Interviewee: Elena Labarta
Gynecologist and specialist in human reproduction, IVI RMA Valencia, Spain
Disclosure: Dr Labarta received a grant from Finox in 2016, has provided consultancy services for Ferring Pharmaceuticals and MSD, and is part of the Ferring Pharmaceuticals LIFE programme. During the past 12 months, she has received honoraria from Angelini/IBSA, MSD, and Ferring Pharmaceuticals for lecturing.
Support: The publication of this feature interview was supported and reviewed by IBSA Institut Biochimique SA.
Acknowledgements: Medical writing assistance was provided by David Jacobs of Lewis-Barned, West Sussex, UK.
Disclaimer: The opinions expressed in this article belong solely to the named interviewees.
Citation: EMJ Repro Health. 2019;5[1]:34-37. DOI/10.33590/emjreprohealth/10312233. https://doi.org/10.33590/emjreprohealth/10312233.
At the end of December 2017, some colleagues and I reported results from a prospective cohort study (N=211) into the relationship between serum progesterone (P) and endometrial volume on the day of embryo transfer (ET) and ongoing pregnancy rates (OPR) in artificial endometrium preparation cycles.1
Progesterone Deficiency – A Minimum Threshold Level
Our study found that patients with serum P <9.2 ng/mL on the day of ET had a significantly lower OPR; but that endometrial volume was not related to OPR.1 The implication is that, if outcomes are to be optimised, a minimal threshold of serum P values on the day of ET must be reached.
Until our study it was thought that the level of serum P would not reflect its effect in the uterus as there was no direct correlation between blood and uterine P levels.2
However, there were some limitations to this initial study. Only women with a healthy uterine cavity and appropriate endometrial thickness were included. A further study was needed. At ESHRE 2019, we were delighted to present our findings from a new investigation of 1,197 non-selected patients3. Our preliminary findings appear to be in line with the first study.1
There are some clear implications for current clinical practice; we found there was a minimum threshold of serum P below which the chance of having a live birth was decreased by around a fifth.3
Management of Luteal Phase Support – The Individualised Modern Approach
Although serum P is not the only predictor of implantation failure – there are other factors related to the success of the cycle4 – the results demonstrate the importance of measuring serum P at ET. We now do this at our practice as a matter of routine. In this way, we can detect which patients have adequate levels of P, essential for embryo implantation and pregnancy maintenance. Until now, it was thought that a conventional dose would be sufficient for all patients during the luteal phase. However, it has become clear that many patients require individualised luteal phase support (LPS); by routinely measuring serum P levels, we can detect which patients need raised P in order to optimise their pregnancy rates. In fact, we found that 30% of women showed inadequate levels of serum P after receiving the standard dose of vaginal P.3
The Addition of Subcutaneous Progesterone
Vaginal P via capsule, gel, or tablet is the most common route for LPS support in Europe.5 In a retrospective analysis conducted at our centre (IVI RMA Valencia, Spain), which included almost 1,700 patients, we observed that by adding subcutaneous (sc) P to the vaginal administration for patients with low serum levels, we could overcome P deficiency and therefore deliver similar results to those patients with adequate levels.
We chose to administer sc P for a number of reasons: increasing the vaginal dose might increase the vaginal discharge (patients were already receiving four tablets per day); and the sc route to P supplementation could overcome the possibility of poor absorption by the vaginal route, where P is rapidly absorbed into the epithelium and endometrium and thus prevented from entering into circulation.2 sc P, on the other hand, has been shown to very rapidly increase the levels of serum P6 (see Figure 1). Herein lies the importance of pursuing alternative administration routes for P, especially considering the lack of positive correlation between vaginal administration and circulating blood levels.
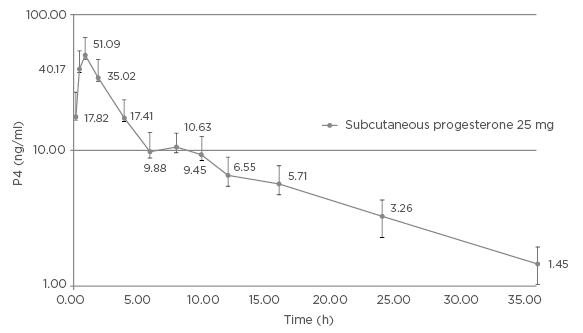
Figure 1: Mean (+SD) baseline corrected plasma progesterone concentrations (ng/mL) versus time profiles after single dose administration of subcutaneous progesterone 25 mg to 28 post-menopausal women. (Semi-log scale).
Reproduced by permission of IBSA Institut Biochimique SA
Observed Benefits of Administering Subcutaneous Progesterone
We observed that almost all patients increased their levels of serum P when adding sc P; it is known that patients with pregnancy-related vaginal bleeding have significantly lower serum P levels. Furthermore, no additional procedural risks were detected using the sc method. It has yet to be demonstrated whether other ways of administering increased doses of P are as effective.
As well as the apparent difference this technique has made to pregnancy outcomes, we observed that patients appear to feel more confident in us as clinicians. We hypothesise that this is because by bringing more control to the procedure we are able to improve their results.
GREATER PREDICTABILITY
We can predict quite accurately whether patients are going to have low serum P levels; in 80.5% of cases, patients show similar results in a second cycle when using the same doses of exogenous P.7
MAINTAINING THE SUCCESS RATES OF IN VITRO FERTILISATION CLINICS
We have seen that individualising the LPS in patients with inadequate exposure to exogenous P, by increasing the dosage using sc administration of water-soluble P, can overcome low serum levels and normalise pregnancy rates. Such improvements are essential if we are to maintain the success rates of in vitro fertilisation clinics. Using this strategy in our clinic, those patients who showed a smaller chance of having a baby due to low serum P levels have been able to improve their results significantly – this is an outstanding finding (Figure 2).
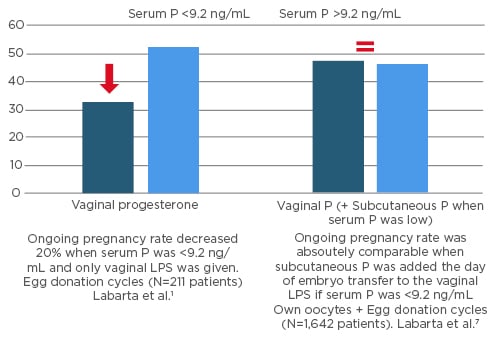
Figure 2: Ongoing pregnancy outcome according to serum progesterone levels on the day of embryo transfer.
LPS: luteal phase support; P: progesterone.
Biographies
Elena Labarta Gynecologist and specialist in human reproduction, IVI RMA Valencia, Spain
Dr Labarta has worked at IVI Valencia since 2005. She has participated as a researcher in numerous clinical research projects, including Phase II and Phase III clinical trials, and has published many scientific articles and book chapters based on the field of in vitro fertilisation. She is a frequently invited lecturer in the most relevant meetings. Dr Labarta’s research is now focussed on the predictive value of mid-luteal serum progesterone levels in egg donation cycles; ovarian stimulation and embryo quality; use of 3D ultrasound for uterine evaluation in infertile patients; and the impact of autologous mitochondrial transfer on oocyte and embryo quality in in vitro fertilisation patients, among others.








