Abstract
In recent years, E-learning, also known as web-based learning, online learning, computer-assisted instruction, or internet-based learning, has been used frequently in healthcare education programmes. E-Learning has played a significant role in the author’s cytotechnology programme by providing online distance education to multiple sites nationally, and soon internationally.
Although many papers currently exist regarding E-learning, the literature lacks review papers on E-learning in pathology education. The objectives of this paper, therefore, are to provide a narrative review of the approaches used in incorporating E-learning in pathology education, and to provide a faculty member’s perspective of experiences, lessons learned in developing E-learning modules, and suggestions to future faculty developers of E-learning modules.
For the purpose of this review, PubMed and Google Scholar search engines were used to search articles published between the years 2008 and 2018. Any review articles and articles from proceedings were not selected for this review. The search resulted in 17 articles that met the criteria for further review. The reviewed literature showed that E-learning has been widely used in pathology education. There is, however, a lack of studies evaluating pre and post-test scores and the cost effectiveness of E-learning technologies.
INTRODUCTION
In recent years, E-learning, also known as web-based learning, online learning, computer-assisted instruction, or internet-based learning, has been used frequently to train healthcare practitioners, including those in nursing and radiology.1,2 E-Learning has played a significant role in the author’s cytotechnology (CT) programme by providing online distance education to multiple sites nationally, with plans for international implementation as well. This CT programme is a post-baccalaureate certificate programme with a 12-month curriculum that provides students with entry-level competencies as cytotechnologists. The class size ranges from 4 to 12 participants, and is currently the only programme in the nation that offers synchronous distance education, serving 4 satellite sites.
This CT programme has incorporated E-learning slowly and steadily for the past few years, with the significant step of incorporation of a virtual microscopy (VM) system. E-learning started with the building of a VM database of cytopathology digital images scanned using iScan Coreo Au scanner (Ventana, Arizona, USA) in mScope software (Aurora Interactive, Montreal, Quebec, Canada). Currently, the author has >3,000 digitised images that are used to create annotated teaching images, unannotated daily screening practice images, and screening test images. The digitised images are also used to create virtual scope session videos to mimic multihead microscope sessions. These videos are made available to the students on the course management system.
After it was determined that the students were able to learn cytomorphology using VM and apply their learning to screening glass slides with a microscope,3 the author aimed to reduce or eliminate the need for additional in-person training in the cytology laboratory by adding E-learning modules to the current online curriculum. With internal funding received from the author’s institution, the digitised images were used to develop E-learning modules. At this time, nine E-learning modules have been developed using Articulate 360 (Articulate Global, Inc., New York City, New York, USA) software. The E-learning modules include the title, specific objectives, video clips of the content, and interactive self-assessment questions with feedback. The perceptions of the CT students were assessed regarding the content of the E-learning modules and the perceived influence of the E-learning modules on their performance during clinical rotations. Students responded positively to the statements regarding the quality of the video and audio, duration, navigation, and the materials presented. Most of the students also responded positively, stating that the E-learning modules better prepared them for their role during clinical rotations and recommended developing more E-learning modules for cytology courses in the future.4 With the positive results received from the students, more E-learning modules are currently being developed. The programme, however, is yet to evaluate the objective outcomes of students’ learning influenced by E-learning modules. It is crucial to determine the role of E-learning modules in students’ education, which can be measured by comparing the pre and post-test scores. The author’s long-term goal is to statistically prove the effectiveness of E-learning modules in students’ education in this CT programme. The short duration as well as small class size of the programme, however, makes it difficult to statistically measure the objective outcomes.
Although many research papers have been published regarding E-learning in the training of healthcare professionals in sectors such as radiology, pharmacy, and nursing, the literature lacks review papers regarding the effectiveness of E-learning in specific healthcare professional educational training. As a faculty member who has had positive as well as challenging experiences in developing E-learning modules, the current paper was the result of the author’s own personal curiosity to know how other educational programmes have used E-learning for pathology education. The primary objective of this review was to identify the approaches to measure the objective outcomes of students’ learning influenced by E-learning modules in pathology education. The secondary objectives were to provide a narrative review of the approaches used to incorporate E-learning in pathology education, with a particular interest in describing the purpose of that incorporation, how E-learning has been incorporated, what types of outcome measures have been used to evaluate the effect of E-learning in pathology education, and a faculty member’s perspective of experiences and lessons learned in developing E-learning modules with suggestions for future development of E-learning modules.
