BACKGROUND AND AIMS
Hepatitis C virus (HCV) infection has been associated with extrahepatic malignancies such as colorectal carcinoma (CRC).1 The majority of CRCs arise from adenomatous polyps, and it is not known if HCV infection influences the growth of these pre-cancerous lesions.2 This study evaluates the prevalence of colorectal adenomas in patients with HCV compared to the general population, and whether HCV is an independent risk factor for the detection of colorectal adenomas.
MATERIALS AND METHODS
This case-control study included patients who underwent screening colonoscopy at the authors’ hospital. Patients were divided into cases (HCV) and controls (non-HCV). Patients with hepatitis B, inflammatory bowel disease, or no biopsy reports were excluded. Colonoscopy findings were stratified on the biopsy results i.e., hyperplastic, adenomatous, CRC, or normal mucosa. Continuous variables were analysed using the Mann–Whitney U test, and categorical variables using the Chi-square and Fisher’s exact test with p<0.05 were considered statistically significant. After a 1:1 propensity score matching for chronic hepatitis C, a matched cohort of cases and controls was generated. A multivariate regression analysis to compute an odds ratio (OR) for colorectal adenoma detection rate was done.
RESULTS
415 patients were screened, of which 109 patients with HCV and 97 controls were included. Descriptive analysis showed that age (p=0.030), BMI (p=0.001), aspirin use (p=0.001), smoking (p=0.004), alcohol use (p=0.010), and adenoma detection (p=0.006) were significantly different between both groups. There were 118 polyps in the HCV group and 78 polyps in the control group, and 97% of the polyps in the HCV group were tubular adenomas. Polyps in the HCV group were arising from the ascending colon in 24.5%, 25% from the sigmoid colon, and 20% from the transverse colon. After propensity matching for HCV, 97 cases and 97 controls were generated. Following covariate adjustment, logistic regression analysis showed that patients with HCV had an OR of 2.06 (p=0.030), and aspirin users had an OR of 0.38 (p=0.010) in having colorectal adenoma (Figure 1).
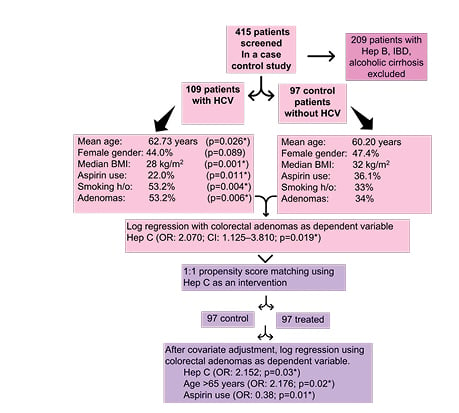
Figure 1: Flowchart of the study.
*Stastistically significant p-value. CI: confidence interval; HCV: hepatitis C virus; Hep C: hepatisis C; Hep B: hepatitis B; h/o: history; IBD: irritable bowel disease; OR: odds ratio.
CONCLUSION
The authors’ study shows a significantly higher rate of adenomas in patients with chronic HCV. On multivariate analysis with and without propensity score matching, HCV infection was found to be an independent risk factor for colorectal adenoma. Current guidelines do not recommend earlier screening for CRC for such patients. Prospective studies would be required to assess if treatment of HCV leads to lower adenoma detection rates








