Abstract
Background: Neurosyphilis can manifest as recurrent brain infarction, although not frequently, but can be challenging to diagnose due to atypical presentations.
Case report: A 43-year-old male with history of smoking presented to the Midland Regional Hospital, Tullamore (MRHT), Offaly, Ireland, with focal speech deficit and arm/leg weakness for 3 days. Neuroimaging showed acute cerebral infarction. He denied any high-risk sexual contacts. Forty-eight hour telemetry, trans-thoracic echocardiogram, cerebral catheter angiogram, and magnetic resonance angiogram were normal. He was treated with high-dose aspirin for 14 days and then discharged on aspirin with a follow-up plan. Trans-oesophageal echocardiogram performed after 2 weeks showed no evidence of subacute bacterial endocarditis, but there was evidence of fibroelastoma on the aortic valve. The cardiology department felt this was not a likely cardioembolic source.
The patient presented 2 months later with recurrent stroke symptoms of loss of speech to another hospital. However, he was discharged for follow-up in MRHT as symptoms resolved. Brain computed tomography (CT) showed ‘old’ stroke. One week later he re-presented to MRHT with dysarthria, ataxia, and a National Institute of Health Stroke Scale (NIHSS) score of three. Repeated neuroimaging showed multiple ‘new’ and ‘old’ cerebral infarcts. The patient was anticoagulated based on recurrent thromboembolic events and magnetic resonance imaging was repeated. CT aortogram and 48-hour Holter results were normal. A repeated magnetic resonance angiogram showed multiple stenosis areas due to vasculitis. As aetiology was complex, a lumbar puncture was performed and blood tests repeated (viral serology, vasculitic and thrombophilia screens). Cerebrospinal fluid and serum analysis displayed a diagnosis of neurosyphilis with co-infection of HIV. Treatment with penicillin was commenced, after which the patient greatly improved and is now under long-term follow-up.
Conclusion: Stroke in a young patient is rare and recurrent stroke-like events in a young person raise the clinical suspicion of an alternative diagnosis. It is therefore imperative to investigate neurosyphilis in all HIV-positive patients, as it can cause early clinical manifestation in such patients.
SUMMARY
Neurosyphilis has different clinical manifestations, which include recurrent ischaemic stroke. We report a case of a 43-year-old male who presented multiple times to the Midland Regional Hospital, Tullamore (MRHT), Offaly, Ireland, with recurrent dizziness, blurred vision, and lower limb weakness. Neuroimaging demonstrated multiple areas of infarction on three different presentations. On further evaluation of the cause of his recurrent stroke-like presentations, a diagnosis of neurosyphilis and co-infection with HIV was made after lumbar puncture results, as both cerebrospinal fluid (CSF) and serum analysis showed a positive rapid plasma reagin (RPR) test and a positive treponema pallidum particle agglutination (TP-PA) assay. Serum samples were also positive for HIV antibodies. Treatment with penicillin was commenced, after which he showed drastic improvement and did not develop any further ischaemic stroke. The patient is also on highly active antiretroviral therapy (HAART) for HIV and is now under long-term follow-up.
CASE REPORT
Background
Ischaemic stroke under the age of 45 years is not as common as ischaemic stroke in older ages. Reported stroke incidence is variable with an annual incidence of 10 per 100,000 in the UK. A total of 50% of these cases are ischaemic (compared with 85% in older patients). Major causes of stroke include cardioembolism (the most common cause, representing 20–30% of strokes) and arterial dissection, which causes 2% of all strokes. Other causes include thrombophilia, vasculitis, viral infection (cytomegalovirus, varicella zoster virus, HIV), neurosyphilis, and tuberculous meningitis.1
Neurosyphilis can occur during any stage of the disease and is divided into early and late stages. It can manifest in many different ways, which means diagnosis can be challenging and is therefore often delayed. It is an easily treatable illness and is important to diagnose early. If the patient has co-infection with HIV, the disease becomes clinically evident quickly and extensively.2 If it presents as recurrent stroke, it becomes more important to ensure early diagnosis, in order to prevent extensive damage to the brain and hence the neurological functioning of such patients.