METHODS
For the purpose of this review, PubMed and Google Scholar search engines were used to search articles published between the years 2008 and 2018. The keywords used to search the articles were “E-Learning”, “E-learning”, “eLearning”, “e-learning”, “Web-based”, “online”, and “pathology”. This search resulted in 26 articles. Seven articles, however, did not report E-learning in pathology education, one article was a proceeding, and another article was a review article and therefore all nine articles were excluded from the analysis for this study. The title or the abstract of the articles that contained at least one of the six keywords mentioned above and the words “pathology/pathologist”, “training”, and/or “education” were included for the analysis of this study.
RESULTS
The search resulted in 17 articles that met the criteria for further review for this paper.5-21 Review of the literature led to the arrangement of 3 categories: 1) purpose of incorporating E-learning in pathology education; 2) how E-learning has been incorporated; and 3) outcome measures that were used to evaluate the effects of E-learning in pathology education. The main information gathered from the 17 articles reviewed in this study are summarised in Table 1.
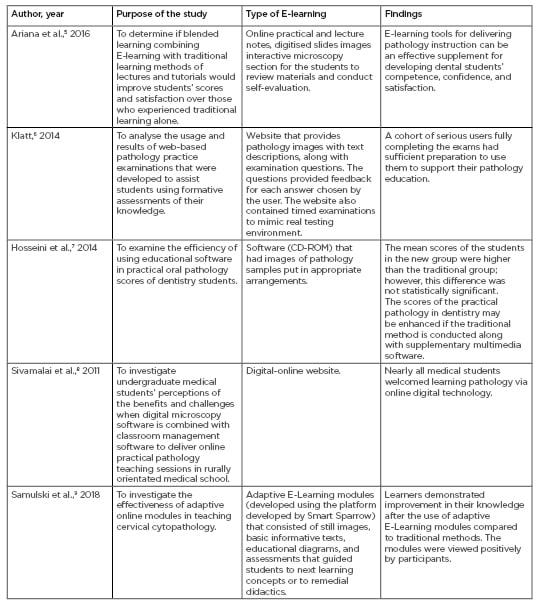
Table 1: A summary of the main information gathered from the 17 articles reviewed in this study.
ER: oestrogen receptor; HER2: human epidermal growth factor receptor 2; IHC4: immunohistochemical 4; MAPA: Microanatomy and Pathology Atlas; MCQ: multiple choice questions; PR: progesterone receptor.
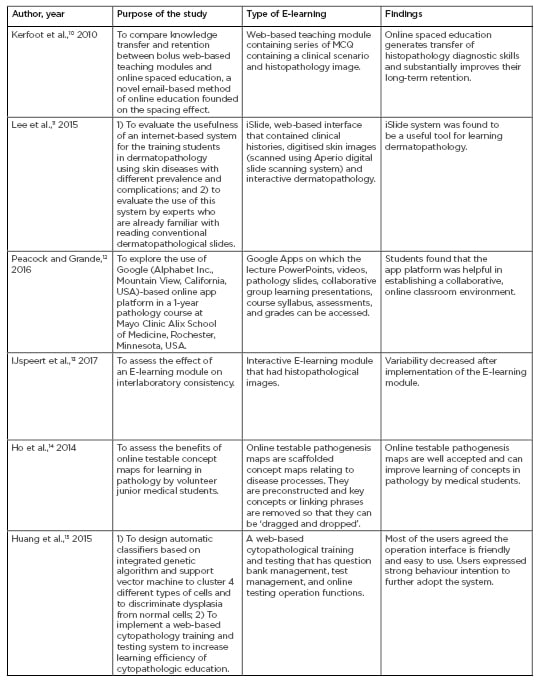
Table 1 continued: A summary of the main information gathered from the 17 articles reviewed in this study.
