Meeting Summary
This article is based on a Learning Lounge educational session that took place on 22nd October 2022, as part of Infectious Diseases Society of America (IDSA) IDWeek™ 2022 held in Washington, D.C., USA. The objectives of the Learning Lounge were to enhance understanding of the principal reasons for patients’ vaccine hesitancy based on key sociocultural, behavioural, and psychological factors; identify the general communication ‘cues’ and specific psychosocial objections that signal a patient’s inclination to vaccine bias; and help healthcare professionals (HCP) learn how to address vaccine hesitancy based on patients’ cognitive and behavioural biases. The knowledge shared in this Learning Lounge can help guide and assist HCPs in recognising and addressing vaccine hesitancy, thereby supporting effective conversations with patients and/or their caregivers, and drive more personalised solutions to improve acceptance of vaccinations. The Learning Lounge was hosted by Christopher Graves, Founder and President of the Ogilvy Centre for Behavioral Science, New York, New York, USA., who is an expert on vaccine hesitancy and guiding HCPs on recognising and addressing this phenomenon. Graves was joined by Wendy Wright, Partners in Healthcare Education, LLC, Bedford, New Hampshire, USA, and Todd Wolynn, Kids Plus Pediatrics, Pittsburgh, Pennsylvania, USA, in a roleplay discussion to highlight cognitive biases that are relevant to vaccine hesitancy, and how these might be addressed in clinical practice.HOW DO HUMANS MAKE DECISIONS?
According to Graves, important considerations for effectively addressing vaccine hesitancy include understanding behavioural science, particularly how an individual’s construct of reality is formed, as well as the process and rationale behind decision making. Emotion can be a driving force in all decisions.1 There are two specific areas of the human brain that are suggested to act in concert to enable decision making: the amygdala and the ventromedial prefrontal cortex.2,3 The amygdala is responsible for the original raw fight or flight in the brain, which is believed to be instrumental in evolutionary survival,4 and is likely to be an emotional governor or ‘senior partner’ in decision making.1 The ventromedial prefrontal cortex is a more evolved part of the brain that is considered to make sense of the raw emotional signals that are received from the amygdala.2,3
Two co-existing modes of human thinking in decision making have been proposed. System 1 is the default mechanism, a quick, automatic, intuitive, emotion-based system that is utilised in 95% of decision making;5,6 while System 2 is a slower, more demanding, and far more accurate non-emotion-based system that uses approximately 5% of the brain’s energy.5 However, despite the emotional governance always working below our conscious level in System 1, the brain has its limitations. Cognitive bias is a subconscious systematic error in thinking that occurs when people are processing and interpreting information in the world around them, and this affects the decisions and judgements that they make.7
THE ENHANCED HEALTH BELIEF MODEL
Awareness of the Health Belief Model (HBM Figure 1) may help HCPs to better understand vaccine hesitancy. The HBM was developed in the early 1950s by social scientists at the U.S. Public Health Service (USPHS) to attempt to predict health-related behaviour in terms of certain belief patterns.8,9 The enhanced health belief model assumes that people will take a health-related action if they believe that a negative health outcome can be avoided, and believe they can be successful in enacting the recommended action.9
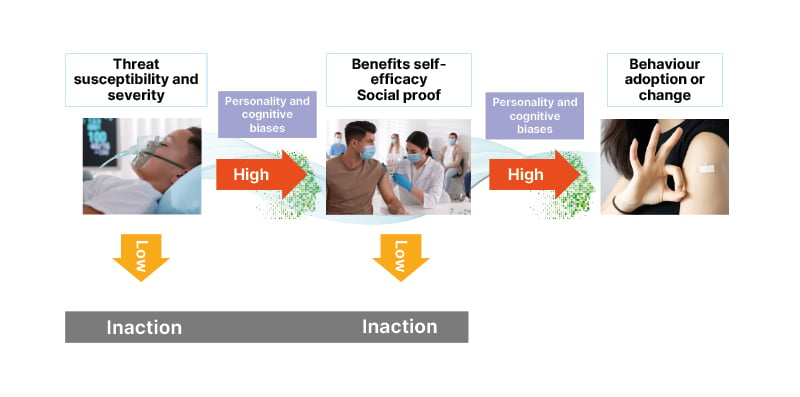
Figure 1: Enhanced Health Belief Model.9
For anyone to adopt a health behaviour or make a change, they must first view the threat as real and potentially severe.9 They must also believe that they personally are vulnerable, and that the initiated health behaviour or change works, and is less risky than doing nothing.9 Further, they must see that other individuals believe in the behaviour or change.10,11
It is suggested that the inclusion of the understanding of the cognitive biases, and the innate, internal wiring of personality and thinking styles would enhance the current health model.9,12 Assisting HCPs in ‘decoding’ the internal brain wiring would help them to reframe communications and interventions to resonate, and not clash, with the way the patient views the world.
