Abstract
Purpose: Dynamic contrast-enhanced (DCE)-MRI has a promising role in breast cancer detection and lesion characterisation. Diffusion-weighted imaging (DWI) acts as an adjunct in the differentiation between benign and malignant lesions. The purpose of the study was to evaluate the efficacy of DCE-MRI and DWI in differentiating benign and malignant lesions.
Methods: In a prospective study conducted between March 2019 and February 2020, 60 patients with breast lesions underwent DWI combined with DCE-MRI of the breast. The time–intensity curves were plotted. Lesions were classified according to the latest American College of Radiology Breast Imaging Reporting and Data System (ACR BI-RADS; 5th edition). The results were compared with the histopathological diagnosis. The sensitivity and specificity of DWI, DCE-MRI, and combined DWI and DCE-MRI were calculated for detection of benign and malignant breast lesions.
Results: Sixty patients underwent breast MRI in which 78 lesions were detected, out of which 28 were benign and 50 were malignant. Quantitative apparent diffusion coefficient measurement revealed 96% sensitivity and 82% specificity, with a positive predictive value of 92% and negative predictive value of 96%, for differentiating benign from malignant lesions. DCE-MRI findings showed 96% sensitivity and 78.5% specificity. The sensitivity of combined DWI and DCE-MRI was 98% and specificity was 86%, which was higher than DWI and DCE-MRI alone.
Conclusion: Multiparametric MRI of the breast has very high sensitivity for detecting and characterising breast lesions as benign or malignant lesions. DWI had higher specificity than DCE-MRI, and the combined use of DWI and DCE-MRI had greater efficacy than DWI and DCE-MRI alone.
INTRODUCTION
Breast cancer is a leading cause of morbidity as well as mortality. It remains a matter of interest for both clinicians and investigators. Increased understanding, regular physical check-ups, and diagnostic radiological procedures have resulted in a timely diagnosis of carcinoma of the breast and have resulted in improvement in the prognosis of malignancies of the breast.1-3 Early diagnosis of breast cancer is essential for a more conservative surgical approach towards management of the disease. The triple assessment protocol has been established as a diagnostic protocol for the management of palpable masses of breast; the triple assessment consists of regular physical check-ups, radiological investigations, and histopathological examination.4
Although ultrasound breast is a well-recognised modality for the detection of breast pathologies, various studies have shown that dynamic contrast-enhanced (DCE)-MRI has a promising role in the detection of various breast masses, along with characterisation of the lesion.5,6
In addition to DCE-MRI, the use of diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) values help to distinguish benign breast lesions from malignant breast lesions; they also aid in early detection and diagnosis of the breast malignancies. Therefore, DWI can also be used to detect carcinoma of the breast without injecting contrast or as an adjunct to it, specifically for patients with deranged renal function tests or prior history of contrast reactions.7
MRI offers accurate visualisation of posterior breast tissue, axillary lymph node involvement, multiplicity in the same as well as opposite breast, and can assess contiguous involvement better than conventional imaging, so aids preoperative imaging of carcinomas.
PURPOSE
The purpose of this study was to evaluate the efficacy of DWI and DCE-MRI in differentiating benign and malignant breast lesions.
METHODS
A prospective, single-centre, observational study was conducted of 60 patients who had a clinically palpable breast lump or mass lesion detected on breast ultrasound breast March 2019 to February 2020, after obtaining approval from the institutional ethics committee/review board. Informed and written consent was taken from each patient. Female patients who presented with a breast lump on self-examination or clinical examination, or those with lesion detected on ultrasound breast, were part of the study group in the present study. Patients with contraindications to MRI and those with a history of allergic reaction to contrast media were not included. Patients with any history of previous interventional procedure or any surgery in the 3 months preceding the examination were also not included in the study.
