Abstract
Headaches are common in children and adolescents, and are the most common pain complaint when seeking medical advice. Primary headaches are one of the most common disorders of childhood, with migraine and tension type headache being the most prominent. Treatment strategies for primary headaches vary according to patient’s age, family structure, culture and beliefs, headache diagnosis, and according to the disability the headache imposes on the patient’s daily living. A multidisciplinary treatment approach was found to be an effective strategy for children and adolescents; it was shown to improve multiple outcome variants, including frequency and severity of headache, and school days missed because of headache.
INTRODUCTION
Headaches are common in children and adolescents, and are the most common pain complaint when seeking medical advice.1 Primary headaches are one of the most common disorders of childhood, with migraine and tension type headache (TTH) being the most frequent.1 In spite of their prevalence, there is a paucity of knowledge regarding the underlying pathophysiological mechanisms that cause headaches, the unique aspects of paediatric and adolescent headaches, and their evolution into headache disorders in adults. Most of our current knowledge is derived from extrapolations from studies that were conducted with adult patients. Children and adolescents are very different to adults regarding their rapid growth, significant development, and the psychological changes that happen during this time of life. Thus, findings from studies conducted on adults need to be validated for the paediatric age group. This article will discuss primary headaches that do not require any laboratory or imaging evaluation. In some instances, though, when the treating physician suspects a non-primary origin of headache, further investigation may be warranted.2 If any of the following features are present, one may consider evaluation: new onset of headache, changes in a stable headache pattern, headache that changes with posture, first onset of headache prior to 3 years of age, and headache awakening the patient at night. In case of any abnormal neurological symptoms or signs, trauma, or a history of malignancy, further investigation is recommended.2 This article will review the current knowledge about primary headaches in children and adolescents, their pathophysiology, diagnosis, and different modalities for treatment.
TREATMENT PRINCIPLES FOR PRIMARY HEADACHE SYNDROMES
Treatment strategies for primary headaches vary according to patient’s age, family structure, culture and beliefs, headache diagnosis, and according to the disability the headache imposes on the patient’s daily life.3 A multidisciplinary treatment approach was found to be an effective strategy for children and adolescents, improving multiple outcome variants, including frequency and severity of headache, and school days missed because of headache.3
Counselling and Education
Due to the variety of bio-psychosocial components in the evolution of primary headache, education of the family and patient regarding the diagnosis, its natural course, and the different possible treatment modalities, is of great importance. Educating patients about how different triggers, such as stress, sleep, diet, obesity,4,5 and environmental factors influence a headache attack, and how managing triggers can reduce the number of headache attacks, increases the patients’ internal locus of control. Therefore, the patient has a greater sense that the headache episode could be under their control.6 Reassurance about no underlying imminent disease may also be of value in case the patient and the family show great concerns about it.
Pharmacological Treatment
When recommending pharmacological treatment, one must take into consideration the age and sex of the patient, headache diagnosis, comorbidities, and side effects of the pharmacological agent.3
TREATMENT FOR AN ACUTE PAIN EPISODE
An acute episode of migraine deserves a slightly different treatment approach than an acute episode of TTH. In the case of acute migraine, the aim of treatment is to alleviate pain so that the patient will be able to function normally within 1–2 hours without the risk of relapse.7 The pain caused by an acute episode of migraine is relatively easy to control, as long as it is treated early in the course of the attack, even by over-the-counter medication, such as ibuprofen and paracetamol, that were shown to be effective for that purpose in children.8 In a more severe episode, the use of triptans is fairly common and was shown to be safe in the paediatric age group.9 However, only almotriptan (6.25 mg, 12.5 mg) has been approved for use in children by the US Food and Drug Administration (FDA) (Table 1).10
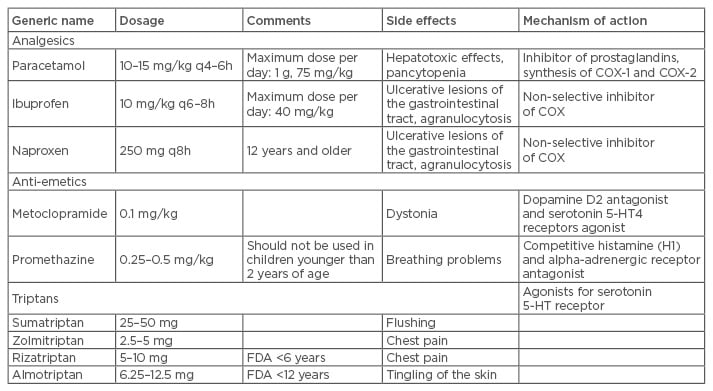
Table 1: Drug therapy for acute headache episode: dosage, side effects, and mechanism of action.
