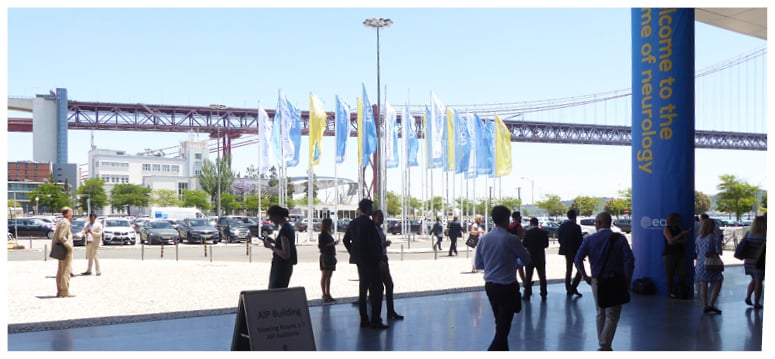
The 4th European Academy of Neurology (EAN) congress was held in the hilly, coastal capital of Lisbon, Portugal, on the 16th–19th June 2018. The over-arching theme of the congress was neurogenetics, with the meeting aiming to unravel these seemingly hidden diseases. Situated just a stone’s throw away from the congress hall, the impressive 25 de Abril suspension bridge over the Tagus river symbolised the collaboration seen at this year’s EAN congress, with attendees travelling from across the globe to revel in this magnificent event.
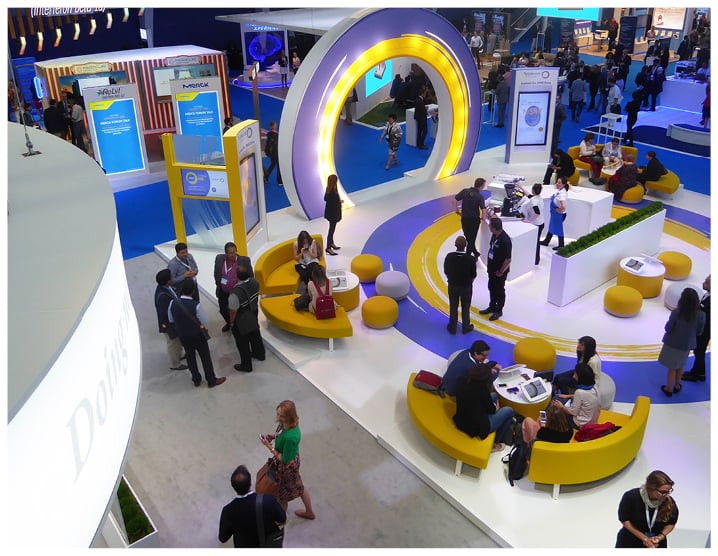
The programme for the 4th EAN congress was full of focussed workshops, hands-on courses, and spectacular symposiums presenting the cutting-edge research from a myriad of neurological topics. Some of the ground-breaking highlights from the congress are detailed in this Congress Review, including new treatment guidelines, an investigation into consciousness after stroke, and many more intriguing results.
Prof Joaquim Ferreira, Chair of the local organising committee, welcomed attendees to the Opening Ceremony and encouraged everybody to learn from the numerous sessions, share experiences and knowledge, meet new people, and explore the Portuguese capital. Prof Günther Deuschl then took to the stage for his last presentation as EAN President and gave a thought-provoking reflection on some of the major advances in neurology. Innovations in neurology were the cornerstone of Prof Deuschl’s presentation, including the approval of the first drug to treat secondary multiple sclerosis, which is highlighted later in this Congress Review. The 2018 Brain Prize winners were also celebrated by the EAN President for their outstanding work in the field of Alzheimer’s disease pathology and their identification of blood biomarkers and imaging techniques, allowing early diagnosis of this debilitating disease.
Prof Deuschl proceeded to highlight the importance of identifying and actioning new diagnosis and treatment programmes and their direct impact on the burden of neurological disease in Europe. Neurological diseases have been ranked the third highest cause of disability adjusted life years and death in Europe following a continent-wide assessment of major diseases. Prof Deuschl used Alzheimer’s disease and stroke, despite increased prevalence of the conditions, as examples of how disability adjusted life years have drastically reduced, highlighting the impact of treatment progress and early diagnosis on this ever-progressing field.
