Abstract
Intussusception as the initial presentation of coeliac disease has been rarely reported, with an incidence of 1% in all coeliac disease presentations. Furthermore, intussusception requiring surgical reduction as the primary presentation for coeliac disease in adults is even rarer. Presented here is a case of a 37-year-old female Asian patient who presented with abdominal pain and distension; she was diagnosed with small bowel obstruction due to jejunojejunal intussusception and required surgical reduction as the initial presentation of coeliac disease.
INTRODUCTION
Coeliac disease is a disorder of the small intestine, which is characterised by mucosal inflammation, villous atrophy, and crypt hyperplasia, and occurs upon exposure to dietary gluten; the disease eventually shows improvement after cessation of gluten in the diet. Adult coeliac disease is now considered to have a prevalence of 0.5–1.0%.1,2 A classic presentation in patients with coeliac disease is diarrhoea with stool that is floating, bulky, and foul-smelling due to steatorrhoea. Historically, intussusception in association with adult coeliac disease is considered to be transient and asymptomatic.3 Willingham et al.4 were the first to suggest that intussusception in adults with coeliac disease may result in symptoms. Intussusception is defined as the invagination or telescoping of a part of the intestine into itself. Intussusception is unusual in adults (approximately 5% of all cases) and is thought to be due to structural lesions in more than 80–90% of cases, a retrospective series of surgical cases reports.5,6 In the majority of adult cases, a pathologic cause is identified.7 Conversely, reviews analysing radiologically diagnosed intussusception reported that only 30% of patients had an identifiable lead point, while >50% were without one and were therefore considered to have idiopathic or non-lead intussusception.8,9 Furthermore, the location of adult intussusception in surgical literature6,10 and radiologic series5,9,11,12 was found to be enteroenteric or ileocolic, with the majority of non-neoplastic cases being enteroenteric intussusception. Moreover, non-lead intussusceptions are mostly inflammatory in nature: pancreatitis, cholecystitis, appendicitis, Crohn’s disease, cystic fibrosis, adhesions, scleroderma, and coeliac disease.5 In the medical literature, a well-established relationship has been made between transient intussusception and known coeliac disease; however, intussusception requiring surgical reduction appearing as the primary presentation for coeliac disease in adults is a rare entity.
CASE REPORT
Initial Presentation
A 37-year-old female Asian patient, with no previous medical or surgical history, presented with acute onset of diffuse abdominal pain associated with nausea, two episodes of vomiting, and increased abdominal girth for the past day, and the inability to pass any flatus for the past 12 hours. The patient denied fever, chills, change in bowel habits, history of diarrhoea, and weight loss, nor any previous episodes of similar complaints. On physical examination, the patient had tachycardia, with a pulse rate of 117 beats per minute, and her blood pressure was haemodynamically stable at 120/80 mm Hg. On abdominal examination there was abdominal distension, very faint bowel sounds, tenderness on deep palpation, and no rebound tenderness.
Laboratory Findings
Laboratory work-up showed leukocytosis, with a white blood cell count of 15,000 cells/mm3 and neutrophil shift with 80% neutrophils, and elevated inflammatory markers, with normal electrolytes, creatinine, amylase, and lactate dehydrogenase.
Imaging
Consequently, an abdominal and pelvic CT scan with intravenous contrast was performed, which showed jejunojejunal intussusception 6 cm in length with wall thickening (Figure 1); no lead point could be identified nor any signs of compromise in blood supply, and there was minimal free intraperitoneal fluid. Therefore, a nasogastric tube with a low pressure Gomcoâ suction machine (Allied, St Louis, Missouri, USA) was inserted. Due to the aforementioned, the patient was scheduled for diagnostic laparoscopy.
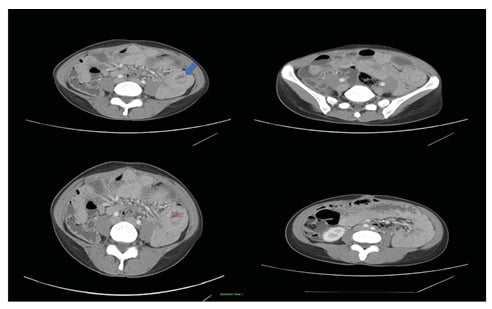
Figure 1: Abdominal and pelvic CT scan with intravenous contrast.
Target sign (blue arrow), extending 6 cm, suggests intussusception between ileo-ileal loops. There is prominent wall thickening of the intussuscepted bowel, measuring 11 mm in thickness with surrounding fat streaking.
