Abstract
Retained foreign bodies have become very rare in countries where the safety rules in the operating theatre are very rigorous and follow precise guidelines. There are low-income countries where hospital structures are precarious, in which the implementation of surgical safety rules has only been effective recently. Surgical teams in these countries are not yet well trained in the observance of the guidelines concerning swab count, meaning that textilomas are not uncommon. Abdominal textiloma may be asymptomatic, or present serious gastrointestinal complications such as bowel obstruction, perforation, or fistula formation because of misdiagnosis. It may mimic abscess formation in the early stage or soft tissue masses in the chronic stage. This case report presents a 27-year-old female who underwent an emergency laparotomy in a rural surgical centre for an ectopic pregnancy. Two months later, a swelling had appeared on the left side of her abdomen, gradually increasing in size, which was not very painful but caused digestive discomfort and asthenia. Intermittent fever was described and treated with antibiotics. The patient was referred to a better equipped centre to benefit from a CT scan. A textiloma was strongly suspected on the CT but a left colic mass was not excluded. Laparotomy confirmed the diagnosis of textiloma and the postoperative course was uneventful. Prevention rules must be strengthened in these countries where patients can hardly bear the costs of iterative surgeries for complications that are avoidable.
INTRODUCTION
Despite the establishment of sponge count during the operative checklist, foreign bodies such as surgical gauze can be left behind. The exact incidence of intra-abdominal foreign bodies is not known because of under-reporting or unrecognition.1 In June 2015, 205 articles on textilomas were collected by Mercier et al.2 Depending on location within the peritoneal space, clinical symptomatology may vary from mild abdominal pain to serious complications such as bowel or visceral perforation, obstruction, fistula formation, or sepsis.3 The imaging appearance of textilomas is not widely known and they can be mistaken for a soft tissue tumour.4 In Madagascar, textiloma incidents are not uncommon. Operative checklists in operating theatres have only become systematic very recently. Given the poor working conditions and the lack of staff in the context of emergency surgery, some surgical teams do not follow the mandatory steps recommended by the guidelines from the Association of Perioperative Registered Nurses (AORN) regarding swab count.5
The authors describe a case of intra-abdominal textiloma mimicking a left colonic tumour, which appeared 2 months after an emergency laparotomy for ectopic pregnancy. The first operation was carried out in a rural surgical centre. Throughout the description of this case, a review of the literature concerning variations in the clinical and radiological presentation of textilomas is made. The authors would also like to emphasise the importance of swab counting, as per the guidelines, especially in low-income countries.
CASE REPORT
A 27-year-old female patient was referred to a visceral surgery ward in October 2018 because of abdominal swelling localised in the left quadrant of the abdomen, near the umbilicus. Two months previously, the patient had undergone an emergency laparotomy for ectopic pregnancy and became aware of a palpable abdominal mass on the left side of the abdomen, which become painful 1 month after an uneventful postoperative course. The mass increased in size and was associated with pain and intermittent fever. The patient also presented with asthenia, anorexia, and food vomiting in the late postprandial period, with moderate weight loss. There was no sign of intestinal obstruction and the patient was given oral painkillers and antibiotics each time she had a fever. No blood tests or imaging were performed to explore this postoperative mass in the hospital where the previous surgery was carried out. Because of the persistence of symptoms and a progressive deterioration of her general condition, the patient decided to seek an alternative centre for treatment. Physical examination revealed asymmetry of the abdomen with the left side being deformed by swelling. Inspection of the abdomen showed that the previous surgical approach was a transverse Pfannenstiel incision.
The earlier operation was performed at another hospital and it was difficult to obtain sufficient information about the surgical procedure from the patient.