FDA: US Food and Drug Administration; COX: cyclooxygenase.
In the case of an acute episode of TTH, a more gradual strategy is appropriate, as the patient’s activity is usually not interrupted and pain intensity is usually not severe.11 In case of repeated, prolonged, or severe episodes of both types of primary headaches, the use of prophylactic treatment should be considered.
Pharmacological Prophylaxis
Lifestyle changes are recommended for young people with migraine who are struggling with the burden of their headaches, such as better sleep hygiene, regular exercise, and a balanced diet.12 For those who have demonstrated persistent disability (as assessed by either Pediatric Migraine Disability Assessment Score [PedMIDAS] or by persistent school absence) in spite of lifestyle modification, pharmaco-prophylaxis should be employed.11 The cases of repeated, prolonged, or severe episodes of both types of primary headaches, where the use of prophylactic treatment should be considered, are: frequent migraine episodes (>1–2 per week, or >3–4 per month), patients experiencing headache-related disability that interferes with daily activities, such as school attendance, and daily routines (e.g. PedMIDAS >30),13 and patients that are prone to extremely intensive, prolonged (>48 hours), hemiplegic, or basilar-type migraine, or to severe aura. Prophylaxis should also be considered if acute treatment options are either ineffective, or not tolerated, contraindicated, or regularly overused.3 For patients suffering from frequent episodic TTH and, moreover, for those suffering from chronic TTH, prophylactic treatment should also be considered.11,14
Topiramate at 100 mg a day has been shown to be effective in reducing the burden of headaches when compared to placebo.15 Other studies using amitriptyline15 and propranolol16 showed conflicting results (Table 2). Cyproheptadine has been studied as well, showing positive effects, yet its use is often limited by the troubling potential side effects of somnolence and weight gain.17 A large-scale, prospective, double-blinded, placebo-controlled study compared the effectiveness and safety of amitriptyline, topiramate, and placebo for prevention of childhood and adolescent migraine and found no significant difference.18
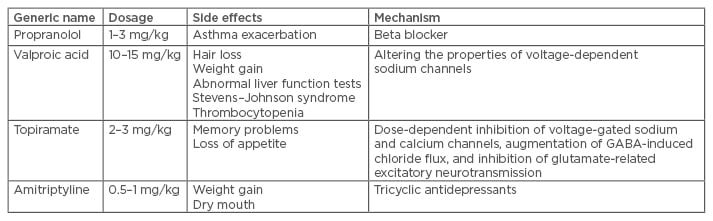
Table 2: Drug therapy for headache prophylaxis: dosage, side effects, and mechanism of action.
GABA: gamma-aminobutyric acid.
Adjunctive Pharmacological Therapy
Many of the children and adolescents diagnosed with migraine will present during an acute pain episode with nausea and vomiting, in part due to gastroparesis.17 This phenomenon might delay the absorption of the anti-pain medication and therefore usage of promotility and anti-emetic medication might be beneficial in such patients. Prochlorperazine, chlorpromazine, promethazine, and metoclopramide have all been shown to relieve nausea in acute migraine episodes, while also showing some therapeutic effect for the migraine itself.19 In addition, anxiety was found to be a common comorbidity in patients with migraine, either primary, as a pre-existing comorbidity, or secondary, due to the severe pain experienced by the patient during the acute pain episode. An anxiolytic agent was shown to be beneficial in patients who experience anxiety during an acute migraine attack. It does not address the underlying pathophysiology of migraine, but it can reduce suffering during the attack.19
Non-Pharmacological Treatments
Pharmacological, as well as non-pharmacological, treatments for primary headaches require counselling, ongoing education, and reassurance for the patient, family, and often the peer group. Non-pharmacological treatments include relaxation techniques, biofeedback training, different psychotherapeutic approaches (such as cognitive behavioural therapy [CBT]), strategies relating to daily living activities, family relationships, school, friends, and leisure time activities, or combinations of these treatments. Data supporting the effectiveness of these measures in children and adolescents are less clear-cut than in adults,3 yet a recent Cochrane review of psychological therapies for the management of chronic and recurrent pain in children and adolescents showed that different modalities of psychological interventions delivered face-to-face were effective in reducing pain intensity and disability for children and adolescents with headache, and that the therapeutic gains appeared to be maintained during follow-up.20
Relaxation Techniques
Relaxation techniques are common non- pharmacological treatments used for different symptoms in which anxiety and elevated muscle tone seem to play a role in triggering the symptom. These are relatively easy to administer, cheap, and well tolerated by patients.21 The two more commonly used techniques are progressive muscle relaxation and autogenic training. The effectiveness of both relaxation strategies has been proven in several studies and meta-analyses for pain relief in headache syndromes.22 The effect of relaxation techniques may be mediated by a direct impact on the underlying cause of headache, i.e. increased muscle tone, or it may hold an indirect effect by reducing anxiety.23 Despite many studies that were conducted on relaxation techniques, their specific underlying neurophysiologic effect on headaches remains uncertain. One of the hypotheses is that habituation to repetitive stimulation is typically reduced in patients with migraine, and relaxation increases habituation toward normal values.24 Relaxation may also reduce cortical arousal and excitability,25 which may result in reduced information processing of pain-modulating subcortical areas.26 However, these possible neurophysiological mechanisms have still to be proven. Muscle relaxation techniques require repeated training which includes contraction and relaxation of different muscle groups. There are specific instructions for practicing relaxation in the younger age group, depending on age, compliance, and motivation for change of the child and his or her family.22 It was shown that self-administered versus therapist-administered interventions had similar effects on pain reduction.21 A relatively recent small pilot study has shown beneficial effects of a combination of relaxation and biofeedback techniques in children.27
