Abstract
Optimal treatment of bifurcation lesions is still a major challenge for coronary intervention. A planned two-stent approach may be more appropriate when both the parent vessel and side branch (SB) are large, and when there is significant disease distal to the ostium of a SB that arises from the main vessel at a shallow angle.
A simple, provisional stenting approach that is associated with shorter fluoroscopy time, lower incidence of periprocedural myocardial infarction, and similar rates of target-vessel revascularisation compared with a routine two-stent strategy is needed. The combination of a biovascular scaffold and drug-eluting stent implantation as a two-stent technique using a ‘mini-crush’ technique is a safe, feasible, effective, and durable treatment option for patients with true bifurcation disease. Patient selection for complex stenting requires accurate lesion evaluation. Our current institutional recommendations are to use provisional stenting in the majority of cases, but if a planned two-stent approach is required, we recommend the use of imaging methods, plaque modification before stent implantation, final kissing balloon, and proximal optimisation inflation technique to achieve good final results.
INTRODUCTION
Optimal treatment of bifurcation lesions is still a major challenge for coronary intervention. Important factors such as anatomic variation, angulation between branches, downstream territory, and extent of plaque burden should be taken into consideration when addressing a bifurcation lesion, to choose the most appropriate approach and achieve the optimal result. A planned two-stent approach might be more appropriate when both the parent vessel and side branch (SB) are large. This mainly occurs when there is significant disease distal to the ostium of a SB, that arises from the main vessel, at a shallow angle.
Nevertheless, there is still a need to try simple, provisional stenting approaches that are associated with shorter fluoroscopy time, lower incidence of periprocedural myocardial infarction, and similar rates of target-vessel revascularisation compared with a routine two-stent strategy.1 A meta-analysis of previous randomised studies demonstrated that a provisional one-stent approach was comparable to a two-stent approach in terms of mortality, repeat revascularisation, and quality of life.2 The one-stent technique was superior to the two- stent technique in terms of risk of periprocedural myocardial infarction, however the two-stent technique is still a viable option in patients with complex true bifurcation lesions.3 In randomised studies comparing one-stent techniques with two-stent techniques, the two-stent approach was used in between 4% and 31% of all cases.1
Before making a decision on whether to treat a bifurcation lesion with two-stent strategies several questions must be answered:
- How large is the SB? (Diameter, vessel length, and myocardial territory supplied)
- Is the SB ostium diseased? If yes, what is the severity and length of the lesion?
- Is there severe disease in the SB beyond the ostium?
- What is the angle of the SB take-off? Is it difficult to wire/rewire?
- What is the severity and distribution of the main branch (MB) lesion?
- What will happen to the SB after MB stenting (mild or significant compromise or occlusion)?
- What are the clinical consequences of SB occlusion? (dependent on the territory supplied)4
The European Bifurcation Club (EBC) consensus from the first 10 years of meetings regarding planned two-stent strategy recommends that the main vessel should be stented first in most cases. However, when the SB is particularly difficult to access, there is dissection after pre-dilatation in the SB, or downstream stenosis is stented, then the SB can be considered for stenting first. For the two-stent method, final kissing balloon (FKB) dilatation is mandatory, as well as using moderate pressure.5 Drug-eluting stents are recommended for bifurcation treatment. The main vessel stent should be sized according to the distal main vessel reference diameter and should achieve adequate stent apposition in the proximal main vessel by the proximal optimisation technique (POT).6 The bifurcation treatment technique classification, proposed by the EBC, was based on two principles: the final position of the stent(s) in the bifurcation and the implantation order. There are four strategies designated by the MADS (main, across, distal, side) classification system. ‘M’ begins with a stent in the proximal main segment. ‘A’ begins with a stent in the main vessel across the SB. ‘D’ defines a double stent implantation, whether simultaneous or not. In an aborted form, a stent and a balloon are at the ostium of the two distal branches, with a slight protrusion (V-stenting), or a long new carina. ‘S’ consists of a stent implantation beginning in the SB, with or without protrusion (short or long). After implantation of the first stent(s), further stents can be implanted using different techniques. No wire or balloon manoeuvres are described in MADS, such as SB protection by wire or balloon, or different ways to crush an SB stent (kissing, balloon crush, double kissing [DK] crush, etc.).7 A variety of two-stent techniques can be performed and because of a lack of studies on the comparative outcomes of diverse two-stent techniques, selection of bifurcation treatment approach should be based on a patient’s clinical condition, bifurcation morphology, the operator skills, and preferred choice.