Cognitive Biases Most Relevant to Vaccine Hesitancy
Awareness of the biases most relevant to vaccine hesitancy (as described below) would help HCPs to recognise these biases during conversations with their patients, thereby enabling them to drive effective conversations that do not conflict with their patients’ views.
Availability bias
The disparity between what people fear and the real causes for fear is representative of availability bias, denoted as ‘the more easily we can picture a threat, the more we value it’.7,13
Optimism bias
The optimism bias is when ‘we believe we can beat the odds’, the chances of good things happening are overestimated, and personal vulnerability to certain threats is underestimated.7
Omission bias
The omission bias refers to ‘when we fear the consequences of our own action, so we do nothing’.7 In terms of vaccination, such inaction by parents or caregivers may place children at risk.7
Confirmation bias
The confirmation bias denotes the consequences when facts conflict with personal beliefs.7 Individuals only accept the evidence that confirms their pre-existing beliefs and take cues from the beliefs of their tribe or group, resisting exclusion from the group.7 The key behavioural biases that impact vaccine uptake are summarised in Figure 2.
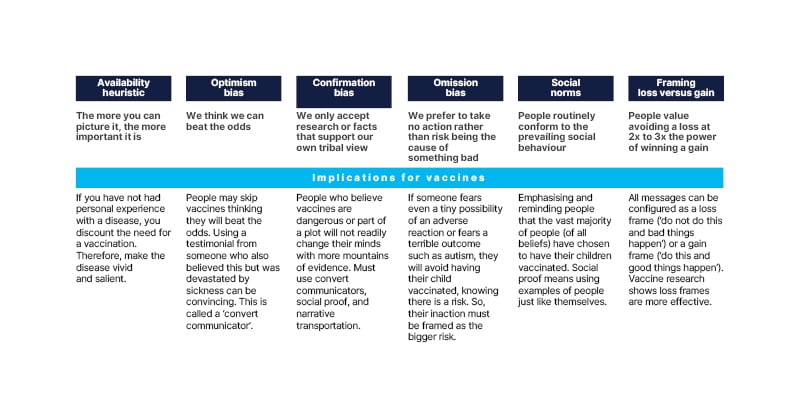
Figure 2: The key behavioural biases that impact vaccine uptake.7,10,13-22
VACCINE HESITANCY IS NOT A NEW PHENOMENON
In 2019, prior to the COVID-19 pandemic, vaccine hesitancy was considered by the World Health Organization (WHO) to be a top 10 threat to global health.23 People have been suspicious of vaccines since variolation, an early form of inoculation against smallpox, which was first used in the 1720s.24 Despite technological and medical advancements over the past 300 years, the COVID-19 pandemic has highlighted that reluctancy regarding immunisation still exists.25-27
ADDRESSING VACCINE HESITANCY: PRECISION MEDICINE-LIKE APPROACH RATHER THAN ‘ONE-SIZE-FITS-ALL’
Vaccine hesitancy is complex and not just about information and education. It has to do with human behaviours that can be separated into several categories, including complacency, distrust, identity, beliefs and world views, the unnatural, and a fear of harm (Ogilvy, unpublished data).
It is important to understand the reasons behind these behaviours in order to develop potential solutions that may lead to greater vaccine acceptance. Behavioural science teaches us that the approach to vaccine hesitancy should not be a ‘one-size-fits-all’ inoculation against misinformation or hesitancy.28 A more precision medicine-like approach, in which clinical management is tailored to the individual patient based on their predicted response or risk of disease,28 will be required to help build vaccine confidence. This means that HCPs need to respectfully and empathetically ‘decode’ individuals before engaging with them and trying to convince them to get vaccinated.
WHERE HUMAN BIAS AND MESSAGING CONVERGE
How patients are internally wired, their world view, and risk propensity affect how successful an HCP will be in communicating the purpose and importance of vaccination.