ER: oestrogen receptor; HER2: human epidermal growth factor receptor 2; IHC4: immunohistochemical 4; MAPA: Microanatomy and Pathology Atlas; MCQ: multiple choice questions; PR: progesterone receptor.
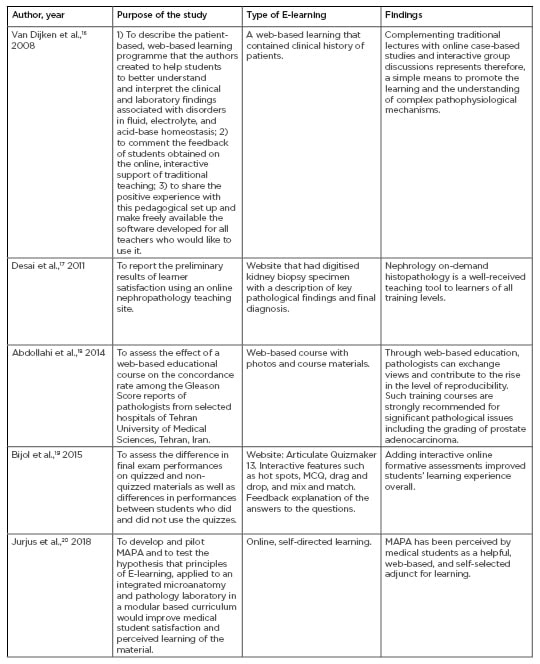
Table 1 continued: A summary of the main information gathered from the 17 articles reviewed in this study.
ER: oestrogen receptor; HER2: human epidermal growth factor receptor 2; IHC4: immunohistochemical 4; MAPA: Microanatomy and Pathology Atlas; MCQ: multiple choice questions; PR: progesterone receptor.
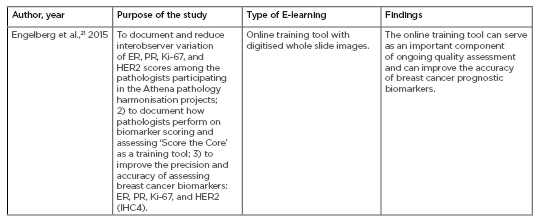
Table 1 continued: A summary of the main information gathered from the 17 articles reviewed in this study.
ER: oestrogen receptor; HER2: human epidermal growth factor receptor 2; IHC4: immunohistochemical 4; MAPA: Microanatomy and Pathology Atlas; MCQ: multiple choice questions; PR: progesterone receptor.
Purpose of Incorporating E-Learning in Pathology Education
Current evidence indicates that E-learning has been incorporated in pathology education in both classroom and clinical settings. In dental, medical, and resident classroom settings, E-learning has been used to determine the effectiveness of blended learning (combining E-learning with traditional learning methods) compared to traditional learning in histopathology education;5 examine the efficiency of using educational software in practical oral pathology scores;7 evaluate the usefulness of an internet-based system in learning dermatopathology;11 explore the use of Google (Alphabet Inc., Mountain View, California, USA)-based online app platform in teaching pathology course;12 evaluate both the qualitative and quantitative impact of online testable pathogenesis maps on learning pathology;14 explore the educational value of web-based formative assessment tool for renal pathology, and develop and pilot an Microanatomy and Pathology Atlas (MAPA) for medical students;20 investigate perceptions of digital microscopy software when combined with classroom management software to deliver online practical pathology teaching sessions;8 compare the knowledge transfer and retention between bolus web-based teaching modules and online spaced education;10 investigate the effectiveness of adaptive online modules in teaching cervical cytopathology;9 and collect students’ feedback on an online, interactive support of traditional teaching of pathophysiology.16
In clinical settings, E-learning has been used to assess the intra and interobserver concordance rates in the Gleason scoring of prostatic adenocarcinoma, before and after a web-based educational course among the pathologists;18 evaluate the performances of pathologists on using a web-based pathologist training tool;21 implement a web-based cytopathology training and testing system;15 and assess the interlaboratory consistency in the histopathological diagnosis.13 In addition, E-learning has been used to analyse the usage of web-based pathology practice examinations6 and gather learner satisfaction of web-based teaching modules in nephropathology education.17
Incorporation of E-Learning in Pathology Education
In the articles reviewed, E-learning has been incorporated as a) quizzes on the website, such as a series of multiple choice questions (MCQ) containing a clinical scenario and histopathology image;10 b) course materials with photos on websites;18 c) digitised images on websites and pathological findings and diagnosis;8,21,17 d) digitised images with text descriptions, clinical histories, and self-assessments with feedback on websites;11,6 e) course materials with online practical and lecture notes, and digitised slide images with interactive microscopy section for the students to review materials and self-evaluate on the website;5 f) CD-ROM with images of pathology samples put in appropriate arrangements;7 g) Google apps through which the lecture PowerPoints, videos, pathology slides, collaborative group learning presentations, course syllabus, assessments, and grades can be accessed;12 h) E-learning modules developed using special software that consist of images, informative texts, educational diagrams, assessments that guide students to the next learning concepts or to remedial didactics, interactive features such as hot spots, MCQ, drag and drop, mix and match, and feedback explanations of the answers to the questions; and finally,9,13,19 i) online testable pathogenesis maps that are scaffolded concept maps relating to disease processes.14
