Abstract
Introduction: Some of the factors that may be associated with and influence vaginismus and female sexual function have already been studied, such as repressive education, religious teaching, cultural values, and anatomical changes; however, no studies exist that have analysed the measurement between the external urethral orifice and the vaginal introitus in the search for differences between women with and without the diagnosis of vaginismus.
Objective: To verify the urethro-vaginal anthropometric relation in women with and without vaginismus.
Method: This was a cross-sectional study, approved by the Ethics Committee and registered in clinical trials, conducted from February to August 2017. Sixty women were evaluated, aged 18–40 years old and all of whom were nulliparous, heterosexual, and sexually active. They were divided into two groups: Group I (women with vaginismus, n=30) and Group II (without vaginismus, n=30). Using an inelastic tape measure, the distance between the external urethral orifice and the inferior border of the vaginal introitus was checked in both groups.
Results: In Group I, the mean distance between the urethral orifice and the inferior border of the vaginal introitus was 0.69 cm. In Group II, the mean was 1.46 cm, with p<0.001 demonstrated in the comparison for the difference between the groups.
Conclusion: A significant difference was observed in the distance between the external urethral orifice and the inferior border of the vaginal introitus in women with and without vaginismus. This anatomical finding may be involved with the evolution of vaginismus.
INTRODUCTION
Vaginismus is a female sexual dysfunction with a multifactorial aetiology, and is characterised by recurrent or persistent involuntary spasm of the perineum muscles, which are adjacent to the lower third of the vagina. This condition prevents penetration, whether by penis, finger, or other object, which has a negative impact on sexual relations and quality of life.1-4
Despite the lack of epidemiological studies that define the prevalence of vaginismus, it is clinically estimated between 5–20%.1,2 However, it is known that many women do not look for medical treatment because of fear, lack of confidence, discomfort, or lack of knowledge. According to this perspective, the population affected by vaginismus is likely to be underestimated.5-7
In the Diagnostic and Statistical Manual of Mental Disorders (DSM-5),6 vaginismus is grouped with the disorders of pelvic pain/penetration and can be presented as a disease that arises throughout life: this means that it either presents following first sexual experience or is acquired. In the International Classification of Diseases (ICD-11), approved by the World Health Organization (WHO) in 2018 and pending implementation in January 2022, the disease is denoted as a sexual disorder of the pain penetration (HA20.Z).7,8
The aetiology of vaginismus has not yet been well elucidated; however, it is known that factors such as sexual, cultural, religious education, previous sexual experiences, violence, or sexual abuse contribute or enhance its development.9,10 These physical and/or psychological factors have been studied and appear to act through a vicious cycle of fear and avoidance, in which attempts of penetration causes distress and muscular tension, leading to greater avoidance and, thus, a relentless fear of penile penetration.8
There is also a need for investigation into anatomical changes, organic diseases such as abnormalities in the hymen, infections, vaginal lesions, and endometriosis, all of which cause pain or difficulty in penetration and have been suggested as additional aetiological factors.11
When the authors investigated studies that had extensively evaluated vaginismus, specifically focussing on anatomical alterations, reports about the relation between the urethra and the vaginal introitus were not found in the literature. This finding could constitute a mechanical barrier that is feasibly linked to the development of vaginismus.
OBJECTIVE
To verify the urethro–vaginal anthropometric relationship of women with and without vaginismus.
METHOD
This was a cross-sectional study, approved by the Ethical Committee (CAAE: 51995515.4.0000.5479) and registered in clinical trials (NC03176069),12 conducted from February to August 2017, evaluating 60 women aged 18–40 years old who were nulliparous, heterosexual, and sexually active.
The women were divided into two groups: Vaginismus Group (n=30) and Control Group (n=30), the latter composed of women without sexual dysfunction. Included in the Vaginismus Group were those with vaginismus throughout their lives and classified as having severe degree (DSM-5).6 They had never been through any treatment or intervention for sexual dysfunction. The authors excluded women that had psychiatric disease, primigravida and multigravida, partners with dysfunction that prevented penetration, presence of vaginal prolapse, or surgical necessity for vaginismus.
All participants were recruited through social media, and those who responded to the call were interviewed by an independent researcher who made the telephone contact to observe the inclusion criteria. An evaluation was scheduled for those who met all the criteria.