Prof Deuschl concluded his last presidential presentation by stressing the important role neurologists play in ageing European societies, with just under 6,000 neurological diagnoses per neurologist. He called for a collaborative approach between all neurologists to work together to achieve common goals. As a final act, Prof Deuschl presented Prof Alistair Compaston (UK) and Prof Mark Hallett (National Institute of Neurological Disorders and Stroke [NINDS]) with honorary membership for their contribution to multiple sclerosis and human motor control disorders research, respectively.
With EAN 2018 fresh in our minds, the EMJ team is already looking forward to the 5th EAN congress, to be held in one of Europe’s fastest growing cities: Oslo, Norway, from the 29th June–2nd July 2019. The EAN congress 2018 will be the first ever congress not to be presided over by Prof Deuschl and will mark the first congress under the presidency of Prof Franz Fazekas. We look forward to witnessing the new era Prof Fazekas will bring to the EAN congresses, as we finish celebrating Prof Deuschl’s esteemed contributions to the event.

Cost Burden Analysis of Brain Disorder Treatment
BRAIN disorders currently affect approximately one-third of European citizens. With up to 8 out of 10 patients with a brain disorder either remaining untreated or inadequately treated despite the existence of effective therapies; these statistics represent a significant number of patients. In response to this, the European Brain Council (EBC) initiated the Value of Treatment (VoT) study to examine the treatment gap and deliver recommendations. This study was one of the topics of discussion at the EAN congress, as reported on in an EAN press release, dated 18th June 2018.
The Vice President of the EBC, Prof Wolfgang Oertel, explained: “The VoT puts a valuable resource in the hands of political decision-makers that contains the background information they need to reach conclusions on and analyse the return on investment for various treatments, as well as pinpointing cost-effective policy recommendations for treating brain disorders in their countries.”
The VoT involved an assessment of the health, social, and economic costs of the best possible treatment compared to standard treatment or non-treatment. It contains nine case studies assessing costs and providing recommendations for care, including Alzheimer’s disease, epilepsy, headache, Parkinson’s disease, restless leg syndrome, multiple sclerosis, normal pressure hydrocephalus, schizophrenia, and stroke.
One of the cornerstone recommendations of the study was that optimal care and an early start to treatment was the most cost-effective long-term policy. An example provided to highlight this was that of a stroke patient who had felt abandoned after acute therapy. After the treatment had taken place, there were no further steps in place, such as a course of rehabilitation or discussing the patient’s work situation. Prof Oertel noted that while it would have been a significant time investment to provide the patient with maximum support to get back on their feet, it would still have been worthwhile. He commented: “That said, in overall economic terms, it is still more cost-effective than early retirement and permanent incapacity at the age of 45.” It is hoped that the VoT study’s recommendations will provide inspiration for ensuring an improved standard of care for patients with brain conditions.
Thrombectomy in Elderly Acute Stroke Patients: A Risky but Promising Therapy
A LIFE free from stroke-related disability may be available for a select group of older patients in the future using mechanical thrombectomy, suggests research presented in a EAN press release dated 18th June 2018. In numerous studies, endovascular thrombectomy has been shown to be more beneficial than drug-based therapy alone, but it is not without considerable risks; as a result, identifying those patients for whom this procedure is appropriate is of utmost importance.
“More and more study results show the effectiveness of mechanical removal of blood clots after a stroke. But researchers are still trying to determine the type of patient for whom this relatively new procedure is the best treatment option,” explained Dr Ary Lopes de Sousa, Centro Hospitalar de Lisboa Central, Lisbon, Portugal.
Following this, Dr de Sousa and colleagues reviewed >200 patients who had experienced an anterior acute ischaemic stroke and had either no or slight disability prior to the event. The patients were categorised into two groups, the former containing patients <80 years old and the latter containing those ≥80 years old. These patients had all received thrombectomy and the treatment did not differ between groups (e.g., the time to revascularisation).
