lower specificity when compared to histopathology.