The evaluation took place in a University Hospital and was performed by a physiotherapist specialised in pelvic physiotherapy. The women were evaluated by the same examiner who was unaware of their allocation (Vaginismus Group or Control Group). Evaluations were performed with the participants in the gynaecological position, with an inelastic tape measure. The distance between the external urethral orifice to the inferior border of the vaginal introitus was measured in the two groups, as exemplified in Figure 1. The data were analysed for statistical significance by SPSS software. The Mann–Whitney test was performed. The level of significance was 5%.
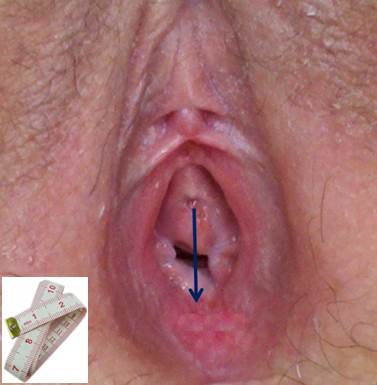
Figure 1: Illustrative image of the measurement of the distance between the external urethral orifice and the lower border of the vaginal introitus.
RESULTS
In Table 1, the characterisation of the women studied in the Vaginismus Group and in the Control Group is described according to several variables: age, BMI, age of menarche (years), beginning of sexual life (years), marital status, and religion.
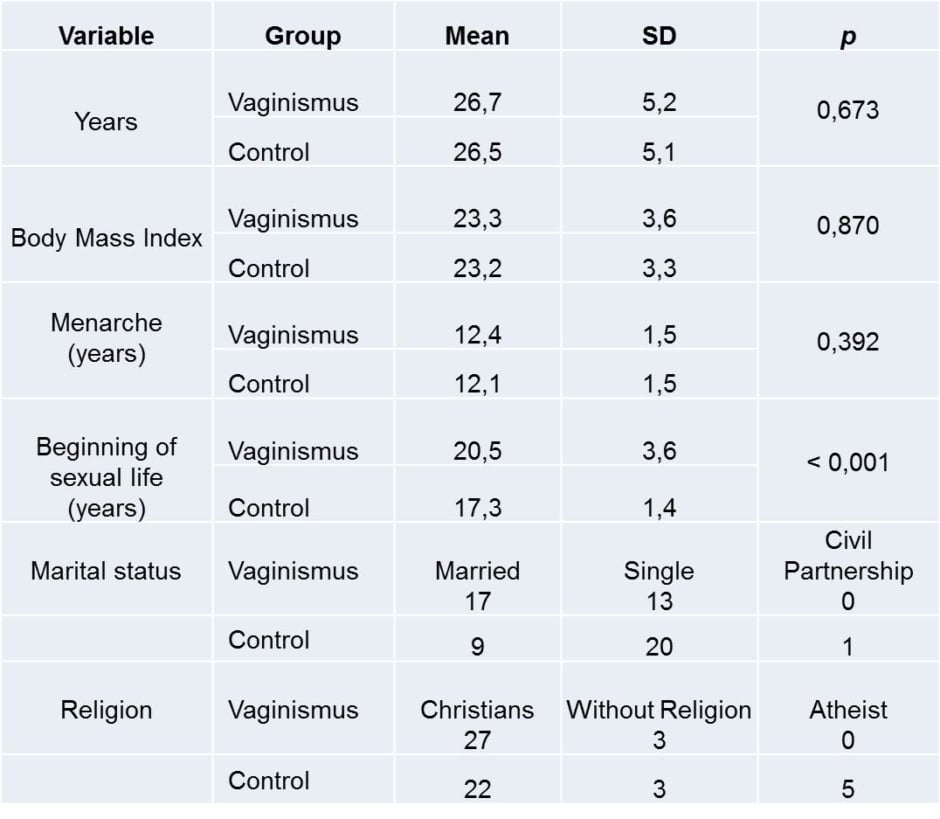
Table 1: Characterisation of the sample of the Vaginismus Group (n=30) and Control Group (n=30).
SD: standard deviation.
Table 2 shows the measurements between the external urethral orifice and the inferior border of the vaginal introitus (cm) of the Vaginismus Group and of the Control Group. The mean distance in the Vaginismus Group was 0.69 cm (standard deviation [SD]: 0.28). The mean distance in the Control Group was 1.46 cm (SD:0.20; p>0.001).
