There is considerable variability in the selection of comatose survivors of out-of-hospital cardiac arrest (OHCA) for immediate coronary angiography. The post-resuscitation electrocardiogram (ECG) is used by some individuals and institutions as a gatekeeper for selecting patients but it is unclear whether it accurately predicts myocardial ischaemia, particularly in the absence of ST-elevation. The aim of this study was to investigate the correlation between the post-resuscitation ECG and coronary angiographic findings in a large unselected cohort of comatose OHCA survivors.
We identified 192 comatose survivors of OHCA who underwent an immediate invasive coronary strategy at our institution between 1st October 2012 and 31st July 2015. Survivors were grouped according to their post-resuscitation ECG into four categories; 1) ST-elevation, 2) presumed new left bundle branch block (LBBB), 3) other ECG signs indicating myocardial ischaemia, and 4) no ischaemia. Coronary angiographic images were reviewed for evidence of an acute coronary occlusion (ACO), which was defined as acute total or subtotal (>95%) occlusion with Thrombolysis in Myocardial Infarction flow grade 0–2 or presence of thrombus.
The prevalence of coronary disease (angiographic stenosis >70% in at least one vessel) was 77% in our cohort. An ACO was found in 42%. Figure 1 shows the proportion of patients in each ECG group who were found to have an ACO. The majority of patients with ST-elevation (89%) had an ACO. However, an ACO was also present in 12% of patients with a non-ischaemic ECG and 26% of patients with an initial non-shockable rhythm. ST-elevation/LBBB identified patients with an ACO with 83% sensitivity and 80% specificity. Percutaneous coronary intervention (PCI) was attempted in 109 patients (57%) with a 96% success rate. A significant proportion of patients without ST-elevation had PCI (Figure 2), including 21% of patients with no ECG evidence of ischaemia. The overall survival to discharge rate was 58%, with 54% of patients achieving good neurological recovery (cerebral performance category 1 or 2).
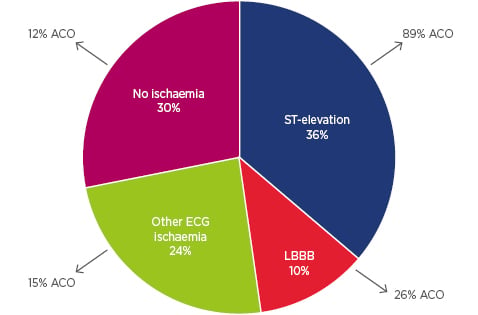
Figure 1: Proportion of out-of-hospital cardiac arrest survivors with an acute coronary occlusion by post-resuscitation electrocardiogram group.
ACO: acute coronary occlusion; ECG: electrocardiogram; LBBB: left bundle branch block.
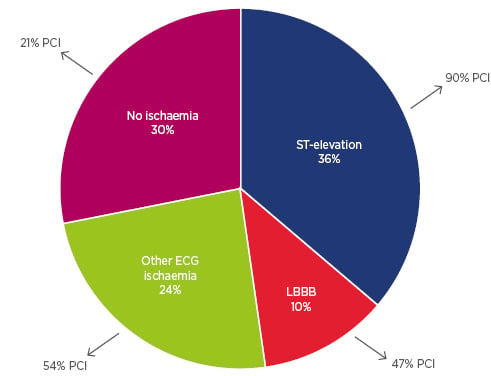
Figure 2: Proportion of out-of-hospital cardiac arrest survivors who had percutaneous coronary intervention by post resuscitation electrocardiogram group.
PCI: percutaneous coronary intervention; ECG: electrocardiogram; LBBB: left bundle branch block.
We conclude from this study that the post-resuscitation ECG does not accurately predict the presence of an ACO. Even in the absence of ECG ischaemia, comatose survivors of OHCA may benefit from emergent revascularisation. These findings are consistent with a recent Norwegian observational study1 and support the European consensus statement on invasive coronary treatment strategies for OHCA,2 which advocates early coronary angiography irrespective of ECG findings in the absence of an obvious non-coronary cause.
The discussion led by the chairperson focussed initially on the variability in OHCA care pathways adopted by different institutions. Despite differing practices, there was agreement that interventional cardiologists should become an essential part of the ‘chain of survival’ for patients with OHCA. The utility and timing of coronary angiography and PCI for all OHCA survivors was predictably debated. Although a growing body of evidence points towards a survival benefit,3,4some cardiologists remain unconvinced that an immediate invasive coronary strategy is beneficial or needed, particularly in the absence of ST-elevation on the post-resuscitation ECG. We hope that the randomised controlled trials currently recruiting (ARREST,5 PEARL,6 and DISCO7) will definitively determine the role of immediate coronary angiography in post-resuscitation care.