From dedicated two-stent techniques we know that:
- T stenting techniques can be performed in many variations (modified T stenting, reverse T stenting, and T stenting and protrusion). The technique is appropriate for bifurcations near to 90°
- The culotte technique regained popularity in the drug-eluting stent (DES) era. The EBC recommends a ‘mini-culotte’ to reduce the proximity of a double layer of stent struts as much as possible. This technique could be used in almost all bifurcation lesions
- The main advantage of the crush technique is that the patency of both branches is ensured during procedure. This can be used in almost all bifurcation lesions. There are some modifications of the crush technique (‘mini-crush’ technique, step-crush technique, reverse-crush technique, DK crush technique). Rates of successful kissing balloon inflation in crush stenting are 75–90%, which is lower than for culotte stenting. In cases of technique change during procedure it is impossible to crossover from provisional stenting to crush stenting8
- Either the V-stenting or simultaneous kissing stenting technique can be used for bifurcations in the large proximal main vessel. These are not frequently used due to relatively unfavourable angiographic and clinical outcomes and are not recommended as a routine two-stent technique9
PATIENT CASE EXAMPLE
Our case report using the two-stent bifurcation treatment approach was based on our single-centre design to treat bifurcation lesions with a ‘keep it simple, swift, and safe’ (KISSS) principle. Where possible we look to incorporate a bioresorbable vascular scaffold (BVS) into our two-stent technique as subsequently this will be absorbed leaving just one stent in situ.
The patient was a 65-year-old man with persisting Grade II–III stable angina for a period of 6 months. His past medical history includes hypertension, active smoking, peripheral vascular disease with claudication, and well controlled dyslipidaemia. Angiographic images demonstrated a critical true bifurcation lesion in the left circumflex (LCX) artery and first obtuse marginal (OM1) branch. LCX was the MB and OM1 was the SB. Medina classification was 1,1,1; this was confirmed by intravascular ultrasound (IVUS) (Figure 1). After careful lesion analysis using IVUS and optical coherence tomography (OCT) data for both branches, the bifurcation type was clear and it was possible to plan a treatment strategy according to the patient’s vessel plaque morphology. In this case OM1 was suitable for stenting as the disease extended from the SB ostium >5 mm. We decided to treat this bifurcation lesion with the mini-crush two-stent technique using the newest generation DES in the MB (LCX), and a BVS in the SB (OM1).
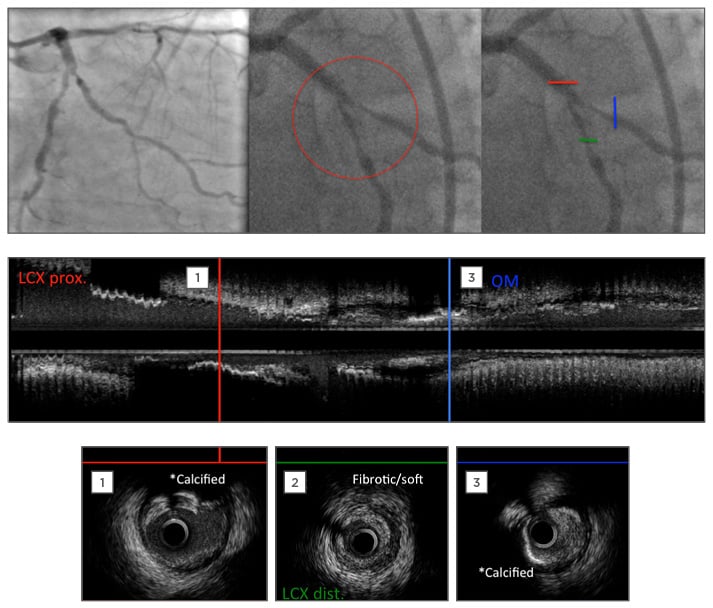
Figure 1: Pre-percutaneous coronary intervention angiographic images and intravascular ultrasound (IVUS) pullback.