Outcome Measures
In the reviewed articles, the outcome measures that were used to evaluate the effects of E-learning in pathology education were retention skills, long-term learning efficiencies of online educational methodologies, resident performances on spaced education versus web-based teaching, student perceptions, pre versus post-scores, and only post-scores.5-21
In general, from the studies reviewed, students welcomed the addition of learning pathology via digital technology.8 They found the app platform helpful in establishing a collaborative, online classroom environment.12 They favoured online testable pathogenesis maps,14 supported further adoption of the online system because it was useful in cytopathology diagnosis and training,15 and they found that online quizzes improved learning experience.19 Very few studies that compared the pre and post-scores showed that post-scores improved after using E-learning tools.9,13,21 Studies that focussed on only the post-scores found that the scores of the students who used the E-learning tools were higher than the students who did not use the E-learning tools.5,7,14,19
The following common survey statement topics received positive responses in the reviewed articles: helpful annotations, easy access from anywhere, more convenient for learning, faster than using microscopes, allows self-paced learning, everyone sees the same image, better for group learning, better technology, feedback received was helpful in reinforcing concepts, module was effective in presenting the content and concepts, more engaging than the lecture and texts, online learning was a worthwhile adjunct to training, recommend to my classmates, collaborative capabilities to create joint-projects were helpful, enhanced learning, and improved understanding and identification of the differences between normal tissues and those with pathologies.8,9,11,14,20 Some difficulties participants indicated when using the online methods of learning included a lack of practice with a microscope, less interaction with the teacher while on rural placement, problems with the internet connection, technical problems with online technology, user needs of computer skills, among others.8 In the open comments, students also indicated that they found the interactive aspects of E-learning very interesting and engaging: it yielded more impact than just reading about a topic; it could be done at the student’s own pace and they could start and stop at will;9 it was easier to visualise; and was clearly organised and labelled.20 Students also suggested some improvements to future E-learning modules, such as user interface; more information; integration with other disciplines; more quiz features, pictures, tissue samples, and short explanations; consistency in the presentation of the material; comprehensive test features; and magnification features.14,20
DISCUSSION
The primary objective of this paper was to identify the approaches to measure the objective outcomes of students’ learning influenced by E-learning modules in pathology education.
Out of 17 articles reviewed, this study identified 2 articles that used pre versus post-scores to measure the participants’ performance in clinical settings, and 1 article in an educational setting.9 The study, which was conducted in an educational setting using a randomised, mixed methods, crossover design, reported improved post-test scores of the participants. Even though this method would be an ideal approach to measure the objective outcomes of the CT students, unlike this study which had a total of 36 participants, the present author’s CT programme has 4–12 students per year. Therefore, it is always a challenge to show statistically significant results with fewer student participants. A collaborative approach with other CT programmes to increase the sample size would help measure the students’ objective outcomes and achieve significance.
