Written by James Coker | Reporter, European Medical Journal | @EMJJamesCoker
![]()
On 4th December 2017, EMJ were present at Global Health Day 2017: “The UK Contribution to Innovation in Global Health”, to hear about vital innovative medical solutions being delivered by teams from the UK to address specific healthcare problems in developing countries. Among a set of highly engaging and impressive presentations, some recurring themes emerged. One regarded the way innovation in healthcare is defined; while it is often seen as referring to developments like high-tech equipment and mobiles applications, innovations were shown to encompass a much wider spectrum than this. The other is the vitally important role data play in providing the foundation for development programmes and other innovative concepts. In this article we describe a selection of the presentations made during this excellent event, which was held at the world-renowned Francis Crick Institute, London, UK. The day also included a poster exhibition, displaying a number of innovative research studies undertaken throughout the world.
Reducing HIV in adolescents and young adults in rural KwaZulu-Natal South Africa: A population health approach
Dr Maryam Shahmanesh, University College London, London, UK provided the first presentation of the day, in which she described a population health approach to tackling the issue of HIV in the Hlabisa area of northern KwaZulu-Natal of South Africa.1 She explained that being able to identify the causes of HIV and those individuals most at risk can be achieved through innovative methods, and is the foundation upon which innovative solutions have been, and will be, built. “Innovations in HIV prevention technologies far outstrip the innovations that we have in reaching the people that need it most,” she stated.
In this programme, the team run a longitudinal, population-based demographic surveillance of around 15,000 homesteads and 100,000 people for over a decade; this was designed to observe the effects of intervention strategies and identify which particular areas need to be targeted to reduce the number of HIV cases. Dr Shahmanesh explained that using these data, the health outcomes of the cohort of people living in this area could be observed through information like their electronic records, whether they are on treatment, and data collection in the clinics displaying the kinds of health services being reached. This showed, for example, that there was a very short window of opportunity to prevent HIV infection, with nearly 60% of women and around 40% of men infected with the virus by the third decade of their life. Identifying that education was strongly associated with HIV testing and contraceptive use provides an area to target for intervention strategies. Overall, the project has emphasised the importance of an interdisciplinary approach to addressing large-scale problems; the integration of social and basic science in this case led to the development and testing of new innovations in the population.
Using genome science to understand the current epidemic of invasive Salmonella disease in Africa
A new strain of Salmonella specific to Africa was the subject of a talk by Prof Jay Hinton, University of Liverpool, Liverpool, UK. The Salmonella Typhimurium ST313 strain kills hundreds of thousands of individuals each year in Africa and causes different symptoms than normally found in people who contract Salmonella-induced gastroenteritis in the developed world. The pathogen is resistant to antibiotics used to treat other strains of the bacteria.2 To understand what differentiates this pathogen, Prof Hinton and his team conducted a major genome comparison between Salmonella Typhimurium ST313 in Africa and strains that cause gastroenteritis in Europe. “If you start to compare genomes, you can start to ask more complicated questions about the relative incidence of different bacterial strains, you can start to track strains, and ask how outbreaks are happening,” he commented.
The comparison of hundreds of genomes showed the team straight away that there was something genetically different about the bacterium that had evolved in Africa to make it so dangerous; it wasn’t just that some of the human population was particularly susceptible. In particular, the analysis identified one single non-coding nucleotide, called PgtE, in the outer membrane of the bacteria, which promotes bacterial survival and dissemination (Figure 1). This study has enabled a key characteristic of a new and dangerous type of Salmonella to be recognised for the first time. The innovative multi-omic research approach could bring new insights to other important pathogens and help us prepare for future epidemics (Figure 2).
