BACKGROUND
The primary pathogens of soft tissue infections, including those of the foot, are beta-haemolytic Streptococci and Staphylococcus aureus.1 However, Pseudomonas aeruginosa has been implicated as a cause of foot infections in patients after they have sustained a nail puncture wound through a sneaker, historically leading to recommendations for prescribing empiric antipseudomonal antibiotics.2,3 At Olive View-UCLA Medical Center, Sylmar, California, the authors evaluated empiric antibiotic prescribing behaviour and microbiology of foot puncture wound infections.
METHODS
A retrospective chart review was conducted on adults (aged ≥18 years) admitted with an ICD-10 code for puncture wounds from January 1 2017–December 31 2023. Inclusion criteria included foot infection after sustaining nail, screw, staple, thumbtack, or razorblade puncture. Non-foot puncture wounds and punctures from an object other than those listed in the inclusion criteria were excluded. Antipseudomonal antibiotic was defined as either piperacillin-tazobactam, cefepime, ceftazidime, or ciprofloxacin.
RESULTS
Fifty-eight cases were reviewed, and 45 met the inclusion criteria. The majority of puncture wounds were due to nails (n=34; 76%), followed by screws (n=6; 13%). Puncture occurred through the shoe in 38/45 cases (84%), barefoot in 2/45 (5%), and not described in 5/45 (11%). An empiric antipseudomonal antibiotic was prescribed in the emergency department in 41/45 cases (91%), whereas an empiric antipseudomonal antibiotic was prescribed or continued upon admission in 19/45 (42%). The average days of therapy on antipseudomonal antibiotics was 2 days (interquartile range: 2–3 days). Wound culture was obtained in 44 cases, with no isolation of P. aeruginosa. The majority of identified pathogens consisted of methicillin-susceptible S. aureus (n=26; 59%) and Streptococcus agalactiae (n=19; 43%); infection involving both S. aureus and Streptococcus spp. was seen in 15 cases (34%; Figure 1). Subsequent foot infection with P. aeruginosa within 30 days of puncture wound infection did not occur in any cases.
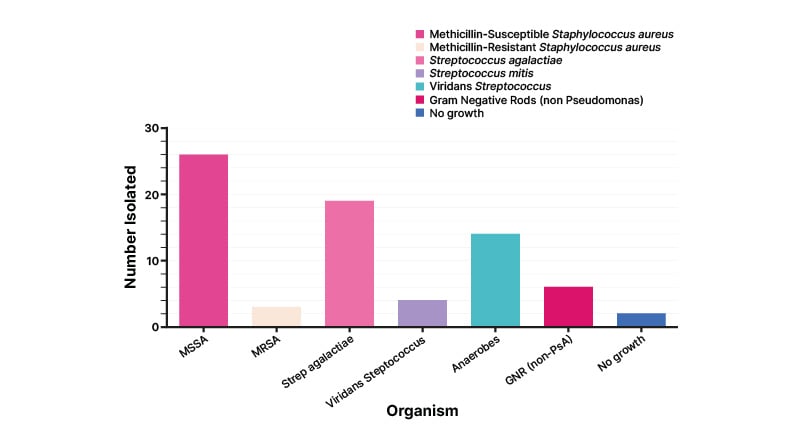
Figure 1: Organisms isolated in wound culture.
MSSA: methicillin-susceptible S. aureus; MRSA: methicillin-resistant S. aureus; GNR: Gram-negative rods; non-PsA: non-Pseudomonas.
CONCLUSION
P. aeruginosa was not isolated in any cases of foot puncture wound infection, including puncture occurring through a shoe, documented in 84% of the authors’ cases, the majority of which had diabetes (95.5%). Given the historical perception of the role that P. aeruginosa plays in this infection, the majority of cases were started on an empiric antipseudomonal antibiotic. This finding provides insight into antibiotic prescribing behaviour for foot puncture infection, whether the puncture occurred through a shoe or not. The primary pathogens consisted of S. aureus and/or Streptococcus spp., especially S. agalactiae, a virulent pathogen in individuals with diabetes. Foot puncture wound infections present an opportunity for antimicrobial stewardship to prioritise empiric, narrower antibiotic treatment selection against S. aureus and Streptococcus spp., and not against P. aeruginosa, as is commonly practised.