Biofeedback Techniques
Biofeedback is the process of gaining awareness of autonomic physiological functions using instruments that provide information on the activity of those same systems, e.g. brainwaves, muscle tone, skin conductance, heart rate, respiratory rate, etc. The goal of biofeedback treatment is to be able to manipulate those functions at will, either towards relaxation (to decrease anxiety, for instance) or for excitation (to improve achievements in short-term missions, such as sports). To achieve this goal, the physiologic function has to be fed back visually or acoustically to the subject so it will be perceived in a conscious manner.28 Biofeedback can be used in the context of behavioural interventions to increase autoregulatory competence; hence, the effect of successful biofeedback training may be similar to the effect of cognitive restructuring.28 According to a recent meta-analysis, evidence levels for the positive effect of biofeedback in the treatment of migraine or tension-type headache in children and adolescents are high.28 Another meta-analysis indicated that biofeedback was highly efficient in management of chronic pain in children and adolescents, and comparable with pharmacologic prophylaxis.21 It was shown to be effective in episodic as well as chronic headaches in the paediatric age group, with the concurrent use of a selective serotonin reuptake inhibitor being a positive predictive factor for a positive response. The use of prophylactic medication was associated with no favourable response to biofeedback treatment.29
Headache Diary Writing
One of the most common and well-studied behavioural strategies for the management of pain is the use of a ‘headache diary’. Recording a diary by itself was shown to reduce headache frequency in children and adolescents.30 A slightly different version of this behavioural strategy is the use of a more detailed diary, that records daily activities, patterns of sleep, workload in school, and the proportion of time spent on work versus leisure. This type of diary can be useful for the estimation of stress load and examination of the impact it holds on pain episodes.3 Recording the type and amount of analgesic taken by the patient is also of great importance, mainly in order to prevent medication overuse, which may cause augmentation of pain. The phenomenon of medication overuse headache is well documented in adults, but might occur in children as well and therefore should be addressed.31
Operant-Behavioural Treatment
The operant model focusses on pain behaviours as a major component of the pain problem, and postulates that they are subject to environmental contingencies.32 It acknowledges that suffering may be distinct from pain, yet contribute to it, and that pain may be triggered by anticipation of a threat to one’s self or identity.33 The effectiveness of operant-behavioural treatment has been studied in relation to chronic pain, and in particular three therapeutic techniques were shown to be effective: graded activity, activity pacing, and time-contingent medication management.34 In this therapeutic approach, patients learn to deal with pain instrumentally, or via operant conditioning; i.e. they learn to approach and deal with potentially pain-triggering situations instead of avoiding them.35
Cognitive-Behavioural Treatment
Over the past three decades, CBT has become a first-line psychosocial treatment for individuals with chronic pain. The goals of CBT in pain syndromes are to reduce pain and psychological stress related to it, and to improve the physical state and functioning of the patient.36 The means by which these goals are achieved are by helping the patient recognise and correct maladaptive thoughts and beliefs, reduce maladaptive behaviours, increase adaptive ones, and increase self-efficacy for pain management. CBT enables the patient to come into contact with the symptoms that accompany painful episodes/chronic pain, especially with negative emotions that may arise, like anxiety and depression.37 In all patients with recurrent or chronic pain episodes, but more so in children and adolescents, CBT aims to prevent or reduce headache episodes, and to modify the cognitive-emotional and cognitive-behavioural processes that influence pain.30 Psychological treatments (mostly CBT) delivered face-to-face were found to be effective in reducing pain intensity and disability for children and adolescents with headaches, and these therapeutic gains appeared to be maintained at follow-up.38 CBT is often delivered in conjunction with pharmacotherapy. A randomised controlled trial looking at adolescents with chronic migraine that were all treated pharmacologically with amitriptyline indicated that those patients who were also treated with CBT had greater reductions in days with headache and migraine-related disability compared to those treated with headache education plus amitriptyline.39 Many studies have shown a beneficial effect of CBT on headaches and its psychological comorbidity (mainly depression and anxiety),30,38 yet many young people do not receive psychological treatments for chronic pain due to barriers such as a shortage of providers, expense, and geographic distance from treatment centres.40 A Cochrane review aiming to assess the effectiveness of psychological therapies delivered remotely and comparing them to waiting-list, treatment-as-usual, or active control for the management of chronic pain in children and adolescents is being undertaken.38 Its conclusions may shed light on the preferred non-pharmacological modality for treating these young patients.