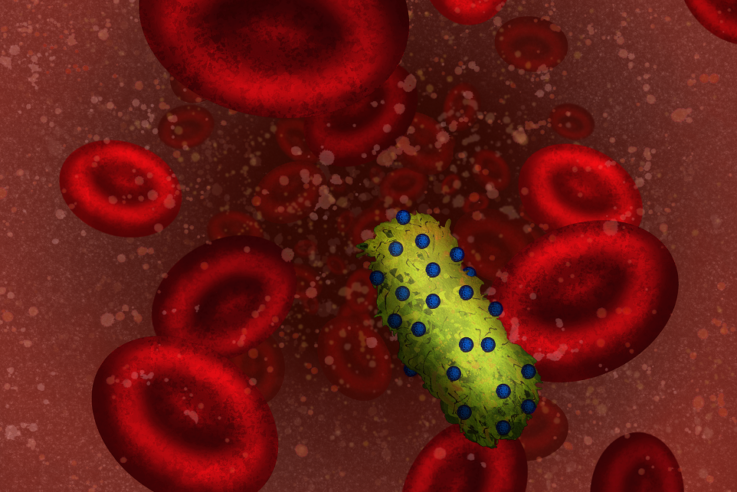
Figure 1: Illustration of African Salmonella expressing high levels of PgtE protein in the human bloodstream.
Eliza Wolfson 2018/CC/BY/NC/ND/4.0
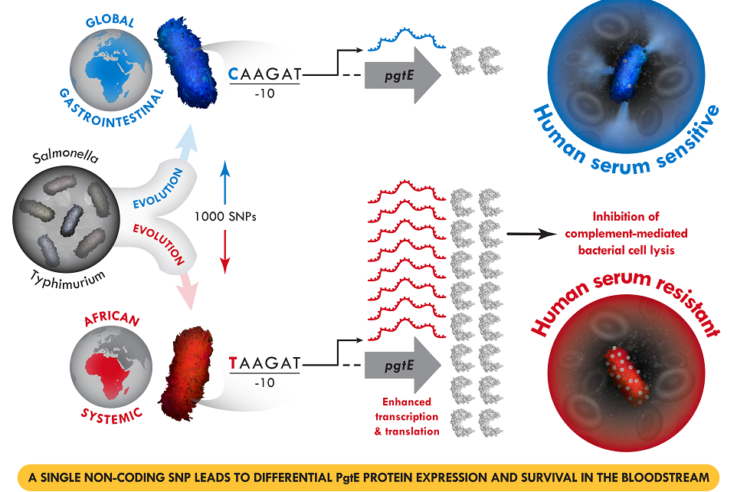
Figure 2: A single non-coding SNP leads to differential PgtE protein expression and survival in the bloodstream.
Eliza Wolfson 2018/CC/BY/NC/ND/4.0.
Peek: Evidence-based solutions for sustainable eye health: Using smartphones and behaviour change to create impact
In this part of proceedings, Dr Andrew Bastawrous, London School of Hygiene & Tropical Medicine, London, UK, informed the audience about the mission and set up of Peek, of which he is co-founder and CEO.3 This company utilises mobile phone technology to organise eye screening programmes in areas where there is a distinct lack of eye specialists and a large population with visual impairments that are mostly treatable. Beginning in Kenya, the programme was inspired by the fact that across Sub-Saharan Africa, despite there often being a lack of essential services, such as electricity and water, there is generally excellent mobile phone reception. Additionally, a large proportion of the population in this region own a phone.4
One of their innovations has been the creation of an application, called Peek Acuity,5 that enables an eye test to be given by unqualified individuals. This is crucial because in countries like Kenya, there is a lack of availability of eye specialists and services.3 A programme was therefore developed for use in schools, in which teachers could undertake eye tests of their pupils using mobile phones. This works by the examiner showing the child the letter ‘E’ displayed on the screen, which changes orientation and size according to the level of the child. They are asked to point in the direction the E is facing and the examiner then swipes the phone in that direction. If the child cannot see it at all, the examiner will shake the phone to record this outcome (Figures 3 and 4).

Figure 3: Trial of vision test in Nakuru.
Credit: @Peek Vision.

Figure 4: Teacher vision test.
Credit: @Peek Vision.