Angiographic images show a diffuse coronary artery sclerosis with severe bifurcation stenosis in LCX/OM1. IVUS pullback confirmed a calcified plaque in proximal LCX (MB) and fibrotic/soft plaque in distal part. Proximal LCX mean lumen area is 4.98 mm2. Distal LCX lumen area is 2.68 mm2. OM1 branch (SB) is calcified too with lumen area 2.47 mm2. SB ostial disease extended >5 mm length.
LCX: left circumflex artery; OM1: first obtuse marginal branch; MB: main branch; SB: side branch.
Using the 7 Fr Launcher® coronary guide catheter (Medtronic, Minneapolis, MN), both branches were wired with soft-tip wires. IVUS and OCT pre-percutaneous coronary intervention images confirmed that mixed plaque was present, along with the presence of heavy calcification. We began with thorough lesion preparation because the treatment would involve a novel technique, using IVUS-guided cutting balloon plaque modification in both branches. The next step after pretreatment was BVS implantation in the SB (OM1), following DES implantation in the MB (LCX) using a mini-crush technique, and ending with kissing and POT. The percutaneous coronary intervention result was evaluated using IVUS and OCT.
Mini-Crush Stenting
First it is important that the lesion and affected vessels are suitable for this technique. Angulation between the vessels should be <60° and the diameter of the two branches should be similar. The guiding catheter should be suitable for the insertion of two stents. From the beginning, both branches need to be wired and pre-dilated if required. Pre-dilatation of the SB origin before MB stenting has the potential to maintain SB thrombolysis in myocardial infarction flow and access to the SB after MB stenting. After this, both stents need to be advanced. The MB stent should be positioned proximally and the SB stent should protrude only minimally into MB. The SB stent can then be deployed, following which, the result of the stent implantation should be checked. If optimal, the stent system balloon and the wire from SB can be removed; the MB stent can then be deployed, crushing the SB stent. After this you will need to rewire branches and conduct a high pressure post-dilatation in the SB and finally, a kissing dilatation for both branches. DK crush modification may aid rewiring of the SB after MB stenting.5
The standard crush and mini-crush techniques require use of a 7 or 8 Fr guiding catheter. Operators who prefer smaller diameter guiding catheters can choose modified crush techniques:
- Step-crush: This is suitable for use with a 6 Fr guiding catheter and can be modified by the balloon crush technique. The result of this technique is identical to that obtained with the standard crush technique, except that each stent is advanced and deployed separately10
- Reverse or internal crush: This is an option in the setting of provisional SB stenting and can be performed through a 6 Fr guide catheter, however this technique shares the same disadvantages as the standard crush technique but with more technical steps11
- DK crush technique: This is a modification of the step-crush procedure in which a balloon kissing inflation is performed twice, the first after a MB balloon crushes the SB stent, followed by the standard final kissing inflation at the end of the procedure. The DK crush technique therefore consists of five steps: SB stenting, balloon crush, first kissing, MB stenting and crushing, and final kissing. DK crush may result in less stent distortion, improved stent apposition, and facilitate final kissing inflation12
In our patient’s case Figure 2 demonstrates the procedural steps of bifurcation angioplasty. The final result of bifurcation treatment in the mini-crush approach is seen in Figure 3, where OCT images show excellent SB ostial coverage and neocarina formation. Figure 4 demonstrates the 1-year angiographic follow-up without signs of angiographic stent restenosis.