Breast MRI
All the patients included in the study group had MRI examination with Achieva dStream 1.5T MRI (Philips, Amsterdam, the Netherlands). The dedicated breast coil was used. All metallic objects related to the patients’ bodies were removed. Intravenous access was secured for gadolinium contrast injection. The patients were instructed to lie in prone position and both breasts were placed into the breast coil. Both the breasts were placed deep and centrally in the coil, with the nipple facing downwards. Patients were advised to stay immobile until the completion of scan.
The standard imaging protocol included:
- T1-weighted pulse sequence. Axial and coronal non-fat-saturated T1-weighted images were acquired by turbo spin echo imaging, by using the subsequent imaging parameters: repetition time (TR) 425–475 ms, echo time (TE) 14–18 ms, and field of view (FOV) 200×340 mm2 for axial and 300×379 mm2 for the coronal plane.
- Short T1 inversion recovery (STIR). Axial and coronal STIR images were obtained with the following imaging parameters: TR 3,500–4,500 ms, TE 70–90 ms, and FOV 200×340 mm2 for axial and 300×379 mm2 for coronal plane.
- DWI. DWI was obtained before DCE-MRI. ADC values were obtained using b values at 0, 350, 700, and 1,000.
- Dynamic study. All dynamic studies were performed in the T1-weighted sequences by applying fat-saturated pulses. Dyn thrive was used for contrast-enhanced images with the following parameters: TR 450–500 ms, TE 40–50 ms, and FOV 200×340 mm2. DCE-MRI study was conducted by injecting 5–8 mL of gadolinium chelate (Gadovist®, Bayer, Leverkusen, Germany) intravenously followed by 10 mL of normal saline. Kinetic curves were obtained based on the DCE-MRI study. Dynamic study consisted of one precontrast and five postcontrast series; each of the sequences was captured in approximately 45 seconds, with an approximate time gap of 20–40 seconds between the pre- and postcontrast sequences as well as the individual postcontrast sequences.
Image Post-Processing
Subtraction images were acquired by subtracting each of the precontrast images from the postcontrast images. Kinetic curves were generated for enhancing lesions and maximum intensity projection images were also generated.
Time–Intensity Curves
After administration of intravenous gadolinium contrast, three types of enhancement kinetic curves are possible for an enhancing lesion in the breast parenchyma (Figure 1):8
- Type I curve (rising enhancement pattern): typically shows a continuous increase in signal intensity throughout time. Most of the lesions are benign; only a small proportion of malignant lesions show this pattern.
- Type II curve (plateau pattern): initial uptake is followed by the plateau phase towards the latter part of the study. This pattern is suspicious for malignancy.
- Type III curve (washout pattern): initial rapid uptake, then shows washout of contrast towards the later part of the study. This pattern is strongly suggestive of malignancy.
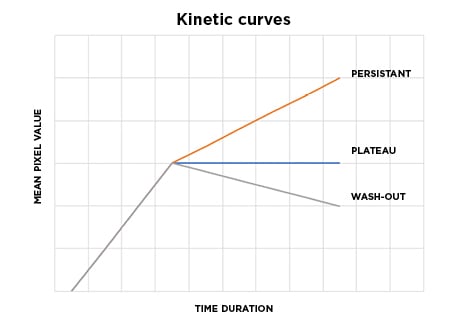
Figure 1: Diagrammatic representation of the types of kinetic curves according to wash-out patterns in dynamic contrast-enhanced MRI study.
MRI Image Analysis
Initial detection of the lesions was first completed on STIR images. Morphologic characteristics (shape and margins) of all detected lesions were analysed on STIR and T1-weighted images. The enhancement characteristics of the lesions were assessed on DCE-MRI by plotting the kinetic enhancement curves, which were characterised as kinetic curve Type I, kinetic curve Type II, or kinetic curve Type III on the basis of their delayed-phase enhancement.
DWI characteristics and corresponding ADC values were evaluated using b values of 0, 350, 700, and 1,000. The region of interest was chosen for the part of the lesion that demonstrated the highest signal intensity on DWI image. ADC value of ≤1.1×10-3 mm2/sec was taken as the cut-off value for diffusion restriction.
