Abstract
Sarcoidosis is a disorder that affects multiple systems with unclear causes and is relatively rare. The defining characteristic of this disease is the presence of granulomas in various organs in the human body. The incidence and presentation are changeable according to many factors, such as geography, ethnicity, sex, and genetic background. It is highest in Scandinavians. Löfgren syndrome represents a sudden manifestation of sarcoidosis, constituting approximately 10% of all cases. The classical signs and symptoms include bilateral symmetric hilar lymphadenopathy, fever, multiple joint swelling, and skin lesions known as erythema nodosum. Diagnosis of the disease can be quite challenging owing to its infrequent occurrence and the limited availability of sensitive and specific diagnostic tools, tests, and changeable clinical pictures that may suggest different aetiologies. Early diagnosis of Löfgren syndrome will ensure rapid treatment and fewer complications. This review presents the case of a 27-year-old healthy female with sudden onset of bilateral knee joint pain, swelling, erythema nodosum, and fever. Laboratory tests revealed elevated inflammatory parameters. Chest CT and chest X-ray revealed mediastinal and hilar lymphadenopathy, suggesting Löfgren syndrome. This report emphasises the broad spectrum of mimicry observed in cases of acute sarcoidosis, with a focus on the clinical picture and standard differentials that must be carefully evaluated to exclude other inflammatory and malignant conditions. The patient achieved full remission following symptomatic treatment.
Key Points
1. Löfgren syndrome is a rare disease with clinical manifestations similar to other syndromes. Therefore, it is a challenging diagnosis that is diagnosed by excluding other differential diagnoses.2. Presentation of the acute form of sarcoidosis and its management.
3. Early diagnosis of sarcoidosis is crucial for rapid remission and preventing serious complications.
INTRODUCTION
Löfgren syndrome is an acute form of sarcoidosis first documented by Sven Löfgren in 1953.1 Sarcoidosis is an idiopathic multisystem autoimmune disorder in which the immune system reacts abnormally to unknown triggers to form granulomas and small clumps of inflamed cells.2 The typical manifestations of this condition primarily target the pulmonary and thoracic lymph nodes but can also extend to the integumentary system, ocular structures, hepatic tissue, cardiac muscle, and nervous system. It occurs most often in adults aged between 20–39 years.2 Sarcoidosis is a relatively rare disease, with an annual incidence rate of 11.5 per 100,000 people in northern Europe, with a higher tendency for sarcoidosis in women than in men.3
Löfgren disease is a frequent presentation of acute sarcoid arthritis, occurring in approximately 5–10% of sarcoid cases.2 The clinical manifestations of sarcoidosis vary depending on the organ involved. The usual clinical features include long-lasting cough, dyspnoea, chest pain, tiredness, fever, weight loss, skin lesions, eye inflammation, and joint or muscle pain.4 Unlike the often reported slow progressive course of sarcoidosis, Löfgren syndrome usually presents with an acute breakthrough of signs and symptoms, including the sudden onset of erythema nodosum, bilateral symmetric hilar lymphadenopathy, fever, and multiple joint swellings.2 Difficulty breathing, dry coughing, and chest pain can occur due to inflammation of the lungs. In addition, patients may experience pain and swelling in the ankles, redness, soreness of the eyes, sore throat, and general fatigue.1,2
Diagnosing Löfgren disease involves a combination of the patient’s symptoms, physical examinations, imaging modalities, blood tests, and biopsies. It is important to rule out other similar diseases to provide proper treatment as the symptoms may resemble those of other malignant and inflammatory conditions.3,4 The majority of individuals diagnosed with Löfgren syndrome experience full and spontaneous recovery, while a subset of patients may require the use of steroids and immunosuppressive drugs to achieve remission.1 Chronic sarcoidosis is considered in patients with active symptoms for more than 2–5 years. In some chronic patients, about 10–20% may develop complications due to permanent scarring, especially in the lungs, which leads to pulmonary hypertension.
CASE PRESENTATION
A 27-year-old otherwise healthy female who smoked 1.75 pack-years, presented with a sudden onset of swelling and erythema nodosum around the ankles that extended to both legs for 1-month duration and was accompanied by a feeling of fever. The patient also experienced pain in the ankles, knees with right-sided predominance, and elbows. In addition, the patient had a mild rash under the left eye, irritation, dry throat, and dry cough especially in the morning, chills, pronounced night sweats, and fatigue throughout the course. No weight loss, itching, chest pain, or palpitations were noted. The patient had no family predispositions to any specific disease. Blood tests have shown high inflammation parameters with C-reactive protein (CRP) of 98.3 mg/L (normal: 8–10 mg/L), leucocytosis of 16,000 /µL (normal: 4,000–11,000 /µL) with 85.2% neutrophils, IgM 2.68 g/L (normal: 0.8–3.9 g/L), P.interleukin-2: 5,356 kU/L (normal: 158–623 kU/L), and angiotensin-converting enzyme (ACE) 98 U/L (normal: 12-60 U/L). Spirometry showed a forced vital capacity of 3.71 (93%), forced expiratory volume in 1 second of 3.12 (90%), forced expiratory volume in 1 second/forced vital capacity of 84.4, and diffusion capacity of the lungs for carbon monoxide of 70. Initially, chest radiography revealed bilateral hilar lymphadenopathy with no signs of calcification (Figure 1).