Surgery
In the operating theatre, the patient was given general anaesthesia, positioned in the modified lithotomy position with both hands adducted, and a urinary Foley catheter was inserted. A 10 mm trocar was inserted into the infraumbilical area and two additional 5 mm trocars were inserted into the left side of the abdomen under direct vision. The ileocaecal valve was identified and small bowel inspection was performed, starting at the ileocaecal valve until the ligament of Treitz was reached. The intussusception was identified (Figure 2A), which was reduced with no signs of ischaemia; however, the oedematous bowel wall was identified, with no tumourous growth detected.
Inpatient Stay and Further Analysis
The patient had a smooth in-hospital stay. Oral feeding resumed and flatulence passed on Day 1 post-surgery. The patient was discharged on Day 2 post-surgery. The patient also completed the necessary laboratory work-up (gastroscopy, colonoscopy, and possible capsule endoscopy) in order to identify the aetiology of intussusception. Further blood work-up showed increased levels of IgA and anti-transglutaminase, suggesting the diagnosis of coeliac disease. This was followed by a gastroscopy that showed scalloped duodenal mucosa, which too suggested the identification of coeliac disease. Duodenal biopsy showed mild to moderate villous atrophy (Figure 2B), increased intraepithelial leukocytosis (Figure 2C), and positive CD3 staining (Figure 2D). This led to the diagnosis of adult coeliac disease, with primary presentation of jejunojejunal intussusception requiring surgical reduction as the first manifestation.
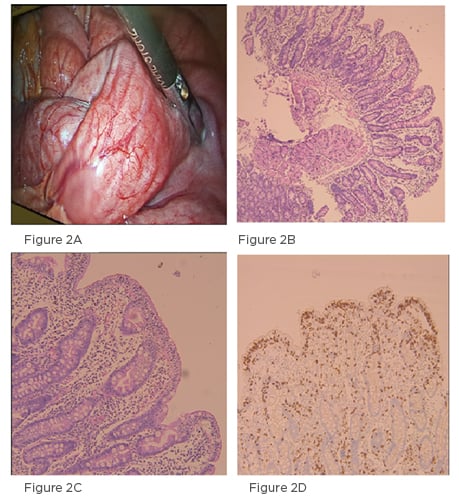
Figure 2: Intraoperative findings and histologic appearance.
A) Intra-operative picture of the intussuscepted bowel loop, with no signs of ischaemia or necrosis noted; B) section of duodenum showing mild to moderate villous atrophy; C) increased intraepithelial lymphocytosis; D) CD3 immunohistochemistry stain confirming the increase in intraepithelial lymphocytes.
Long-Term Follow-Up
The patient was started on a gluten-free diet. There was one reported episode of abdominal pain with transient intussusception, which was likely caused by non-adherence to the advised diet, 6 months post-diagnosis. Following this, the patient lived 1-year symptom-free with strict adherence to a gluten-free diet.
DISCUSSION
Coeliac disease is a chronic, inflammatory disease of the small intestine, with an incidence in the general population of 1–2%.13,14 If undiagnosed and thereby untreated, the inflammation can lead to bowel wall oedema,15 intestinal lymph node swelling,16 dysmotility in the small intestine,16 ulcers, and strictures in the small intestine,17 all of which are predisposing factors for intussusception; therefore, patients with undiagnosed coeliac disease may present with intussusception. However, intussusception as the initial presentation leading to the diagnosis of coeliac disease has been rarely reported in the medical literature. Adult intussusception is a rare entity (5% of all cases) and is much more common in children,18 being the most common cause of bowel obstruction (whereas it is responsible for only approximately 1% of adult cases).10,19 Three main aetiologies have been identified: idiopathic, benign, and malignant.20 Among the widely available imaging modalities, CT scanning is a sensitive test for diagnosing adult intussusception.10,18,20 Furthermore, CT can further identify a lead point, the size of intussusception, detect vascular compromise, and predict the likelihood of self-resolution.12,21 Although less sensitive than CT, ultrasound sonography has the ability to detect the pathognomonic target sign in some cases.18 As a result, the more frequent use of cross-sectional imaging modalities in recent years has increased recognition of intussusceptions in adults.22 With regards to the site of intussusception, enteroenteric intussusceptions account for the majority of cases in adults, although gastroenteric, ileocolic, and colocolonic intussusceptions can also occur.11 A wide spectrum of symptoms are associated with adult presenting intussusception: non-specific abdominal pain, nausea, vomiting, change in bowel habits, abdominal distension, haematochezia, and surgical abdomen when venous blood flow is compromised followed by arterial compromise, making the diagnosis a challenge. However, intussusception as the initial manifestation of coeliac disease in adults is rare, and even rarer is intussusception requiring surgical reduction as the primary presentation. Only nine cases in the medical literature have reported intussusception as the initial presentation for coeliac disease (Table 1).