American College of Radiology Breast Imaging Reporting and Data System (ACR BI-RADS; 5th edition) lexicon criteria were used to classify lesions that were detected on MRI breast. Two certified radiologists with 10 years of experience in MRI simultaneously evaluated the MRI findings. Percutaneous core needle biopsy was performed in the patients with lesions labelled as BI-RADS ≥3 according to the study protocol and were taken as gold standard. Biopsies were performed within 30 days of the breast MRI in all cases. The lesions that were classified as BI-RADS 2 and 3 were considered benign lesions, while the lesions classified as BI-RADS 4 and 5 were considered to be malignant. The MRI findings were also compared with the histopathological findings.
Statistical Analysis
The lesions that were classified as BI-RADS 4 or 5 were considered as a positive test (MRI evaluation) result, while the lesions that were classified as BI-RADS 2 or 3 were considered as a negative test (MRI evaluation) result. The sensitivity and specificity of DWI and DCE breast MRI were calculated in the detection and diagnosis of cancerous lesions of the breast. Positive predictive value and negative predictive value were also calculated.
Statistical assessment was carried out using SPSS® 23.0 version (IBM®, Armonk, New York, USA). Chi-squared test was used to find connotation in categorical data. A probability threshold of 0.05 was considered as noteworthy.
RESULTS
The present study included 78 breast lesions among 60 female patients with ages ranging from 25 to 73 years. The mean age of those with benign breast lesions was 31 years and of those with malignant breast lesions was 46 years. All the cases (BI-RADS ≥3) were confirmed by percutaneous core needle biopsy.
The malignant lesions were most common in the upper outer quadrant (42%), followed by the upper inner quadrant (20%). These were followed by the lower outer quadrant (20%) and lower inner quadrant (14%). Only 4% of the lesions were detected in the retroareolar region.
The description of MRI breast findings was completed using the latest ACR BI-RADS lexicon, which included the basic morphological criteria (shape, margin, enhancement, and kinetic curve). On MRI breast, 22 benign lesions (78.5%) were categorised as BI-RADS 2 and 3. Only six benign lesions were categorised as BI-RADS 4. Fifty malignant lesions (100%) were characterised as BI-RADS 4 and 5 (P=0.001).
Contrast enhancement was assessed following gadolinium contrast injection and time–intensity curves were evaluated. Type I enhancement kinetic curve (rising curve) was noted in 20 benign lesions (71.4 %) and none of the malignant masses. Type II enhancement kinetic curve (plateau curve) was observed in only two benign lesions (7.1%) and two malignant lesions (4.0%). Type III enhancement kinetic curve (washout curve) was noted in six benign lesions (21.4%) and 48 malignant lesions (96.0%) (P=0.001).
DCE-MRI findings showed 96% sensitivity and 78.5% specificity, whereas quantitative ADC measurement revealed a sensitivity of 96% and specificity of 82%, and a positive predictive value of 92% and negative predictive value of 96%. The sensitivity of combined DWI and DCE-MRI was found to be 98% and specificity was 86%.
The determination of final ACR BI-RADS category of each lesion was made including all the above criteria.
DISCUSSION
Breast MRI is well known for its high capability and increased potential for the detection of breast masses. However, MRI breast is an expensive imaging modality, and it cannot be used in patients who have contraindications to MRI or any history of reaction to intravenous contrast media.
Lee9 conducted a study that found that breast cancer is more frequently detected in the upper outer quadrant of the breast, which might be because more breast parenchymal tissue is present in the upper outer quadrant or because of the overuse of underarm cosmetics. In the present study, it was also found that the malignant lesions were more common in the upper outer quadrant.