There was a marked tenderness in the whole abdomen. The day she arrived in the centre, she no longer had a fever. White blood cells were moderately raised to 12,000 /mm3. A plain film of the abdomen showed limited opacity in the projection of the left flank, with air-fluid levels wider than the height of the projection of the hypogastrium. The abdominal ultrasound revealed a large mass at the left flank and a heterogeneous hyperechoic echostructure centred by gaseous structures with posterior shadow cones which measured up to 9 cm long, surrounded by infiltrated bowel (Figure 1). CT showed a left paracolic, well delineated, spontaneously hyperdense mass, which was not enhanced after injection of intravenous contrast. There was a fluid collection mixed with stercoral materials, with air-fluid level mimicking abscess formation inside a tumoural colonic mass adjacent to the left anterior abdominal wall (Figure 2). The descending and sigmoid colon were infiltrated with parietal thickening, associated with a low abundance of intraperitoneal liquid effusion. Gossypiboma was considered because of the recent surgical history, but a locally advanced colonic left tumour was not excluded because of the stercoral materials inside the mass. At laparotomy, a fluid containing mass adherent to the abdominal wall, strongly encrusted inside the sigmoid colon, was excised. After evacuation of approximately 400 mL of purulent fluid, a surgical sponge was successfully extracted (Figure 3), leaving a perforated colon on the anterior side. Abundant washing was performed. Because of the sepsis of the operative site, immediate end-to-end anastomosis of the colon was contraindicated. A temporary colostomy was made and the postoperative course was unremarkable; the patient was discharged on the seventh postoperative day.
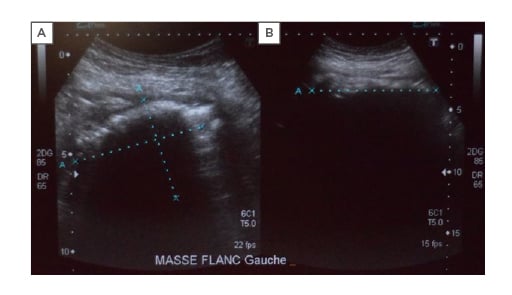
Figure 1: A) Axial and B) ultrasound sections showing an intraperitoneal, hyperechoic mass under the left hypochondrium with a posterior shadow cone.

Figure 2: CT with intravenous contrast injection axial cut. Intraperitoneal heterogeneous hyperdense formation under the left hypochondrium with mixed component that did not enhance with intravenous contrast injection.

Figure 3: Opening of the mass with evacuation of purulent fluid, allowing extraction of a gauze sponge foreign body inadvertently left at the time of a previous surgical procedure, performed with a transverse Pfannenstiel incision.
DISCUSSION
Textiloma and gossypiboma are technical terms used to describe a mass of cotton matrix that is left behind in a body cavity during an operation. The term ‘gossypiboma’ is derived from the Latin word gossypium, meaning cotton, and the Swahili word boma, meaning place of concealment.6 The first case of a gossypiboma was reported by Wilson in 1884.7 Areas of location within the body are variable. Although the most common site reported is the abdominal cavity, almost any cavity or surgical procedure may be involved. Other sites reported are the nose, tracheobronchial tree, breast, pancreas, pararenal space, vagina, femur, and spine.8,9
In 2015, Arikan and Kocakusa10 described 14 textiloma cases, whose treatment procedures had been followed-up personally by them over a period of 27 years, almost the whole of their professional lives.10 Locations of textilomas in the patients included the abdominal cavity in seven cases, inguinal surgical wound in four, epigastric surgical wound in one, thyroidectomy lodge in one, and bilateral axillary cavities in one. The case reported here is one of the most commonly seen since it is an intra-abdominal textiloma in a Malagasy woman. The last case of textiloma reported by the Malagasy authors dates from 2017.11 Cases of textiloma are not rare in Malagasy hospitals, but the cases reported are still few. In low-resource countries, poor working conditions and non-observance of universal precaution, risk factors for the occurrence of textiloma, prevail in the operating theatre. In Madagascar before 2015 swab count was not performed systematically, but according to the surgeon’s habits, however, all surgeons regardless of the socio-economic context of their place of practice should be aware of the importance of the guidelines regarding swab count in the operating room. Despite good performance of the counting protocols, incidents of retained sponges and instruments can sometimes occur.
