The convergence of three viral epidemics, respiratory syncytial virus (RSV), COVID-19, and influenza, during 2022–2023, placed a significant burden on healthcare systems nationally. While there was regional variation in timing and intensity of disease spread, as well as severity of illness, by early November 2022, an estimated 80% of USA regions had already neared their expected seasonal peak levels in RSV, several months ahead of its typical peak in early February.1 Nearly 50% of USA regions reported high or very high levels of influenza activity,2 months ahead of expected seasonal peaks.3 Meanwhile, COVID-19 continued to circulate in the background, with 2% of USA counties, districts, or territories reporting high COVID-19 community level, and 20% reporting medium community level during the same period.4
The co-circulation of these three respiratory viruses is not new, and indeed, all three viruses circulate year-round, and experience peaks during winter months. However, the prematurity, rapidity, and simultaneity of their surges in 2022–2023 uniquely taxed health systems, and challenged the way they approach preparedness and response for more common respiratory diseases in the wake of the COVID-19 pandemic and an era of climate volatility. Here the authors describe the emergency preparedness and response experiences of NYC Health + Hospitals, New York, USA, during the 2022–2023 ‘tripledemic’, as it was popularly dubbed, and further call attention to critical equity considerations in how hospitals and health systems prepare for and respond to such events.
THE ‘TRIPLEDEMIC’ IN NEW YORK CITY
At NYC Health + Hospitals, New York City’s public healthcare system, and the nation’s largest municipal healthcare system, the unanticipated simultaneous surge in three respiratory viruses created need for time-sensitive coordination, principally targeting three goals: first, to improve comprehensive situational awareness to support efficient local and systemwide response needs; second, to decrease demands on acute care resources that were created by the patient surge; and third, to increase those resources to care for surging demand, particularly in areas of staff and supplies.
Improving Situational Awareness
Real-time situational awareness, meaning information about the current or anticipated extent of emergency, including resources and operations necessary for response, is critical to any response coordination. At NYC Health + Hospitals, situational awareness was provided to central and local response teams through two primary approaches: co-ordination groups and analytic tools.
NYC Health + Hospitals’ Central Emergency Management team activated a number of co-ordination groups to provide regular, subjective real-time information. A ‘Pediatric Action Team’ (PAT) was activated, consisting of selected pediatric clinical subject matter experts from a variety of fields (pediatric emergency medicine, pediatric intensive care unit [PICU], general pediatrics, etc.) from several of the NYC Health + Hospitals facilities, and provided both on-the-ground feedback regarding patient volumes, acuities, resource availability; and response operations and needs. A separate co-ordination group brought together broad hospital pediatrics and facility executive representation to identify challenges from departmental and facility perspectives, and to share response strategies and progress for further dissemination to frontline staff. Finally, the system’s Multi-Office Coordination (MOC) Group brought together system clinical, operational, public affairs, and intergovernmental leadership, and teams to co-ordinate response actions leveraging systemwide, and external resources, informed by needs at other levels. To ensure alignment of all groups, Central Office Emergency Management led co-ordination of all three groups.
Beyond co-ordination groups, situational awareness was gleaned from a number of real-time analytic tools. While NYC Health + Hospitals had existing reporting tools available to provide real-time awareness of patient trends, including as part of their electronic health record, not all of these tools were available to all response participants, especially those without appropriate electronic health record access. Moreover, additional response metrics were required beyond those in production, and thus, new tools were necessitated. NYC Health + Hospitals’ Data & Analytics team, building on experiences in COVID-19 and mpox outbreaks, developed tools to measure percentage of patients admitted with viral syndromes, trends of positive test cases (Figure 1), volumes in pediatric emergency departments, and outpatient clinic volumes. As Figure 1 shows, the peak timings of all three respiratory viruses varied, with RSV peaking around mid-November 2022, influenza peaking around late November and into December 2022, and COVID-19 peaking around early November 2022. The information gleaned from these dashboards supplemented and informed subjective reports provided in co-ordination groups, and helped response leadership better understand the points of strain, and anticipate where energy and resources should be focused on clinical operations.