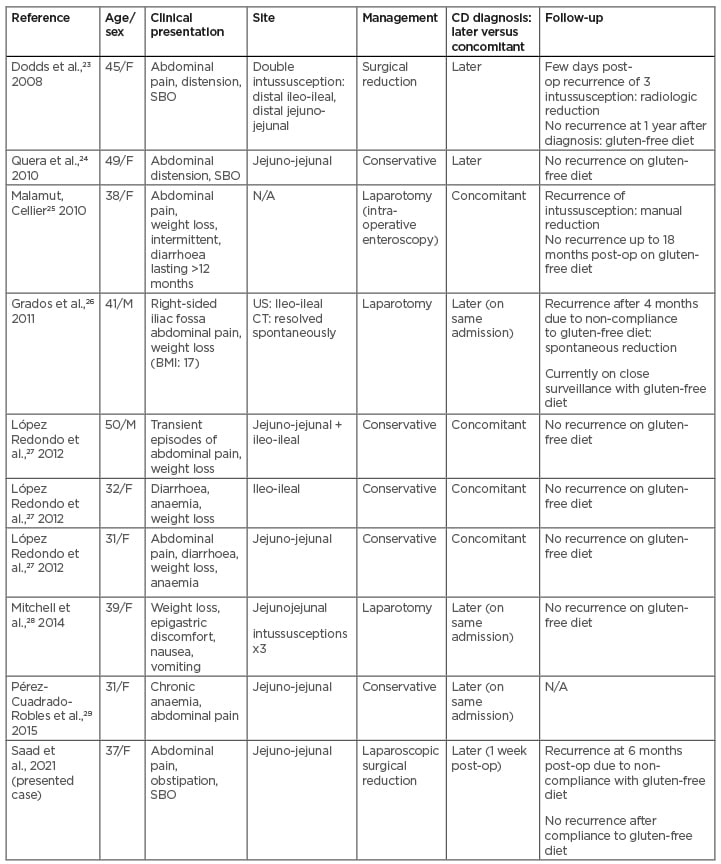
Table 1: Previously reported cases of coeliac disease with intussusception as the initial presentation.
CD: coeliac disease; F: female; M: male; N/A: not available; post-op: post-operatively; SBO: small bowel obstruction; US: ultrasound.
On the other hand, Warshauer et al.11 suggested that transient intussusception of the small intestine be advocated as the sole finding in coeliac disease diagnosis, most likely due to intestinal motility disorders. Historically, surgical treatment was argued to be universally appropriate for adult intussusceptions; however, recent literature suggests that a more selective approach is warranted, whereby intussusception usually remits spontaneously in the majority of cases and surgery is deemed necessary only in a small subset of patients. Indeed, Lvoff et al.,20 in an analysis of 37 cases of adult intussusception identified by CT, found a significant difference between the length of the intussusception between surgically and conservatively managed cases, with a length of <3.5 cm likely to be self-limiting. In general, recent studies favour a conservative approach to cases of adult intussusception, where the probability of malignancy, lead point, and ischaemia are low and the likelihood of spontaneous resolution is high. However, in patients presenting with recurrent intussusceptions, a diagnosis of inflammatory bowel disease or coeliac disease must be ruled out. Nonetheless, coeliac disease must be taken into consideration in cases of unexplained intussusception in adult patients, allowing for early diagnosis and hence early treatment to decrease the morbidity and mortality associated with delayed diagnosis.
CONCLUSION
Intussusception as initial manifestation of coeliac disease in adults is rare. Even rarer is intussusception requiring surgical reduction as the primary presentation for coeliac disease. CT and barium studies are the gold standard for diagnosis of intussusception. Coeliac disease must be taken into account in cases of unexplained intussusception in adult patients. Compliance with a strict gluten-free diet is greatly important as this will decrease the rate of emergency admissions and consequently hospital admissions.
Written informed consent was obtained from the patient to publish the case, as well as any associated images.