The incidence of syphilis is drastically increasing worldwide. European data shows that overall syphilis rates have been increasing since 2010, predominantly among the male population. Almost two-thirds of these cases have been reported in men who have sex with men (MSM). In the USA, the number of primary and secondary syphilis cases has been continually rising each year since 2000. The national syphilis rate in the USA between 2014 and 2015 was the highest rate reported since 1994. Again, this increased rate is largely attributable to increased cases in the male population, specifically among MSM.
Case Presentation
A 43-year-old male presented to the emergency department with a 3-day history of slurred speech and dizziness accompanied by lower limb weakness. On further questioning, this was reportedly his second episode of dizziness in the past 2 months. He had no previous medical history and he was not on regular medication. He was a smoker, with a history of smoking 30 packs of cigarettes a year, and drank alcohol socially. He was single, living alone, and he denied any high-risk sexual contact; however, he admitted to being involved with MSM. Physical examination was normal and there was no focal neurological deficit or signs of cognitive impairment, apart from mild expressive dysphasia.
Neuroimaging showed three areas of old infarction. Forty-eight hour telemetry, trans-thoracic echocardiogram, and magnetic resonance angiogram (MRA) were normal. He was treated with high-dose aspirin for 14 days and discharged on aspirin 75 mg once daily with a follow-up plan. Transoesophageal echocardiogram (TOE) performed after 2 weeks showed no evidence of subacute bacterial endocarditis, but did show fibroelastoma on the aortic valve. The cardiology department felt it was not a likely cardioembolic source and recommended antiplatelet therapy and computed tomography (CT) aortogram.
The patient presented 2 months later with recurrent stroke symptom of loss of speech to another hospital. However, he was discharged for follow-up in MRHT as symptoms resolved. A subsequent brain CT showed an old stroke. One week later he re-presented to MRHT with dysarthria, ataxia, and a National Institute of Health Stroke Scale (NIHSS) score of three. Repeated neuroimaging showed multiple new and old cerebral infarcts. As TOE showed suspicion of vegetation in the aortic area, it was suggested to start anticoagulation along with antiplatelet therapy until a definite diagnosis was reached. Magnetic resonance imaging (MRI) and MRA were repeated. CT aortogram, CT intracranial vessels, and 48-hour Holter were normal. There was no clinical evidence of sepsis. A neuroradiological review of repeated MRA showed multifocal stenosed areas in the left middle cerebral artery, right anterior cerebral artery, and basilar artery, suggesting vasculitis, and therefore 30-day Holter was not considered until later.
As the aetiology was complex, lumbar puncture was performed and blood tests repeated (viral serology including varicella zoster serology and vasculitic and thrombophilia screens). CSF and serum analysis displayed the diagnosis of neurosyphilis with co-infection of HIV; CSF for other virology like cytomegalovirus and varicella zoster virus was negative. Treatment with penicillin was commenced, after which, the patient greatly improved and he is now under long-term follow-up. He is currently also on HAART. Since HIV is also a known cause of ischaemic stroke by several mechanisms (such as coagulopathy and vasculopathy), co-infection with neurosyphilis and a CD4 cell count >200 makes it less likely to be caused solely and directly by HIV.2
Investigations
A CT brain scan on his first presentation demonstrated three separate areas of non-haemorrhagic infarction, in the left inferior frontal lobe, left superior frontal lobe (both of uncertain age), and a small infarct in the left posterior parietal lobe which appeared to be acute. An MRI brain scan showed a focal area of diffusion weighted images, identified in the posterior aspect of the left parietal lobe (Trial of ORG 10172 in acute stroke treatment [TOAST] Classification 4 [stroke of other determined aetiology]) consistent with acute cerebral infarction. It also showed old cerebral infarcts in the left frontal lobe and anterosuperior aspect of the left parietal lobe as well as an old lacunar infarct in the left basal ganglia. There was a small focal area of high signal intensity in the left thalamus consistent with chronic ischaemic disease (Figure 1).
