BACKGROUND
T-lymphoblastic lymphoma (T-LBL) is a neoplasm of immature T-cell precursors or lymphoblasts.1 This neoplasm tends to occur in older adolescents, with a male predominance.1 T-LBL usually presents as an anterior mediastinal (thymic) mass with supradiaphragmatic lymphadenopathy and variable splenic, hepatic, and bone marrow involvement (with leukaemic phase of the illness).2 T-cell acute lymphoblastic leukaemia localised to the central nervous system (CNS) represents <5% of cases, and does not have the subsequent systemic evolution of usual cases of acute lymphoblastic leukaemia.2-4
METHODS AND MATERIALS
Multiple diagnostic tests can be undertaken in assessment of suspected cases of T-LBL: somatic and neurological examination; laboratory tests including flow cytometric (FCM) immunophenotyping of cerebrospinal fluid, antiphospholipid antibody, rapid plasma reagin, and HIV testing; MRI of the head; X-ray of the thorax; coronary angiogram; lymphocytic choriomeningitis testing; and trepan biopsy of bone marrow.
CLINICAL CASE
This summary presents a clinical case of a 44-year-old patient admitted to the emergency department with complaints of progressively increased headache, stiffness of the neck, impaired co-ordination, nausea, vomiting, and irritation from noise and light. Consent to publish this case was obtained from the patient’s family. The patient had a meningeal syndrome, and MRI showed a tumour in the left cavernous sinus area.
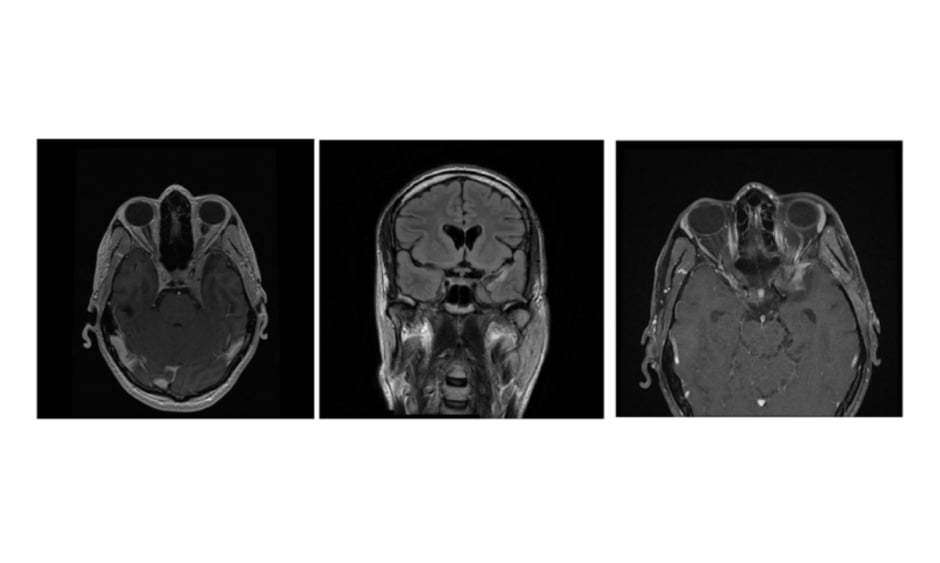
The patient had a history of peripheral facial nerve palsy, and MRI showed extra-axial tumour formation in the left cavernous sinus area and retro-orbital area (Figure 1). Biopsy was performed 3 months earlier and the histology showed partially hyalinised connective tissue. Blood testing showed a slightly increased troponin I at 1,761.4 pg/mL, C-reactive protein of 25.4 mg/L, a negative QuantiFERON-TB Gold test, negative tests for hepatitis B and C, antiphospholipid antibody, and HIV, and negative rapid plasma reagin test. The X-ray of the thorax was without pathological changes.
Figure 1: T-lymphoma MRI images.
Because of the laboratory constellation of results, coronary angiography was performed; no stenosis or thrombosis were observed. A lumbar puncture was performed because of the meningeal syndrome; examination of the cerebrospinal fluid showed lymphocytic pleocytosis and atypical cells in different phases of mitosis, with a negative result for lymphocytic choriomeningitis. Trepan biopsy of bone marrow was without pathological changes. FCM of cerebrospinal fluid was diagnostic for T-lymphoblastic leukaemia/lymphoma. Intrathecal chemotherapy was started.
CONCLUSION
CNS T-LBL is a rare disease with an incidence of approximately 51 cases per 10 million per year.5,6 Differential diagnoses include aseptic meningitis, brainstem glioma, granulomatous angiitis, neurological infections, neurosarcoidosis, and neurosyphilis.5 FCM of cerebrospinal fluid could help to make the right diagnosis.7 FCM is a highly sensitive technique capable of detecting malignant cells.7,8,9 FCM can detect CNS disease before the manifestation of clinical symptoms; the routine use of flow cytometry and cytology may permit the earlier detection of neoplasm.