Internet-Based Self-Help Behavioural Techniques
With the widespread use of the internet by young people, many internet-based self-help strategies were developed, aiming to relieve challenging emotions/experiences/situations in children and adolescents’ lives. Among them are self-help techniques for relieving the burden of recurrent headaches. A randomised controlled trial compared three self-help internet based techniques: CBT, applied relaxation, and education intervention. All techniques showed a significant reduction in headache frequency and duration, but not in headache intensity and health-related quality of life. CBT showed the highest reduction in headache frequency.41 A randomised trial of a web-based intervention to improve migraine self-management and coping for adults with migraine showed promising results in increased headache self-efficacy, increased use of relaxation, increased use of social support, decreased pain catastrophising, decreased depression, and decreased stress.42 A pilot study assessing the feasibility and preliminary effectiveness of an internet-delivered CBT intervention for adolescents with chronic headache did not demonstrate a beneficial effect for the CBT group. However, both groups reported high levels of engagement with the web programme and reported satisfaction with the intervention.43 More prospective well-controlled studies are required to reliably assess the effectiveness of different web-based interventions.
Nutraceuticals
Many patients and families of children and adolescents who have a chronic condition turn to nutraceuticals, which they believe is ‘a more natural way’ than pharmacotherapy for treating their condition.44 The word ‘nutraceuticals’ is a portmanteau of the words ‘nutrition’ and ‘pharmaceutical’, and the term is applied to products that range from isolated nutrients, dietary supplements, and herbal products to specific diets and processed foods. Alone and in combination, magnesium, riboflavin, coenzyme Q10, and the herbal extracts of butterbur, feverfew, and ginkgolide B have all been suggested as preventatives for migraine.45 It is postulated that intracellular magnesium may be decreased in migraineurs, resulting in a decreased migraine threshold through a number of interdependent pathways. Riboflavin is a precursor for flavin compounds necessary for mitochondrial oxidation, which may be impaired in migraineurs.45 Coenzyme Q10 is necessary for electron transport, exhibits anti-inflammatory properties, and has been shown to be protective against glutamate toxicity, which is thought to play a key role in the pathogenesis of migraine. Butterbur extract (Petasites) was shown to have antispasmodic, anti-inflammatory, and vasodilator properties.46 However, in spite of the growing basis of knowledge about nutraceuticals and their possible therapeutic effects, studies involving paediatric patients looking at the use of a single or combination of nutraceuticals in the treatment of paediatric headache are still missing.
SUMMARY
Primary headaches are common among children and adolescents, with migraine and TTH being the most common types. In this review, we have summarised the recommended treatment strategies, pharmacological and non-pharmacological alike. The specific treatment should be tailored according to patient age, family structure, culture and beliefs, headache diagnosis, and according to the disability the headache imposes on the patient’s daily life.3 Having reviewed the literature, it seems safe to suggest that the recommended approach to treatment of primary headache in children and adolescents is the multidisciplinary approach. This approach is comprised of education, ongoing support, behavioural techniques, and medications as needed, and takes into consideration the stage of development the young patient is at. The multidisciplinary approach was shown to improve multiple outcome variables, such as frequency and severity of headache, school days missed, stress levels, anxiety, etc. Further studies regarding application of new neuroimaging techniques will most likely improve our understanding of the pathophysiology of primary headache, and our ability to accurately diagnose the young patients. Further studies on different modalities of treatment, alone and in combination, will assist physicians to better serve their young patients, who struggle with the common and burdening phenomenon of headache.