With regard to clinical presentations and complaints, most intra-abdominal foreign bodies remain asymptomatic, and can be detected incidentally after many years. Adhesions and encapsulation are common features of gossypiboma and the lesion may present as a mass.12 Similarly, textiloma of the patient in this report was detected as a solid appearance at clinical examination and on CT 2 months after the initial surgery. Atay et al.12 described the case of a 50-year-old female patient, previously operated on because of a pelvic pleomorphic sarcoma in an outside centre 3 months before admission.12 The textiloma was initially taken as a tumour recurrence in the case described by this author. In a paper published by Arikan and Kocakusak,10 reporting on 14 textiloma cases in a period of 27 years, the mean time interval until diagnosis was 14.48 (median: 5.50) months. Some authors have reported cases discovered several years after the initial surgery. The case of a 64-year-old female with a foreign body retained in the liver 39 years after a perihepatic gauze packing described by Xu et al.13 represents the longest time for which a foreign body has been retained in the liver. Another Malagasy case concerning a 39-year-old female patient who underwent subtotal hysterectomy 7 years previously was described by Rasoaherinomenjanahary et al.11
The diagnosis of gossypiboma can be difficult because it can mimic a benign or malignant soft tissue tumour in the abdomen and pelvis.14 In this case, the patient noticed an asymmetry in her abdomen 1 month after the surgery, caused by the mass, which gradually increased in size, raising doubts between an advanced colonic tumour or a textiloma. The absence of this mass before the operation suggested an iatrogenic cause rather than a tumour. While the gossypiboma remains in the body, extrusion of the gauze can occur externally through a fistulous track or internally into the rectum, vagina, bladder, or intestinal lumen.15 Either by fistulising to a lumen or through direct migration, it can cause intestinal obstruction, malabsorption, and gastrointestinal haemorrhage.16 In this case, the postoperative foreign body became embedded in the left colic lumen, creating a fistula between the anterior side of the sigmoid colon and the capsule enveloping the textiloma. Fistulisation explains the absence of signs of intestinal obstruction in the present case. This situation, already suspected by the CT, was confirmed intraoperatively when the extraction of the textiloma left a perforation of the underlying sigmoid colon.
Many characteristic radiological findings can be used to diagnose gossypiboma. Radiographs are the most commonly used method to detect retained sponges.17 If the sponge contains a radiopaque marker, the diagnosis can be made easily using conventional radiography.17-19 Radiolucent material such as sponges can cause diagnostic problems. For this patient a plain film of the abdomen was performed, but it was not contributive because the retained foreign body was not radiopaque and the diagnosis was uncertain. This diagnostic doubt led to an abdominal ultrasound and a CT scan. Ultrasound is useful in the diagnosis of abdominal retained gauze. Ultrasound features are usually a well delineated mass containing a wavy internal echo with a hypoechoic ring and strong posterior acoustic shadowing.20 These ultrasound signs were found in the case described here. CT is the technique of choice for detecting gossypibomas and possible complications. Many authors consider a gossypiboma to be specifically indicated by a CT finding of a low-density heterogeneous mass with an external high-density wall that is further highlighted on contrast-enhanced imaging and that has a spongiform pattern containing air bubbles.17-19,21 In this case, the CT confirmed the diagnosis by showing a very limited mass with mixed content, very characteristic of a postoperative
foreign body.
Yuh-Feng et al.22 reported the 18F-fluorodeoxyglucose PET with CT (18F-FDG PET/CT) findings of an intra-abdominal gossypiboma in a 42-year-old woman who had undergone caesarean section twice previously. To date, only a few reports of the MRI appearance of gossypiboma in the abdomen and pelvis have been published. In the case reported by Atay et al.12 about textiloma mimicking tumour recurrence, CT was completed by MRI because of the difficulties with the diagnosis. The patient in this case report could not benefit from these two imaging exams due to their unavailability in the hospital centre; however, CT was sufficient to make the diagnosis of textiloma. This is in agreement with the data already published by several authors on the contribution of CT in the diagnosis of retained foreign bodies.17-19,21
Exploratory laparotomies, emergency, and complex surgeries performed in unstable patients, with unplanned changes in the surgical procedure, needing haemostatic textiles and, often, performed by tired medical teams in improper environments, are the main risk factors for retained foreign bodies during surgery. In the study by Cima et al.,23 the majority of retained bodies occurred in routine and elective open surgeries. The patient in this case report underwent an emergency surgery for acute abdominal pain due to an ectopic pregnancy and transversal Pfannenstiel incision was performed. The site of the textiloma suggests that it was used to achieve haemostasis and to push back the intra-abdominal viscera in order to facilitate the exposition. Brazilian authors have also experienced the same situation, reporting that during emergency surgeries, sponges are routinely inserted into cavities to expose the operative field. The transverse incision during the previous surgical procedure in the case of this patient, may have contributed to the occurrence of this incident. The surgical sponge had probably been placed deep in the abdomen, far from the surgeon’s field of vision, and mixed with blood at the end of the procedure. According to the guidelines from AORN regarding swab count,5 sponges should be counted during all procedures in which the possibility exists that a sponge could be retained in the patient. Sponge counts should be performed before the procedure to establish a baseline, before closure of a cavity within a cavity, before wound closure begins, at skin closure or end of the procedure, and at the time of permanent relief of either the scrub person or the circulating nurse.