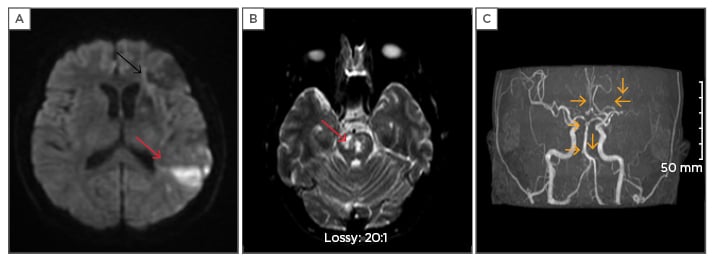
Figure 1: Images of the patient.
A) DWI during first presentation of the patient; acute infarct (red arrow) parietal area with old infarct frontal area (black arrow); B) DWI during the third presentation; acute infarct (red arrow) in pons; C) MRA showing multifocal areas (yellow arrows) of stenosis in left middle cerebral artery (M1, M2), right anterior cerebral artery, left anterior inferior cerebellar artery, basilar artery.
DWI: diffusion weighted imaging; MRA: magnetic resonance angiography.
CT aortogram and cerebral catheter angiogram were normal and the MRA brain scan performed at the same time was also normal. In repeated MRA brain scans, the neuroradiologist commented on the presence of multiple irregular stenoses including left M2 right anterior cerebral artery and basilar artery stenosis secondary to vasculitis. As part of his stroke work-up, the patient had a transthoracic echocardiogram, which was normal; a Holter monitor, which demonstrated sinus rhythm; and a normal carotid Doppler.
Thrombophilia screen, janus kinase 2 (JAK-2) mutation tests, homocysteine levels, viral serology for cytomegalovirus and varicella zoster, QuantiFERON®, acid-fast bacilli smear, antiphospholipid antibodies, autoantibody screens, and anti-neutrophil cytoplasmic antibody tests were all negative. Immunoglobulin and complement levels, lipid screen, HbA1c test, vitamin B12, folate, and ferritin were all within normal range. MRI brain scan repeated on re-presentation showed a new area of infarct in the anterior aspect of pons, consistent with acute brainstem infarction.
A TOE showed an aortic valve lesion suggestive of a fibroelastoma in the aortic valve which was not attributed to be a possible cause of his multiple infarcts; however, he was started on dual antiplatelet therapy. At this point it was decided that he should have CSF and serum testing for syphilis and HIV. CSF analysis demonstrated high protein levels of 76.2 mg/dL and a high white cell count 60/mm3; 95% mononucleated, 5% polynucleated. The CSF tested positive for TP-PA 1:10240 and rapid plasma reagin test 1:1. The serology showed rapid plasma reagin test positive 1:8, TP-PA immunoglobulin M positive, TP-PA positive 1:1520 and HIV antigen/antibody positive, confirmed on HIV confirmation assay. A diagnosis of neurosyphilis and HIV was made based on these results. The patient also had a CD4 cell count of 600 cells/mm3 and a viral load of 13,467 copies/mL.
Differential Diagnosis
Initially, echocardiogram, 48-hour Holter monitor, carotid Doppler, thrombophilia, vasculitis, autoimmune test, HbA1c, lipid screen, and viral studies were negative. Therefore, cardioembolic strokes were a possibility given that the patient had a lesion on his aortic valve on TOE; however, it was considered less likely, particularly as he had one episode of stroke. Despite treatment with anti-platelet agents given his strong family history of strokes at a young age, cerebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy and Fabry disease were considered as potential causes.
Treatment
He was treated with 14 days of intravenous penicillin G, as per current guidelines3,4 as well as commenced on HAART. Dual antiplatelet was stopped and single antiplatelet was continued, considering smoking as another risk factor of stroke for the patient.