Findings showed that hypertension and transitory ischaemic attacks were both more frequent in the older group, but no differences in death rates were recorded between the groups. Additionally, a poor functional outcome was exhibited 3 months post-treatment in two-thirds of the older group (i.e., moderate-to-severe limitation at performing daily tasks), compared to 46% in the younger group. However, in contrast to these poor outcomes, one third of the older group was shown to have mild or no impairment to their everyday lives at 3 months follow-up. Thus, while thrombectomy is clearly a risky treatment in some regards, it can also be highly beneficial. The challenge now is to identify those in the very elderly patient population for whom mechanical thrombectomy may be a beneficial treatment option, and for this, more research is needed. “For patients over 80, thrombectomy appears to be riskier than for younger patients. But one third of the patients over 80 can be fully functional in their everyday lives after the procedure, so we must identify the factors associated with this favourable outcome,” concluded Dr de Sousa.
A Focus on Stroke Treatment and Prevention
THE LATEST developments in stroke treatment were a hot topic at this year’s EAN congress, including reducing the risk of recurrent stroke and the use of thrombolysis in acute stroke treatment. Detailed in a EAN press release dated 17th June 2018, these latest results will make a significant contribution to improving stroke management.
Although stroke-related death rates have steadily declined in recent years due to improved treatment and rehabilitation, further progress is still required to prevent the 600,000 newly reported cases in Europe each year. In addition, one study has highlighted the high risk of recurrent stroke; therefore, researchers have recently been addressing these issues in a number of studies presented at the EAN 2018 congress. For example, one study demonstrated the suitability of combined clopidogrel and aspirin treatment as a preventative measure of stroke recurrence. Around 4,900 post-minor cerebral infarction or transitory ischaemic attack patients were given either placebo, aspirin only, or the combined regimen. Although a heightened risk of major haemorrhage was associated with the clopidogrel-aspirin patients, this group experienced fewer cerebral infarctions, heart attacks, and deaths following the monitoring period.
Furthermore, the results of an investigation into embolic strokes of unknown cause showed that oral rivaroxaban, an inhibitor of factor Xa, was not more effective than aspirin, with the number of ischaemic events in both treatment groups being very similar (158 and 156 for rivaroxaban and aspirin, respectively). The study also showed an increased risk of haemorrhage with rivaroxaban therapy. “Before initiating any anticoagulation therapy, we still need to determine if there really exists a cardioembolic source,” commented Prof Franz Fazekas, Medical University of Graz, Graz, Austria.
With a more positive outcome, another study presented evidence of the effective use of thrombolysis when time of stroke onset is unknown. The WAKE UP study involved patients who had evidence of ischaemic lesions on diffusion-weighted MRI only, suggesting stroke occurred ≤4.5 hours prior. A total of 53.3% of participants had favourable treatment outcomes alter intravenous alteplase compared to 41.8% with placebo. In addition, on a scale of 0 (no symptoms) to 6 (death), the thrombolysis group scored an average of 1 and the placebo group averaged 2; however, a higher incidence of intracranial bleeding and increased mortality rates were associated with alteplase treatment. “We now have clues how MRI may identify those patients in whom thrombolysis is beneficial even if we do not know the exact time of stroke onset,” stated Prof Fazekas. The results provide hope for improving the risk of permanent stroke-related injury and preventing stroke altogether.
Improving Migraine Treatment and Prevention Could Save The Global Economy Billions
MIGRAINES seriously burden patients’ work and social lives, but also impact on the wider economy. Results from a French and a second Swiss study, presented in a EAN press release dated 17th June 2018, highlight the pressing need to increase investment in research into the prevention of migraine, which is believed will benefit society as a whole. A French study of 7,700 migraine patients and a Swiss study of 700 working migraine patients both set out to assess the true cost of migraine, from individual patient costs to society and business costs as a whole.