The secondary objectives of this study were to provide a narrative review of the approaches used in incorporating E-learning in pathology education and to provide a faculty member’s perspective of experiences and lessons learned in developing E-learning modules and suggestions for future faculty developers of E-learning modules.
Based on the reviewed articles, it is evident that E-learning has been incorporated and evaluated successfully in pathology for variety of purposes. Students’ perception surveys predominated as an outcome measure than the cost effectiveness of the E-learning modules or the test scores, particularly, the pre versus post-test scores.
Many of the articles reviewed used either digitised whole slide images or pathology images with quiz materials as E-learning tools. A limited number of studies used E-learning as a module that included lecture materials, videos, pathology images, and interactive features such as hot spots, MCQ, drag and drop, and mix and match, with feedback explanation of the answers to the questions. In the author’s experience in cytopathology education, students enjoyed and benefited from similar E-learning modules with videos that had voiceover descriptions and interactive self-assessment features.4 Additionally, the reviewed articles lacked detailed explanation in regard to the time and cost involved in developing the E-learning modules. In the author’s experience, time and cost are critical issues to consider for the faculty members in developing E-learning modules.
The anticipated faculty time commitment exceeded 50% when the author developed their first E-learning module (12 minutes 23 seconds in length) in their programme. This was primarily to learn the various E-learning technologies and software available and to choose those that best fit the objective. By the time the optimal option was chosen, affordable software that fit the objective of the module, and learned to develop the E-learning module, updated software programmes were already available to consider for the next E-learning modules. Therefore, faculty members need to be aware of the constant changes and updates in the technologies and the software and plan to spend considerable time to learn these technologies.
Updating educational material is a critical process in training healthcare professionals. A faculty member needs to be aware of the considerable amount of time spent in this process to make the most of the E-learning modules for education. From a faculty point of view, the author found updating E-learning modules initially challenging, particularly videos that contained digital images and voiceover audio descriptions. For example, when a description in an existing video portion of the E-learning module needed to be included, the whole video then had to be reshot, edited, inserted in the module, and republished to acquire the URL. This led to the rearrangement of the whole E-learning module.
A time-saving strategy identified through experience in developing E-learning modules was to involve the students. The author’s institution provided yearly funding opportunities for faculty-led E-learning projects, in which the students help the faculty members develop these modules. From this experience, working with students also helped the author to understand what they would like to see and how they would use the module. Their innovative ideas made the modules more creative and interactive. All of the E-learning modules were developed through internal funding mechanisms. As the process unfolded, unanticipated costs were identified. For the initial E-learning modules developed in the programme, the biggest expenditure was a professional videographer, voiceover recording, and editing of the videoclips. For the later modules, the author’s institution created an E-learning Lab that provided high quality video cameras in addition to a soundproof booth in which the audio recording could be done for the E-learning modules. This reduced expenses considerably.
A limitation of this study was the small number of articles reviewed. A more systematic approach on searching and selection of articles to review could have identified more information on using E-learning modules in pathology education.
In summary, the task of developing and evaluating E-learning modules may seem difficult; however, with proper planning and commitment it is achievable. As a faculty member who developed and evaluated E-learning modules in this CT programme, it gives the author great satisfaction and encouragement to observe students enjoy and benefit from these modules. Therefore, the author highly recommends that faculty members of other educational programmes who have never had the opportunity develop this valuable resource to enhance their training in their educational programme. One way to sustain the inclusion of E-learning in pathology is to collaborate with other educational programmes to develop E-learning modules so they can be shared among programmes. Through this, the time and manpower can be shared and the content of the modules can be standardised. Involving students, residents, or fellows in the development of E-learning modules with the faculty members to capture students and faculty members perspectives can also be considered to improve the quality of E-learning modules.
CONCLUSIONS
E-learning has been widely used in pathology education. There is still, however, a lack of studies that evaluate the cost effectiveness of the E-learning technologies, and pre and post-test scores of the participants.