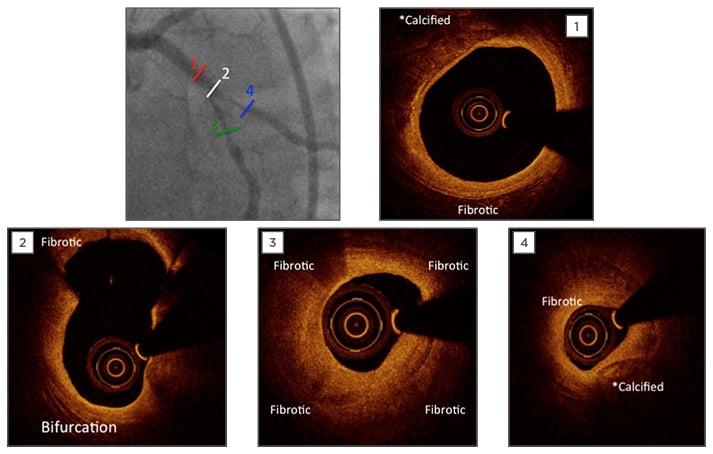
Figure 2: Pre-percutaneous coronary artery optimal coherence tomography imaging.
OCT confirmed calcified and fibrotic plaque composition in MB (1,2,3) and SB (4).
OCT: optimal coherence tomography; MB: main branch; SB: side branch.
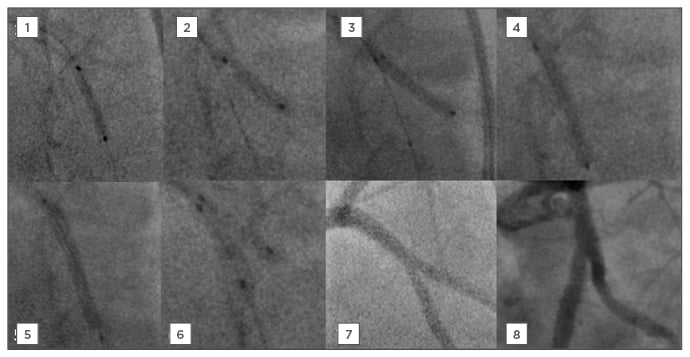
Figure 3: Percutaneous coronary intervention steps for elective mini-crush stenting with a drug-eluting stent and bioresorbable vascular scaffold.
1) LCX (MB) plaque modification with cutting balloon (3.25×15 mm, 4,5,6 bar).
2) OM1 (SB) plaque modification with cutting balloon (3.0×10 mm, 4,5,6 bar).
3) BVS implantation in SB (Absorb 3.0×18 mm, 11 bar) following by NC balloon post-dilatation 3.25×15 mm.
4) SC balloon dilatation in MB mini-crush (3.0×15 mm, 18 bar).
5) DES implantation in MB (Synergy 3.5×28 mm, 7 bar), following NC balloon post-dilatation 3.5×15 mm.
6) Final kissing with 2 SC balloons (3.0×12 mm, 8 bar).
7) and 8) Final images after PCI.
LCX: left circumflex artery; MB: main branch; OM1: first obtuse marginal branch; SB: side branch; DES: drug-eluting stent; NC: non-compliant; SC: semi-compliant; PCI: percutaneous coronary intervention.
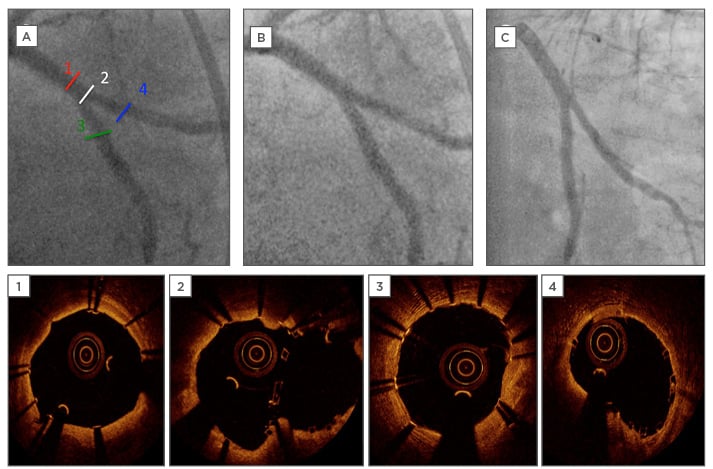
Figure 4: Final angiographic images and optical coherence tomography after percutaneous coronary artery and 1-year follow-up angiography control.