Of those included in the French study, 3.8% had experienced severe migraines on at least 8 days each month. Of those, the average age was 41 years, meaning that migraines are affecting individuals of prime working age, who are likely to have families to support. The study results also revealed that migraine patients reported missing an average of 33 working days a year due to the condition, costing the economy roughly €3.8 billion. The study also highlighted that patients also spent >€30 per month for non-reimbursed medicines, and 14% reported that family members had to adjust their working hours as a result of the patients’ migraines.
The 700 Swiss patients reported losing an average of 32 days a year as a result of migraine, which is not dissimilar from the French study. However, there were differences depending on the type of headache the patient experienced: patients with chronic migraine, episodic migraine, and low-frequency episodic migraine missed an average of >56, 33, and 15 working days per year, respectively. Results also highlighted that the number of sick days taken were not constant, the total steadily increased along with the amount of medication taken.
Migraines impact all aspects of the patient’s life and as a result, the quality of life for migraine patients remains far from satisfactory. As a consequence of these eye-opening study results and the burden migraines place on individuals, experts at the EAN Congress 2018 issued a call for increased investment in migraine research and prevention which would benefit not only those who experience migraines, but also society as a whole.
New Developments in Dementia Research
DEMENTIA: a disease that 47 million people across the globe currently present with, which already results in a notable social and economic burden. This number is currently predicted to increase to 131 million by 2050, with the social and economic burden set to increase accordingly.1 Therefore, dementia research was a key talking point at the EAN congress, as reported in a EAN press release, dated 17th June 2018. Two of the topics highlighted were the use of big data and an ongoing study into the impact of physical activity.
While previous observational studies have suggested that individuals who regularly partake in physical activity tend to have a better cognitive status, there is the need to more closely examine this potential association. As Prof Ana Isabel Verdelho, EAN Scientific Panel on Dementia and Cognitive Disorders, explained at the EAN congress: “If individuals who have been physically active throughout their life do not develop dementia, you cannot necessarily conclude that physical activity is the reason. These persons may have taken other good decisions as well, for example, a healthy diet or regular checks for vascular risk factors.”
Therefore, a study has been designed to determine if physical activity is specifically associated with superior cognitive outcomes. Participants have been identified who all share common signs of a vascular disease in the brain. These participants have been randomised into two groups: one group undertakes supervised physical activity and the other group does not. The results of this study are eagerly anticipated.
One of the reasons more of these studies have not been conducted is that it is very challenging to identify patients for randomised studies because symptoms of the disease are not perceived until they cause noticeable impairment. This is where researchers are hoping big data will play a role. Using data such as molecular biomarkers and electronic health records, it might be possible for researchers to obtain a better understanding of the development of dementia and its course. Prof Verdelho added: “Moreover, resource distribution could be optimised and tailored treatments could be made available to patients exhibiting special courses of the disease.” She also added a note of caution: “Precision and critical analysis will be the keys for making optimum use of this data. Although we assume that big data is one of the correct paths to new findings, this approach has not yet arrived at a point where it affects actual practices of prevention or treatment.”
References
- Alzheimer’s Disease International. Dementia statistics. Available at: https://www.alz.co.uk/research/statistics. Last accessed: 02 July 2018.
Sleep Disorders: A Diagnostic Aid?
ARE your patients presenting with sleep disorders? If so, the work of Dr Konstanze Philipp, Universitätsklinikum Münster, Münster, Germany, presented at EAN, and reported in an EAN press release dated 16th June 2018, is of paramount importance. Sleep disorders are often harbingers of serious neurological disorders. Sleep disorders to pay attention to include insomnia, excessive sleepiness, or abnormal sleep behaviours such as active sleep.
Dr Philipp explained: “Two-thirds of the population suffering from REM sleep disorders later develop Parkinson’s disease, Lewy body dementia, or multiple system atrophy.” He noted that a patient’s history of sleep disorders, when used in combination with certain biological markers, could enable the diagnosis of neurodegenerative diseases many years before the first consciously perceived symptoms arose. Diagnosing such conditions as early as possible is currently believed to be a key step in improving patient outcomes. One example is Parkinson’s disease, for which it is believed that the latest therapeutic approaches, if begun early enough, could delay or perhaps prevent the development of the disease. Therefore, any insights that lead to an earlier diagnosis could have a significant impact on patients with neurological disorders. Dr Philipp used three case studies to illustrate the importance of paying attention to these early warning signs.