One of the elements that make up this internal wiring is ‘cultural cognition’, which refers to how individuals care differently about things depending on their personal and group identity, and whether these beliefs conflict with those of others.29,30
Social norms refer to the sense of what most people are doing,18 whereas social proof encompasses observing what people similar to the individual are doing.10,11 Identity and being part of a group are extremely important,10,31 and leveraging tribal beliefs and pride is incredibly powerful.32,33 It is essential to include the principles of the group in health communications surrounding vaccination.17,34
Messages about vaccination clearly cannot be generic, as a patient’s or caregiver’s world view is tied to their behaviour regarding vaccines.28 All messages can be crafted as a ‘gain frame’ or a ‘loss frame’.21 A gain frame means ‘if you do this, good things will happen’, whereas a loss frame means ‘if you do not do this, bad things could happen’.21 Humans are a loss-averse species, so they generally value avoiding a loss at two- to three-times the power of winning a gain.19,20 Hence, decoding the individual is vital to enable HCPs to address vaccine hesitancy more effectively.
A presumptive voice of authority (‘your child is going to get two vaccinations today’) has been shown to create far less resistance to vaccination compared with a participatory voice of empathy (‘your child needs some vaccinations, would you like to discuss any concerns?’).35 Also, interestingly, studies testing message framing surrounding vaccine intentions showed that loss framing (‘if you do not do this, bad things could happen’) was more effective than gain framing (‘if you do this, good things will happen’).22 HCPs should be mindful of their approach to addressing vaccine hesitancy, and carefully research which threat they use to alert the patient or their caregiver during discussions regarding immunisations.
It is important for HCPs to identify cognitive bias in their patients, and use this knowledge to drive conversations to help support vaccination within their own framing. Examples of how this can be achieved were provided through roleplay discussions at the congress, summarised below.
VACCINE HESITANCY ROLEPLAY DISCUSSION
Three different vaccine hesitancy scenarios and how they might be addressed in clinical practice are summarised as follows.
Scenario 1: ‘My Child is Not at Risk’
Cognitive biases present
The availability bias (the patient’s mother could not picture the threat of human papillomavirus [HPV] disease) and the optimism bias (the mother did not think her child was at risk).
Scenario
An HCP recommends meningitis, HPV, and tetanus, diphtheria, and pertussis vaccines for an adolescent female. The patient’s mother is hesitant about the HPV vaccine because they think their child is not sexually active, is not at risk for HPV, and is too young to need the vaccine.
Healthcare Professional’s response
The best time to get protected against HPV disease is well before there is any chance of exposure to the virus. Vaccination before risk of exposure is like wearing a car seatbelt at all times (i.e., before there is a potential risk of collision).
Appraisal
This analogy is an effective approach to underscore that the future is unknown, and it is important to prepare now for unidentified future consequences.
Scenario 2: ‘I am Not at Risk’
Cognitive biases present
The availability bias (the patient could not picture the threat of disease, misinformation is more salient), the omission bias (rather take no action than do something that may cause harm), and the optimism bias (‘I can beat the odds, I will not get sick from influenza or COVID-19’).
Scenario
An HCP discusses influenza and COVID-19 vaccination with an adult male patient. The patient is vegan and ‘super healthy’ and is hesitant to take any vaccines because of their ‘foreign or chemical content’.
Healthcare Professional’s response
Eating well and exercising are important for health but, just like a workout, vaccines can contribute to staying healthy and strengthen the immune system to enable a response on exposure to infection.
Appraisal
This reframing of vaccination as a way to help strengthen the immune system to help fight disease is an effective approach.
Scenario 3: ‘Social Proof’ Discussion
Cognitive biases present
The availability bias (vaccine misinformation), the omission bias (rather take no action than do something that may cause harm), and the confirmation bias (looking for information that supports what we already believe).
Scenario
An HCP recommends the COVID-19 vaccine for a child. The child’s mother is hesitant because they have read on social media about children becoming ill after vaccination and is concerned that the vaccine is not safe.
Healthcare Professional’s response
Millions of children in the USA have received at least one dose of a COVID-19 vaccine, which has been shown to be safe for children.
Appraisal
Social proof principles (i.e., millions of children have been vaccinated), and correcting misinformation (explaining that the vaccine has been demonstrated to be safe) are effective in this scenario.
CONCLUSION
It is important to enhance understanding of the principal reasons for patients’ vaccine hesitancy based on key sociocultural, behavioural, and psychological factors. Identification of general communication cues and specific psychosocial objections that can signal a patient’s inclination to vaccine bias is also imperative, and may guide potential solutions for patients who refuse immunisation. This knowledge may help guide HCPs to recognise vaccine hesitancy and address patients’ cognitive and behavioural biases, thereby enabling them to initiate effective conversations with patients and/or their caregivers, and drive more personalised solutions to improve acceptance of vaccinations.
COM-GL-COV-2200222 01/23
Click here to view the full presentation on Using Behavioural Science to Help Understand Vaccine Hesitancy.