Outcome and Follow-Up
After treatment with penicillin his condition improved and he has not suffered any further strokes or neurological symptoms. He has now been referred for an ophthalmology appointment as part of routine assessment for neurosyphilis. He is under long-term follow-up by infectious disease specialists for HIV and neurosyphilis and is due for repeat CSF examination. The patient was followed up in the outpatient clinic on a regular basis, first fortnightly then every 3 months. Recent follow-up showed improvement in speech, no more recurrent symptoms of dizziness/slurred speech, no detection of viral load, and the CD4 cell count was 300 cells/mm3. Repeated CSF analysis is advised.
DISCUSSION
Syphilis is a sexually transmitted systemic disease caused by the spirochete Treponema pallidum. Humans are the only known hosts. It is divided into stages of primary, secondary, and tertiary syphilis and both primary and secondary stages are infectious. Tertiary syphilis is slowly progressive and comprises three types: cardiovascular, late benign (i.e. gummatous), and neurosyphilis.
Neurosyphilis is variable in its presentation and can mimic other diseases, hence the diagnostic challenge. Early neurosyphilis can be asymptomatic or can present as an aseptic meningitis. Late neurosyphilis is variable in its presentation but there are three main syndromes: meningovascular, general paresis, and tabes dorsalis. General paresis often presents with cognitive decline, dementia, or psychosis. Tabes dorsalis is the demyelination of the dorsal columns and leads to sensory disturbance and severe pain.5-7 Meningovascular syphilis can lead to focal ischaemia, causing symptoms of stroke. The underlying pathology of meningovascular syphilis is focal endarteritis of the medium and large vessels with associated perivascular inflammation.8 The likelihood of meningovascular syphilis is increased in HIV-positive patients and its course can be accelerated in this immunocompromised group.9,10 HIV is also implicated in the causation by different ways, including vasculitis, but the mechanism involves direct vasculitis or opportunistic infections, like meningovascular syphilis (as in this case), varicella zoster vasculitis, or tuberculous meningitis (both negative in our case). Vasculitis directly caused by HIV is only considered when CD4 cell count is <200 mm3 and opportunistic infections are excluded.2,9
There have been numerous cases reported in the literature of neurosyphilis presenting as a stroke or stroke-like syndrome. Abkur et al.11 described a patient with a similar clinical picture; however, in that case there was no infarct or ischaemia demonstrated on neuroimaging. Patira et al.12 also described a similar case to ours of a young man presenting with an ischaemic stroke who was subsequently diagnosed with HIV and neurosyphilis. There have also been recent cases reported of neurosyphilis presenting with confusion, psychotic symptoms, personality changes, and Parkinsonism.10,13-17 It is important to document these cases in the literature so that clinicians are aware of the myriad of ways in which neurosyphilis can present and they can recognise that it should always be considered as a differential diagnosis in young patients with unexplained neurological symptoms.
Our case illustrates how a high index of clinical suspicion is critical in young patients who present with stroke-like symptoms, including those with demonstrated infarcts. Neurosyphilis is treatable and early diagnosis is essential. With rates of syphilis on the rise, this is likely to become even more significant. It is important to remember that there is a high proportion of HIV-infected patients who are co-infected with syphilis, and therefore all patients who are diagnosed with neurosyphilis should be tested for HIV.9,10,17
LEARNING POINTS
- Neurosyphilis should always be considered as a diagnosis in young patients with recurrent strokes or stroke-like symptoms.
- Neurosyphilis should always be out ruled as a secondary cause where cerebral vasculitis is suspected, even if there is no documented history of primary syphilis or skin rash.
- In patients diagnosed with neurosyphilis, HIV should always be tested for.10,17
- Even though our patient had a strong family history for young strokes, it is important to remember that it may be incidental and other causes need to be equally investigated.