In the present study, it was detected that the mass lesions that had well-delineated and well-defined margins were mostly benign (89.2%), whereas the lesions that had irregular and spiculated margins were diagnosed to be malignant in most of the cases (94.0%). These findings were in concordance with the study performed by Macura et al.,10 who concluded that the description of the margin of a focal lesion is one of the most foretelling characteristic features of the MRI breast analysis. They also found that irregular margins raised greater suspicion for the lesion to be malignant (Figure 2).10
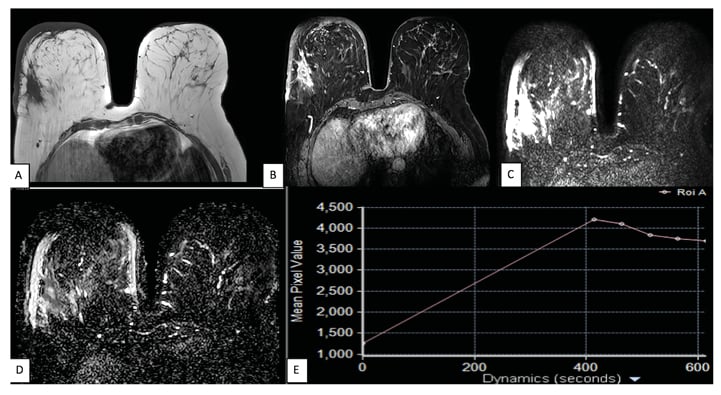
Figure 2: A 57-year-old female presented with a painless lump in the right breast, accidentally palpated 1 month prior. A and B): Axial T1-weighted and axial STIR images reveal an ill-defined, irregular-shaped lesion in the upper outer quadrant of the right breast, appearing hypointense on T1-weighted images and heterogeneously hyperintense on STIR images. C and D) DWI and ADC images show diffusion restriction, with minimum ADC value of 0.714×10-3 mm2/sec. E) Postcontrast images show heterogenous enhancement with washout type (Type III) of enhancement curve. This lesion was labelled as BI-RADS 5 and was found to be invasive ductal carcinoma on histopathology. ADC: apparent diffusion coefficient; DWI: diffusion-weighted imaging; STIR: short T1 inversion recovery.
The internal enhancement characteristics of a focal mass lesion are one of the most efficient diagnostic measures for the differentiation of benign lesions from malignant lesions, as described by Rausch et al.11 Shah et al.12 also concluded that heterogeneous internal enhancement was the most commonly seen morphological finding among all the studied malignant lesions. In the present study, 47 of the enhanced lesions showed heterogeneous postcontrast enhancement on DCE-MRI, with the majority turning out to be malignant (90%; Figure 3).
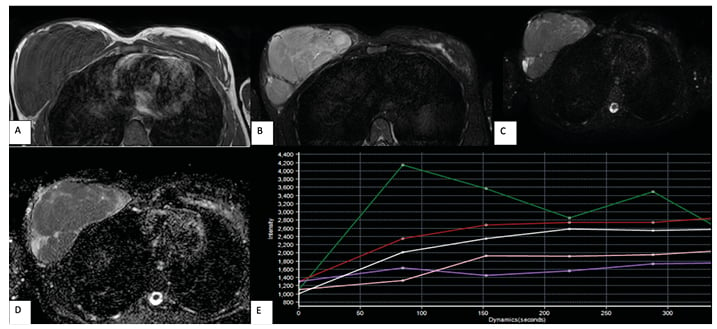
Figure 3: A and B) Axial T1-weighted and axial STIR images reveal a well-defined, lobulated mass lesion replacing the right breast parenchyma, appearing hypointense on T1-weighted images and heterogeneously hyperintense on STIR images, showing internal septations. C and D) DWI and ADC images reveal no restriction of diffusion. E) Postcontrast images show homogeneous enhancement with a rising type of enhancement curve (Type I; red and white curves; green curve represents normal vascular enhancement). This lesion was labelled as BI-RADS 3 and was found to be atypical ductal hyperplasia on histopathology. ADC: apparent diffusion coefficient; DWI: diffusion-weighted imaging; STIR: short T1 inversion recovery.
Along with precisely describing the morphological characteristics of the lesion, MRI also determines the dynamics of the contrast medium by forming the signal intensity curve, signifying the degree of vascularity inside the lesion.