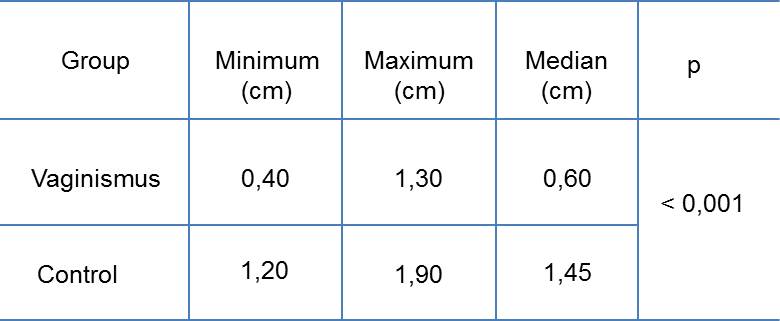
Table 2: Measurements of the external urethral orifice to the lower border of the vaginal introitus of the Vaginismus Group (n=30) and of the Control Group (n=30).
DISCUSSION
Vaginismus is a multifactorial sexual dysfunction that encompasses emotional, psychological, biological, and possibly anatomical factors. Women with vaginismus suffer significant impact on their quality of life. Congenital malformations of the genitourinary tract or changes in the hymen are reported in the literature as possible risk factors for vaginismus.13,14
In the authors’ practice, the differentiated positioning of the urethra of women who present the diagnosis of vaginismus in relation to women without sexual dysfunction was clinically observed, suggestive of a ‘low urethra’ that sometimes overlaps with the vaginal introitus. The authors did not, however, find scientific studies in the literature that investigate this difference. This study focussed on answering the following question: is there a difference in the measurement between the external urethral orifice and the vaginal introitus?
The presence of a bigger mean distance between the external urethral orifice and the hymenal meatus was described as a finding in women who had urethral–hymenal fusion. This urethral-hymenal fusion is considered a congenital predisposition for frequent episodes of cystitis after sexual relation.15 In this study, a decrease in the measurement between the external urethral orifice and vaginal introitus was observed.
Gravina et al.13 related the location of the urethra to the quality/capacity of female orgasms. The urethrovaginal space consists of fibroconnective tissue and large numbers of blood vessels, glands, muscle fibres, and nerve endings. The proximity of the urethra and the clitoris to the anterior vaginal wall suggests an association between such anatomical structures and sexual function. In women without sexual dysfunction, a relationship between the urethra–vaginal distance and the presence of orgasm was described by ultrasonography. The present study was not intended to evaluate the phases of the human sexual response cycle; however, the clinical finding that showed the lowest urethrovaginal space may lead to the development of a new line of research that uses ultrasonography to evaluate in the same way conducted by Gravina et al.,13 allowing a comparison of results.
Anatomical differences are important conditions that can influence sexual function. There are few articles that correlate these differences with sexual function, or even with some sexual dysfunctions. They are insufficient to establish a consensus. Regarding vaginismus, the authors did not find studies in the literature that relate the measurement of the external urethral orifice to the vaginal introitus. Thus, this study may be the precursor of an important diagnostic relationship. Associating anatomical differences with psychological and emotional factors may lead to a better understanding of vaginismus.
Regarding the question “is there a difference in the measurement between external urethral orifice and the vaginal introitus?”, which motivated the present study, these results suggest that the answer is yes. A measure up to three times smaller between the anatomical structures analysed between the groups was observed. This result leads the authors to suggest some hypotheses: did this difference of measure arise after the development of vaginismus, due to recurrent spasms, or did it already exist?; does this measure change after the physiotherapy treatment for vaginismus? If this measure is related to an anatomical change, it would be advisable that the gynaecologist evaluated this measure at the woman’s first consultation. This is because, according to the present study, this measure may suggest a risk factor for the development of vaginismus. Among the possible causes for this difference, the literature does not yet present a hormonal correlation, especially relating gestation to the development of vaginismus. The desire to carry children is one of the reasons women seek treatment for vaginismus. Another factor to be investigated in future studies is the relationship of perineal muscle tone with vaginismus, specifically the urethro—vaginal distance, because there is spasm of this musculature for acquired or congenital vaginismus. The authors confirm, however, that the finding of the present study may suggest a risk factor for development and generate a deeper line of research on the subject.
CONCLUSION
According to the data obtained, a significant difference was observed in the distance between the external urethral orifice and the inferior border of the vaginal introitus when women with and without vaginismus are compared. This anatomical finding may be related to the evolution of vaginismus.