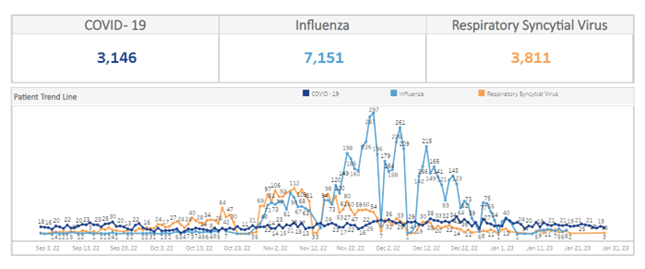
Figure 1: Trends in case counts of three respiratory viruses, September 2022–January 2023, NYC Health + Hospitals, New York, USA.
Decreasing Demand on Acute Care Resources
As case counts regionally increased, so too did media attention on the tripledemic, as well as public fear. Patients began to pour into the pediatric emergency departments and outpatient pediatric clinics. While the overwhelming majority of these patients had mild illness, the sheer volume of them threatened to overwhelm resources, and limit their availability for those most in need. As a result, NYC Health + Hospitals instituted several strategies aimed at reducing overall demand for acute care resources.
To address and assuage the mounting public uncertainty and fear motivating acute care demand, NYC Health + Hospitals instituted a communications strategy designed to engage all NYC Health + Hospitals patients. Communication provided lay guidance on the signs and symptoms of these respiratory viral infections, what to expect, and when and where to seek care. Communications referred patients to the system’s 24/7 virtual urgent care service, Virtual ExpressCare (VEC), where clinical evaluation could be delivered without burden on acute care registration, nursing, or clinical staff or resources, and often in a far shorter timeframe. VEC clinical teams, comfortable in the provision of COVID-19-related care for adults, were simultaneously equipped with educational materials regarding the prevalent pediatric respiratory illnesses, including the three present in the tripledemic, and a series of pediatric protocols were developed with pediatricians and physician associates with pediatric experience. The same VEC service was also offered on after-visit summaries for patients seeking care in acute care settings, as a means of short-term follow-up re-evaluation, should clinical status change or concerns develop after discharge, to avoid recurrent acute care use. In these ways, the public was equipped with an easily accessible and rapid alternative to acute care evaluation, which leveraged system subject matter expertise in a scalable fashion, to ensure comparable quality as in-person evaluation.
Although most children with respiratory illness were stable enough to remain at home with supportive care, some required admission. Several children with respiratory viral illness during this time required non-invasive positive pressure ventilation. As such, as the volume of patients rose, so too did intensive care unit (ICU) admissions, placing strain on system- and citywide pediatric critical care resources. In response, the PAT created several clinical guidance to help optimize ICU resources. Protocols were developed to support weaning of non-invasive positive pressure ventilation on pediatric floors, helping expedite clinical transfers from ICUs to floor units, and opening ICU bed capacity. A systemwide risk stratification tool and set of admission criteria were developed, to standardize admission decision-making for patients with RSV or viral syndromes. When patients did not meet such criteria, to help empower parents and caretakers to feel comfortable caring for infected children at home, discharge instructions were augmented to provide specific discrete instructions for patient and caretaker education. Collectively, these tactics helped ensure that all patients were able to receive the level of care needed, while optimizing and co-ordinating use of acute care resources for patients most in need.