In the present study, Type I enhancement kinetic curve (rising curve) and Type II enhancement kinetic curve (plateau curve) were seen in 22 benign lesions (78.6%). Type III enhancement kinetic curve (rapid wash-in and wash-out curve) was seen in 48 malignant lesions (96%). This was in agreement with various previous research studies that described and assessed the importance of the various enhancement kinetic curves in differentiating between malignant and benign breast lesions. Imamura et al.13 reported that the use of enhancement kinetic curves of time–signal intensity resulted in markedly increased differentiation of benign from malignant breast lesions. Roganovic et al.14 also showed that the enhancement kinetic curve of a persistent type is more in favour of benign changes and a Type III wash-in wash-out curve is more in favour of malignancy, as their study showed that 86% of malignant lesions had a wash-out type of enhancement kinetic curve, 14% had a plateau type of enhancement kinetic curve, and none had a persistent type of enhancement kinetic curve.14 Most of the patients with triple-negative breast cancer in the research conducted by Azzam et al.,15 also showed malignant-pattern kinetic curves.15
In the present study, 53 lesions showed restricted diffusion, out of which 48 lesions (96%) were malignant. This is in accordance with the results of Youssef et al.,7 which proved that DWI further enhances the capability of the DCE-MRI for diagnosing breast lesions.7
The present study also analysed the ADC value using three separate b values (350, 700, and 1,000). No statistically significant difference was exhibited between the ADC values perceived at various separate b values in providing differentiation between benign and malignant breast lesions. Similar observations have been confirmed in the research work by Chen et al.,16 which showed that the conspicuity of breast lesions is not affected by varying the b values on DWI at 1.5T. Partridge et al.17 also concluded that DWI has a promising role in characterising breast lesions in breast MRI and is not considerably restricted by the size or type of the lesion.
In the present study, quantitative ADC measurement and DCE-MRI alone had almost comparable sensitivities (96.0%); however, the specificity of DCE (78.5%) was much lower than that of DWI (82.0%). The concomitant use of DWI and DCE-MRI improved both sensitivity as well as specificity of diagnosing benign and malignant breast lesions, with sensitivity of 98% and specificity of 86%, which was greater than that of DWI and DCE-MRI alone. This is in accordance with the results of the research by Kul et al.18 in which they evaluated the concomitant role of DCE-MRI and DWI as an imaging protocol in patients with suspicious breast lesions; 84 patients underwent MRI breast in their study. The efficacy of DCE-MRI, DWI, and combined MRI for diagnosis and characterisation of breast lesions were calculated. Sensitivity and specificity of ADC values in their study were 91.5% and 86.5%, respectively. DCE-MRI alone had sensitivity of 97.9% and specificity of 75.7%. The combination of DCE-MRI with DWI showed sensitivity of 95.7% and specificity of 89.2%.18 In another research work performed by El Bakry et al.,19 it was also revealed that the sensitivity for DCE-MRI alone was 91.7% and specificity was 84.2%. The DWI showed a sensitivity of 94.4% and specificity of 92.1% in their study. Sensitivity and specificity of breast MRI for the detection of breast tumours were increased in their study by the concomitant use of DCE-MRI and DWI.19
The limitations of the present study include a limited number of patients due to a relatively shorter time duration of the study. There were fewer patients agreeable to undergo MRI breast examination as a diagnostic modality who fit inclusion criteria. The main reason for this was the high cost, as well as a relative lack of awareness and knowledge about the utility of MRI for the timely detection and diagnosis of breast cancer.
CONCLUSION
Multiparametric MRI breast has very high sensitivity for detecting and characterising breast lesions as benign or malignant lesions. DWI alone has almost comparable sensitivity as compared with breast DCE-MRI; however, it is more specific. The concomitant use of DWI and DCE-MRI improved the sensitivity and specificity of breast MRI for characterising benign and malignant breast lesions, compared with DWI and DCE-MRI alone.