Patient safety rules in the operating room have been in effect for decades in high-income countries whereas in low-resource countries, as is the case here, the application of these rules is recent. Most of the surgical centres far from the city have not yet received adequate training on recommended practice for sponge, sharps, and instrument counts. Therefore, some teams still have trouble achieving the required safety standards. However, even in teams already trained, retained foreign bodies can occur despite rigorous precautions. Greenberg et al.24 reported the frequency and significance of discrepancies in the surgical count; in a prospective study, they evaluated the rate and type of discrepancies encountered. The authors concluded that one in eight surgical cases involves an intraoperative discrepancy in the count. The majority of these discrepancies detected unaccounted-for sponges and instruments, which represents potential retained sponges and instruments.24
One author reported that small aesthetic incisions can contribute to retained foreign bodies during a surgical procedure.25 In the case described here, the surgeon who performed the first operation opted for a transverse incision for aesthetic purposes. However, procuring aesthetics was a source of exposure problems during the operation. Added to this was the unavailability of radiopaque sponges in these distant surgical centres, as well as the below-standard working conditions usually experienced in operating theatres in low-resource countries. A gossypiboma should be removed using an appropriate intervention such as open or laparoscopic surgery as well as by endoscopy, in which intraluminal cases are detected, in accordance with different parameters of the textiloma such as its duration in the body, localisation, and the clinical condition it had developed. Rarely, a spontaneous discharge of the foreign body by the rectal route has also been reported.26 When an intracorporeal mass is observed, surgeons should elaborately investigate the patient’s past surgical history by considering the possibility of a textiloma because they are able to mimic any malignant condition.10
Reintervention through open surgery is the best therapeutic choice to remove gossypiboma as soon as the diagnosis is suspected, and this is what the authors of this case did. Indeed, these postoperative foreign bodies are often extracted under septic conditions making an open laparotomy more justified than a laparoscopic approach to the extraction.
Gossypibomas are in fact preventable burdens which create very severe problems for both patients and surgeons, making their prevention far more important than their cure. Careful counting of the gauzes and surgical towels both before and after any major or even minor surgical interventions, re-exploration of the surgical site in cases of any conflict of counting, usage of the routine postoperative plain X-ray imaging to detect any incidental case if gauzes are labelled preoperatively, and usage of gauzes and towels with long tails which stay extracorporeally during the operation are preventive measures to minimise the problem, although human-based errors cannot be totally abolished.10 In some institutions, radiofrequency scanning for electronically tagged surgical sponges has been introduced for all operative cases as an addition to standard counting procedures to check for retained sponges.25 However, in a low-resource country, as it is the case here, such costly paraclinical investigations are not yet available and primary prevention remains the rule. In this case, the patient had to accept all costs related to the two operations. Added to this is the cost of travelling to receive treatment in a better-equipped centre in the capital, and the cost of the CT. Subjecting a patient to a second operation because of an iatrogenic, yet avoidable, complication is unacceptable. Such complications should no longer occur in the present day.
CONCLUSION
Textilomas occur mostly in routine procedures, mainly in laparotomies and at the beginning of the professional career, highlighting, particularly in low-income countries, the need for primary prevention. Given the resource-limited conditions of many African hospitals, it is essential to minimise preventable surgical complications such as textilomas through high-quality training about safety rules during surgery. Challenging medical situations, omission of security protocols, and inadequate work conditions contribute to postoperative retention of foreign bodies. The context of developing countries does not excuse a lack of rigor and meticulousness in respecting safety rules in the operating theatre.