OCT measurement for 1) proximal MB mean vessel diameter after stenting is 3.73 mm; 3) distal MB mean vessel diameter is 3.4 mm; 4) SB mean vessel diameter after stenting is 3.2 mm. Bifurcation OCT (image 2) confirm an excellent result at the neocarina of the bifurcation and full coverage of the SB ostium without scaffold disruption. Angiographic images post-PCI A) segments for OCT; B) final image for bifurcation; C) 1-year follow-up angiography control for bifurcation.
OCT: optical coherence tomography; MB: main branch; SB: side branch; PCI: percutaneous coronary intervention.
The feasibility of using the BVS in bifurcation lesions is still under investigation but so far, the results seem promising. BVS technology has some technical limitations to its use in bifurcation lesions, such as the risk of strut fracture.13 Dzavík and Colombo14 published bench testing in a synthetic arterial bifurcation model with T stenting, crush, and culotte procedures using a BVS. In crush cases, they could easily recross the crushed BVS with the wire and balloon and achieve good results after deployment of the main vessel BVS and FKB inflation. They concluded that in narrower angle bifurcations, a mini-step crush or culotte technique should be considered, deploying a metal DES in the SB. Although using the BVS in both MB and SB appears feasible, their use requires careful evaluation in fractal models with different bifurcation angles and clinically should be limited to patients with large-calibre main vessels. As disrupted BVS struts cannotbe visualised by angiography, they recommend intravascular imaging, preferably with OCT, or alternatively with IVUS (of the MB in particular), whenever dilation of the BVS struts, POT, or FKB inflation has been performed, or two BVS have been deployed, to ensure the integrity of the final result.
CONCLUSION
In conclusion, combined BVS and DES implantation as a two-stent approach using the mini-crush technique is a safe, feasible, effective, and durable treatment option for patients with true bifurcation disease. Patient selection for complex stenting requires accurate lesion evaluation including assessment of distribution of disease (whether the disease involves both branches), size of branch, angle of branch, severity and length of the SB lesion, and presence of concomitant distal disease in the SB. Double stenting is more complex, time-consuming, and labour intensive, and requires specialist techniques, including IVUS/OCT guidance, plaque pretreatment, new-generation DES and BVS usage; post-stenting optimisation is strongly recommended to avoid complications and ensure favourable long-term results. OCT is the best visualisation method for implanted BVS evaluation. Further investigation is needed to prove the long-term results. Our current recommendations are still to use provisional stenting in the majority of cases, but if there is a need to do a planned two-stent approach, we recommend the use of imaging methods, plaque modification before stent implantation, and FKB and POT inflation to achieve an effective final result. FKB inflation should be done with appropriately sized balloons during all two-stent techniques to achieve less proximal stent deformation. Additionally, the DK crush may be superior to the standard crush technique with respect to acute procedural results and clinical outcomes by facilitating successful final kissing inflation in all patients.
Our institution is conducting an ongoing pilot, prospective, consecutive, single-centre registry for unprotected left main intervention by IVUS-guided and OCT-optimised combined BVS (LCX) and DES (left main anterior descending coronary artery) stent implantation using either a two-stent, mini-crush, or T-stent strategy. At this time the registry has included >50 patients. Thirty-eight patients reached the 1-year follow-up whilst 16 patients so far have reached the 2-year follow-up. Data from these patients show good results for this bifurcation treatment strategy.