However, there is a significant stumbling block faced by neurologists in this regard: a patient’s sleep history is often not documented in their medical records, making an early diagnosis in this manner somewhat challenging. Dr Philipp urged: “We have to raise awareness on this matter.” She went on to note: “Asking questions, listening, and documenting are the least expensive and easiest ways of diagnosing these complex diseases. We should use them. The therapeutic approaches are still expandable. Nonetheless, early detection is essential, especially for neurodegenerative disorders.”

Sex Differences in Early Parkinson’s Disease Progression
PARKINSON’S disease pathophysiology shows sex differences in untreated patients, according to the results of a Slovenian study. Reported in a EAN press release dated 16th June 2018, this study presents the first neurophysiological evidence supporting the theory that Parkinson’s disease progression is different in men and women, suggesting sex is an important factor in treatment and management of the disease.
Previous studies have shown that women appear to be better protected from Parkinson’s disease than men, with nearly twice as many males diagnosed with the condition than females; however, there has been uncertainty as to whether sex-specific pathophysiology is responsible for this observation. Since functional changes in the primary motor cortex can be detected in early Parkinson’s disease using transcranial magnetic stimulation (TMS), the Slovenian-based research team focussed on this technique to investigate sex-specific differences in disease progression.
The Parkinson’s Disease Rating Scale (UPDRS) was used to assess disease-related impairments in 39 untreated, newly diagnosed patients with Parkinson’s disease (16 females and 23 males). TMS was then performed on the patients and a control group to investigate parameters such as motor thresholds of the brain, input and output curve, and short interval intracortical inhibition. Paired associative stimulation was also used to measure brain plasticity.
Although the UPDRS test did not show any sex-specific differences in motor scores, the input and output curves were less steep for females on the side of the brain most affected by Parkinson’s disease. Furthermore, the female patients displayed more preserved short interval intracortical inhibition in both brain hemispheres compared to the male patients, and responded better to the paired associative stimulation protocol. No sex-related differences for any parameter was found following TMS in the control group. “The detected gender differences in corticospinal and intracortical excitability in patients with early untreated Parkinson’s disease represent differences in disease pathophysiology,” summarised Dr Maja Kojovic, Ljubljana University Medical Centre, Ljubljana, Slovenia. With reference to the significance of these sex-specific findings in enhancing early Parkinson’s disease patient care, Dr Kojovic added: “Gender may also prove to be a relevant factor when choosing appropriate treatment.”
Multiple Sclerosis Patients and Caregivers Contribute to New European Academy of Neurology Guidelines
PALLIATIVE care guidelines for people with multiple sclerosis (MS) have been developed in collaboration with those they most directly affect: MS patients themselves and their caregivers. As reported in a press release from the EAN congress dated 17th June 2018, 934 individuals directly related to the condition contributed to the creation of these new guidelines.
To allow those most affected by the disease to contribute, two methods of gathering data were used: an international online survey, supported by national MS societies; and targeted focus group meetings. The data gathered showed that most patients agree with the topics suggested by the EAN experts, with around 98% approving of the incorporation of multidisciplinary rehabilitation into the guideline. In the online survey, 569 free comments were recorded, with 182 (32%) relating to specific topics. Furthermore, 227 comments (40%) pertained to additional topics, 16 of which were suitable for inclusion within the guideline. Data gathered from five focus groups (three with MS patients and two with caregivers; a total of 35 people) supported the findings of the online survey. Thus, this collaboration between patient, physician, and caregiver helped to raise a number of important topics that may otherwise have been missing from the guideline.
“It was resource and time intensive to include consumers in the guideline process, but also highly rewarding. Patients and caregivers really helped us to formulate the guideline in a way that was in line with actual practice and their own needs,” explained Prof Sascha Köpke, Institute of Social Medicine and Epidemiology, University of Lübeck, Lübeck, Germany.