Increasing and Safeguarding Supply of Critical Resources
Notwithstanding efforts to reduce demand on acute care resources, the system also implemented several strategies to increase the supply or capacity of critical response resources. Some resources were in short supply regionally or nationally, including amoxicillin to treat pneumonia co-infection, albuterol for patients with co-existing reactive airway disease, ventilators and high-flow nasal cannula units, and cribs for admitted infants. In some cases, resource shortages were significantly ameliorated through development and implementation of protocols (developed by the PAT) to promote use of clinical alternatives. For example, a reference guide helped clinicians systemwide adopt alternative antibiotics in lieu of amoxicillin, helping preserve resource availability, and maintain clinical quality when amoxicillin was in short supply nationally. Elsewhere, NYC Health + Hospitals leveraged stockpiles of resources to bridge supply chain gaps. With surges in inpatients, flex units were rapidly opened to accommodate additional volume, though experienced challenges fully operationalizing, given concurrent challenges in staffing them adequately. Regional surges in demand for pediatrics, and PICU-trained nursing staff, limited the availability of temporary staff traditionally used in such surge settings, and required innovative, but ultimately logistically-complicated methods, to identify existing nurses working in other clinical areas across the system (including adult service lines), whose relevant prior pediatrics or PICU experience and credentials enabled their reassignment to support pediatric services. Finally, in order to balance demand across a system with specialized resources concentrated in some facilities more than others, NYC Health + Hospitals transferred a small number of patients within its system from facilities with less to those with relatively greater resource capacity.
LESSONS LEARNED FROM THE TRIPLEDEMIC RESPONSE
Value of Pre-Developed Plans
While the tactics employed above were effective in helping minimize demand, and maximize resources to support all clinical care needs, many of these operations were developed in a just-in-time fashion. Specific co-ordination structures, plans, protocols, and clinical operations had to be developed in real-time, often limiting their implementation for days at minimum. Although the system had robust and prolonged recent experience with COVID-19 response, especially in an adult population, the tripledemic’s impact on the largely pediatric population underscored the importance of hazard non-specific clinical and operational emergency preparedness planning, as well as exercising among diverse types of clinical, operational, and administrative staff.
Value of Telehealth
The system’s response demonstrated, as it had during COVID-19, the invaluable use of operationally-centralized, on-demand, urgent care in responding to large surges in demand, and newly highlighted the feasibility of such virtual remote clinical services in addressing pediatric respiratory illness, including through use of just-in-time staff training and clinical protocols. Telehealth services provided a low-cost and highly accessible way for patients to access care in lieu of acute care and, in many cases, helped parents or caretakers comfortably care for their children at home, even as public and media attention toward the tripledemic threated to create alarm. The utilization of, and comfort shown toward, telehealth services during this surge showed that it can be a routine option for pediatric evaluation in the community, especially underserved ones.
Health Equity Considerations
As is true with most disasters, the burden of the tripledemic likely fell heaviest on historically underserved and marginalized communities. At the national level, prior research has shown that pediatric patients of color, and those from low-income or limited English proficiency families are more likely to experience worse hospital outcomes compared to other children.5 The same socioeconomic factors increase likelihood for hospitalization due to RSV. Children in these demographic groups are at increased risk for severe illness and complications from RSV and influenza, and may face additional barriers to accessing testing, treatment, and vaccination. Moreover, systemic racism impacts the quality of care that people of color receive, as well as reducing their likelihood to seek care for fear of mistreatment.6 Based on available data, RSV-related hospitalization rates for Hispanic patients of all ages were consistently higher than non-Hispanic patients throughout the respiratory illness surge.7
In responding to the tripledemic, NYC Health + Hospitals, as the largest provider of healthcare services to lower-income communities in New York City, took into consideration the health equity implications of the triple surge event. Communications were developed across multiple languages, telehealth services adapted to limited Internet capabilities, and resource capacity optimized to maintain care delivery capabilities, regardless of patients’ ability to pay.
CONCLUSION
The 2022–2023 tripledemic presented a challenge to health systems in New York City, including NYC Health + Hospitals. Response priorities focused on strengthening co-ordination across clinical and operational disciplines, across facilities, and at varying levels; reducing demand for services; and sustaining critical resources. While successful in mitigating impacts of the unanticipated three-virus surge, considerable co-ordination resources were used to develop, execute, and sustain system response. With such respiratory surges of RSV, influenza, and COVID-19 expected to continue and overlap in the future, exacerbating existing societal health care inequities, greater attention is needed to strengthen the robustness of health care infrastructure, resources, and preparedness measures in a manner that addresses all three threats effectively, with a focus on strengthening systems caring for historically marginalized populations.