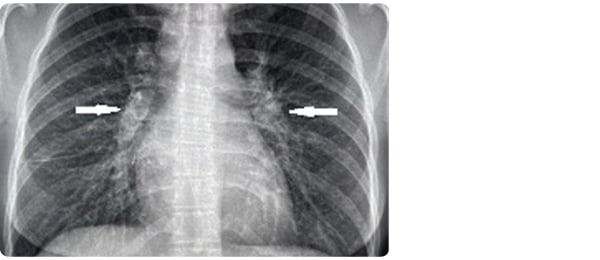
Figure 1: Chest X-ray showed bilateral hilar lymphadenopathy with no signs of calcification.
A CT scan was performed for further diagnosis and exclusion of other conditions, showing mediastinal and hilar lymphadenopathy without classifications and multiple small nodules in the lungs (Figure 2 and 3). There was no pleural effusion, lung or soft tissue tumour, or pathology in the thoracic bone cage. A definitive diagnosis is achieved by clinical assessment and exclusion of other alternative diagnoses. The patient got ibuprofen 600 mg three times daily and paracetamol 1,000 mg four times daily, with good symptomatic relief. After fluctuating between 50 and 100, CRP decreased to 13.1 mg/L. After 5 weeks, IL-2 reduced to 2,389, as well as leukocytes to 7,000/µL and ACE to 97 U/L, with almost full remission of symptoms. The patient was discharged and scheduled for follow-up for 3 months.
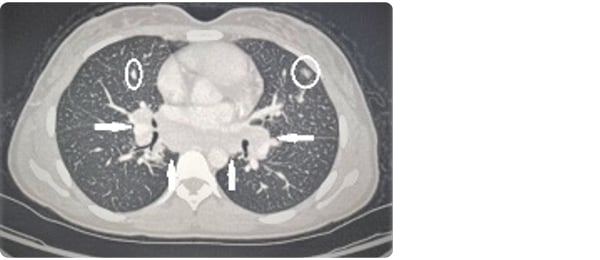
Figure 2: Axial CT scan showing mediastinal and hilar lymphadenopathy without classifications as well as multiple small nodules in the lungs.
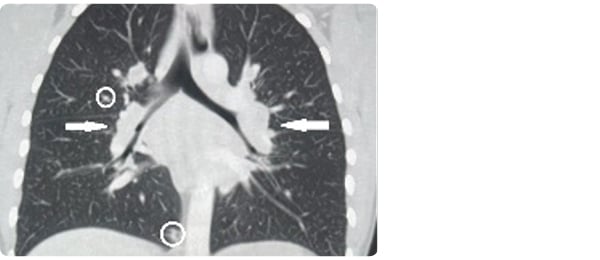
Figure 3: Coronal CT scan showing mediastinal and hilar lymphadenopathy without classifications as well as multiple small nodules in the lungs.
DISCUSSION
The diagnosis of Löfgren syndrome can be challenging because its symptoms and findings can vary considerably.3,4 Bilateral lymphadenopathy, erythema nodosum, fever, and polyarthritis are the main symptoms of Löfgren syndrome. It is challenging to make the diagnosis, which is made by ruling out other possible differential diagnoses, because the clinical manifestations of fever, joint pain, and erythema nodosum are not limited to sarcoidosis, as they can be induced by various other stimuli, such as penicillin, sulfa drugs, oral contraceptives, and immunisation. Other differential diagnoses include conception and other immune-modulating diseases such as inflammatory bowel disease, lupus, and Behcet disease.5 Furthermore, there are no definitive tests available for diagnoses of this syndrome.1 Blood tests assess immune system activity and, most importantly, inflammatory markers such as ACE, alkaline phosphatase, and CRP.5 Chest radiography is often the first imaging modality performed. Typical findings include enlarged hilar lymph nodes with or without calcification and interstitial lung changes. Imaging modalities are necessary to rule out other pathologies. Although most cases resolve spontaneously, patients presenting with symptoms are initially managed with non-steroidal anti-inflammatory drugs. In contrast, individuals with persistent or refractory manifestations may need treatment with glucocorticoids or other immunomodulatory agents.1,2 Histological diagnosis may be required in case of deviation from the classical course or failure to achieve remission within the expected timeframe.5
CONCLUSION
Löfgren syndrome is the usual presentation of acute sarcoid arthritis, occurring in approximately 5–10% of sarcoid cases. Sarcoidosis symptoms can differ significantly from one patient to another depending on the particular organ affected by the disease. Typical signs and symptoms include fever, bilateral symmetric hilar lymphadenopathy, multiple joint inflammation, and erythema nodosum; however, since these symptoms are not specific to sarcoidosis, and there is no definitive test for sarcoidosis, accurate diagnosis is difficult and sometimes requires advanced clinical tests. Early detection of Löfgren’s syndrome is crucial for immediate treatment and to minimise potential complications such as blindness, renal failure, and pulmonary hypertension.4