This development marks a huge success for shared decision-making and is a promising step towards patient-centric, personalised medicine, an approach that the EAN has long supported. “The involvement of patients and caregivers increases the reliability and relevance of the guideline for clinical practice,” concluded Prof Köpke. Just as personalised medicine is taking root in disciplines throughout the medical profession, so too is it hoped that this collaborative form of guideline development will become more widespread.

Multiple Sclerosis: New Drugs and European Treatment Guidelines
TWO novel multiple sclerosis (MS) drugs have recently been approved for use in the prevention of disease progression, coinciding with the publication of new MS treatment guidelines. A EAN press release, dated the 16th June 2018, presented the first drug approved for the treatment of primary chronic progressive MS, along with the timely release of treatment guidelines conceptualised by 13 European countries in combination with the EAN and the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
The focus of MS treatment is to avoid relapse and halt the progression of this debilitating chronic inflammatory disease. By suppressing the chronic inflammation, appropriate and effective treatment has been able to attain disease control in 80–85% of patients. Two new MS approved drugs are hoped to further control disease for MS patients: cladribine, originally an anticancer drug, offering a convenient treatment option, and ocrelizumab, a monoclonal antibody targeting B cells involved in the inflammation.
The most common neurological disease in young adults, MS affects 2.3 million people worldwide, and as such, continuing to strive to prevent disease progression and its severe impact on quality of life is vital; these drug approvals could not have come soon enough.
In accordance with these drug approvals, new MS treatment guidelines building on analysis from clinical studies presented 21 recommendations to support physicians’ decision making. Commissioning these guidelines is part of the EAN guideline programme in which all important neurological diseases will be reassessed, with roughly 20 guidelines currently being drawn up. Prof Günther Deuschl, EAN President, commented on the new guidelines and the EAN influential stand point: “These efforts underscore the major significance of the EAN, which is working through overarching topics of this kind and thus providing important principles not only to medical practitioners but also for healthcare policy.”
Prof Deuschl summarised the importance of both guideline releases and new drug approvals for the treatment of MS, and stated: “Promising new drugs and the treatment guideline published this year by the ECTRIMS and the EAN will further refine and improve the treatment of MS in substantial ways.”
Improving Assessment of Consciousness Disorders
SEVERE brain injury diagnoses, which require evaluation of consciousness at various timepoints, could be improved using novel assessment and examination methods presented by Prof Steven Laureys, Coma Science Group, University of Liège, Liège, Belgium, at the EAN Congress 2018. Reported in a EAN press release dated 18th June 2018, these advances provide hope for the one in three Europeans affected by brain injury or disease during their lifetimes, as well as enhancing progress in this under-researched, relatively small field of neurology.
Although the number of individuals who survive comas following brain injuries is increasing, disorders of consciousness still present a great challenge for neurologists, whose decisions have a large impact on patient survival. To build on the current gold standard neurobehavioural tool, the Coma Recovery Scale (CRS)-Revised, which is not applicable to all patients, the SECONDs scale was developed and tested in severe brain injury patients. This tool was found to determine the conscious state of a patient to 99% accuracy by applying the five most frequently observed criteria and will be particularly useful in time-limited cases. Recent research has also revealed the importance of fluctuations in consciousness; for example, a study examined severe brain injury patients four times a day using CRS scores and showed that consciousness state varied throughout the day. “This finding supports the recommendation to test patients multiple times within a short time period to establish a reliable diagnosis,” commented Prof Laureys.
Technological advances have also been reported in the field of consciousness disorders, such as the refinement of high-tech imaging during diagnosis. Diffusion tensor imaging, which uses MRI to record motion and directional dependence of water diffusion in the body, can aid clinicians to eliminate uncertainties during diagnosis. Novel therapeutic options are also being investigated in clinical studies, such as noninvasive transcranial direct current stimulation. It has been shown that 20 minutes of this treatment applied to the prefrontal cortex transiently improved state of consciousness after brain injury, and treatment repetition prolonged this behavioural change for up to 1 week after the end of therapy.