Following the test, a wealth of data are generated. This includes an automated referral message to the parents informing them of the results and providing them with the information necessary to make an informed decision. At the end of a day of eye tests, the headteacher also receives an aggregate message detailing the overall statistics. A dashboard provides programme managers with a live overview of the entire system, for example, the numbers of schools that have undertaken the test, the number of children tested, how many negative results there were, and the number of follow-up actions required. A visual simulation of what the visually impaired child can see, and what they would be able to see should they receive the correct treatment, can also be printed. Ultimately, the local hospital administrator receives a list of the children referred by their school and the date of referral. If the child does not attend, the relevant parties are informed.
Dr Bastawrous explained that the purpose of this was to identify what issues needed to be targeted; without this information, the problems are difficult to address. “What we’re trying to create here is not something that solves all the problems, but shows specifically where the problems are,” he commented.
The first RCT of the programme in Kenya showed outstanding results; in the space of 9 days, 900 children with visual impairments were identified by 25 teachers. Following further successful trials, the project has grown hugely, and recently the government of Botswana has agreed to completely fund a national programme for every school child in the country to be screened and treated by 2020.
The Brazilian 100 Million Cohort: Innovation in large-scale data collection and linkage
Dr Elizabeth Brickley, London School of Hygiene & Tropical Medicine, London, UK, explained her team’s use of large data resources to link information from >114 million individuals in Brazil with health and social outcomes following government programmes. CADASTRO-UNICO6 is a database of electronic records of applicants to social protection programmes in Brazil, which provides information on housing conditions, education, and income, organised by household. These data are linked to electronic health records, such as births, deaths, hospital episodes, and infectious disease notification. This follows a number of initiatives by the Brazilian state to alleviate inequality and poverty, and improve outcomes for citizens.
In addition to evaluating the impact of the social programmes on health outcomes, the team envisage the project as establishing research capacity with the aim of supporting further evidence-based policy-making. Dr Brickley went through the potential research avenues of the data analysis. Included among their goals is identify the social determinants of leprosy in Brazil to facilitate the early identification and treatment of cases. She also informed the audience about one research project that was carried out to observe the association between symptomatic dengue infection during pregnancy and the odds of stillbirth. The vast information enabled them to look at around 16 million eligible live births and 160,000 eligible stillbirths, discovering that the risk was doubled if there was a symptomatic dengue infection, and increased five-fold if there was severe dengue infection.
She concluded: “The legacy of this resource, which is now in its early days, is a cohort of 114 million anonymised subjects whose data are held in a secure research centre with a powerful public interface. Hopefully, in the future, this can mean that we see more and more policymakers engaging with scientists as they begin to design interventions and see them tested across this vast population, and that we can work together to improve health for future generations.”
Conclusion
These are just a sample of the fascinating and innovative approaches to solving healthcare issues in developing countries that were discussed during Global Health Day 2017. What was emphasised throughout was that innovation can encompass a whole variety of formats, and these approaches are often most effective when designed for context of specific locations. The use of large-scale data, including novel ways of collection and analysis, is a fundamental aspect of this.
References
- i-sense. Collaborating to develop technologies for HIV testing. 2017. Available at: https://www.i-sense.org.uk/news/collaborating-develop-technologies-hiv-testing. Last accessed: 2 February 2018.
- Hammarlöf DL et al. The role of a single non-coding nucleotide in the evolution of an epidemic African clade of Salmonella. 2017. Available at: https://www.biorxiv.org/content/early/2017/08/11/175265. Last accessed: 2 February 2018.
- Peek. Evidence-based solutions for sustainable eye health. Available at: https://www.peekvision.org/peek-solutions/. Last accessed: 2 February 2018.
- The Economist. In much of sub-Saharan Africa, mobile phones are more common than access to electricity. 2017. Available at: https://www.economist.com/blogs/graphicdetail/2017/11/daily-chart-5. Last accessed: 2 February 2018.
- Peek. Peek Acuity. Available at: https://www.peekvision.org/peek-acuity/. Last accessed: 2 February 2018.
- Electronic Health Records Research Group. Brazilian 100 million cohort. 2017. Available at: http://ehr.lshtm.ac.uk/news/brazilian-100-million-cohort/. Last accessed: 2 February 2018.