During his presentation, Prof Laureys stressed the importance of not providing false hope to patients and their families due to these new treatment advances, and explained how future challenges will involve implementing these high-tech methods and scientific findings in clinical practice across Europe. However, since research on brain damage and coma is relatively limited compared to other major neurological diseases, these long-awaited advances are welcomed by clinicians and their patients.
Immigration and New Insights for Neurologists
IMMIGRANT populations have been found to offer neurologists a wealth of information regarding possible risk factors for neurological diseases. According to international studies presented at EAN and reported in a EAN press release dated 16th June 2018, both stroke and multiple sclerosis (MS) have been strongly linked to environmental factor risks, as opposed to genetic predisposition, when analysing the health status of immigrant populations.
A Canadian study compared 1 million new arrivals to the country with roughly 3 million immigrants who had lived in Canada for ≥5 years. Despite lower income and limited access to healthcare systems, first-generation immigrants were found to have a much lower risk of stroke than those who had been in Canada for ≥5 years. Prof Antonio Federico, University of Siena, Siena, Italy, and one of EMJ Neurology’s esteemed Editorial Board members, explained: “The study authors concluded that the risk of suffering a stroke was less a question of genetics, but more down to environmental factors, such as diet.”
A separate study assessed MS prevalence in immigrant populations in Norway. MS was found to be most widespread among immigrants from Europe and North America, whereas those affected by MS from Africa and Asia were limited, showing an uneven worldwide MS prevalence. A sharp increase in MS cases in second-generation immigrants from Pakistan was identified. “This lends additional weight to the theory that strong environmental factors raise the risk of MS,” commented Prof Federico.
Despite immigrant-based studies providing an untapped source of nature versus nurture data, there are a few issues host nation neurologists and physicians should be aware of. One of these is the prevalence of rare diseases in the host country that may be of greater prevalence in the immigrant population, such as Bahçet’s disease (extremely rare in Europe, but relatively common in Asian countries). Other obstacles may include difficulty accessing medical records, language barriers and thus longer hospital stays waiting for translators, and stigma surrounding brain disorders in different cultures.
Despite the potential issues, these population studies will no doubt offer unique data and should be utilised by researchers. Prof Federico concluded that: “We definitely have to make sure that our healthcare systems provide sufficient medical care for all people, no matter whether they are from the original population or have only just arrived.”

Influence of Deep Brain Stimulation on Parkinson’s Disease Over the Long-Term
HAS deep brain stimulation changed the natural history of Parkinson’s disease? This was the question posed by the authors of a comparative long-term observational study that was presented at the EAN congress and reported in an EAN press release, dated 19th June 2018.
Deep brain stimulation is a therapeutic option that involves the positioning of electrodes in specific areas of the brain. These electrodes are connected to a stimulator that has been subcutaneously implanted into either the thorax or abdomen. This allows the generation and delivery of electrical impulses that affect the function of the areas of the brain the electrodes innervate. While numerous randomised controlled trials have demonstrated the positive impact of subthalamic deep brain stimulation in regard to motor functioning in patients with Parkinson’s disease, there are many other elements of the condition that the impact of deep brain stimulation has not been evaluated.
Consequently, this study was designed to investigate the impact of deep brain electrical stimulation on further long-term complications that are typically associated with Parkinson’s disease. Over 50 patients with Parkinson’s disease who had not been treated with deep brain stimulation were compared with over 50 patients with Parkinson’s disease who had been treated with deep brain stimulation.
While deep brain stimulation was not shown to have an effect on the long-term development of dementia throughout the progression of Parkinson’s disease, longevity, or when an individual had to be placed in a nursing home, it did show a positive effect on several other long-term complications. As one of the study authors, Dr Philipp Mahlknecht, Innsbruck Medical University, Innsbruck, Austria, commented: “Deep brain stimulation was associated with a decreased risk for recurrent falls in our cohort of Parkinson’s disease patients under long-term subthalamic stimulation when compared with patients under conservative treatments. The onset of psychotic symptoms was also found to be delayed through this treatment.” In the future, further studies need to be conducted to examine these results further.









