Abstract
Goal-orientated healthcare is multi-level strategic planning of medical care in which the patient’s goals are set first and, thereafter, their operationalisation is implemented into clinical practice. This is a novel approach to the management of patients with multiple morbidities. In this care model, the patients are treated as partners participating in a therapy process that is focussed on improving quality of life and health outcomes. This approach also facilitates the achievement of individually desired therapeutic targets by patients, their families, and/or their caregivers. The aim of this review is to present the concept of goal-orientated care based on current research from the medical literature and to describe some serious concerns related to the disease-centred model commonly used for patients with complex medical and/or mental conditions, such as the elderly. To illustrate the advantages and limitations of the goal-orientated patient care model, two exemplary cases of patients often seen in practice, such as primary care, cardiology, or geriatrics, are briefly described. The principles of goal-orientated patient care and available solutions to common problems should be useful to both the medical practitioners and their patients, in many contexts of multidisciplinary collaboration.
INTRODUCTION
A goal-directed healthcare system involves multi-level strategic planning for medical care. Within this approach, the patient’s goals are set first, and then their operationalisation is implemented into clinical practice. This is particularly important for patients with multiple chronic conditions, or those with short life expectancies, for whom the standard outcome measures may not be as relevant.1 To explore some challenges related to goal-orientated care and propose solutions to commonly encountered clinical problems, two virtual patient cases that are often seen in clinical practice, for example primary or speciality care, are presented hereafter.
Case Study One
The first patient is a 78-year-old man who presents with decreased appetite, weakness, sadness, and insomnia. He has been diagnosed by his physicians with chronic diseases, including arterial hypertension (HTN), congestive heart failure, Type 2 diabetes mellitus (T2DM), and depression; he receives treatment prescribed by different specialists according to the recent state-of-the-art guidelines. For example, to achieve a better blood pressure control, his cardiologist increased the dose of beta-blockers and diuretics. In addition, to optimise his glycaemic control, his diabetologist increased the dose of blood glucose-lowering medication. Furthermore, his psychiatrist is concerned that the adjustment to the patient’s cardiac medications could potentially aggravate his depression, and, therefore, he advised discontinuation of the beta-blocker therapy and starting a new antidepressant therapy. A primary care physician, knowing that the patient lives alone, recommended a nursing home placement since his care would be easier to manage in the in-patient setting. Overall, and strictly based on medical evidence, the therapeutic choices that were made by these physicians were appropriate. In reality, however, these recommendations were not helpful to the patient, since he still feels fatigued and wishes to stay at home.
Case Study Two
The second patient is an 86-year-old woman with medical history positive for coronary heart disease, a myocardial infarction 20 years ago, HTN, T2DM, thyroid insufficiency, dyslipidaemia, and mild dementia. The patient lives with her family and is cared for by her cardiologist, endocrinologist, neurologist, psychiatrist, and primary care physician. She takes nine prescription medications, as well as a few dietary supplements, amounting to approximately 18 tablets daily. Her physicians strive to achieve target therapeutic goals; however, when a social worker interviewed the patient, she discovered that the patient’s goals were different to those of the physicians and included taking a smaller number of daily medications so as to avoid confusion and minimise potential medication errors. Furthermore, both the patient and her family desired to decrease the number of hospitalisations, since the visits are extremely stressful. At this point, simplification of the therapeutic regimen and honouring the patient’s wish to remain at home for as long as possible should be the main objectives, especially when the life expectancy of the patient is limited.
Discussion of Case Studies
It should be noted that, in both cases, the physicians appropriately followed evidence-based guidelines based on target values for blood pressure and glycaemic control, and adjusted the pharmacotherapy based on separate disease-related goals.2,3 However, there is a discrepancy between the disease-focussed recommendations (strictly followed by these physicians) and the goal-directed treatment approach, which considers the individual patient goals and preferences. Recently, patient goal-orientated care has gained more interest. In practical terms, this means that, instead of fragmented care, where different diseases are treated without the necessary co-ordination, the patient’s goals should be identified as early as possible, as a key element of the interdisciplinary therapeutic management.1,4 This new approach will consequently lead to the eradication of unnecessary medications or an adjustment of treatment doses, subsequently eliminating some related dietary restrictions. It will also motivate patients to participate in exercise programmes and community support groups.1,4 Communication between the treating physicians, both primary care and consulting specialists, is needed to determine what interventions work best for every individual patient, and which professional should be considered as a medical partner ‘in charge’ of the patient’s health.1,4
DISADVANTAGES OF THE DISEASE-CENTRED APPROACH
Common disadvantages of the traditional, fragmented approach of focussing on individual diseases, for example, in elderly patients with multiple comorbidities, include the treatment burden, relevant to often contradictory recommendations for different conditions (e.g., treatments that are beneficial for one disease can worsen the condition of another).5,6 In addition, many treatments do not favour the patients’ wishes. Therefore, expensive medical care often does not translate to the desired outcomes of the patients, their families, and/or their caregivers. This is frustrating for both the patients and medical personnel. Furthermore, when a group of medical professionals is treating many individual diseases in the same patient, it is often unclear who is responsible for prescribing certain medications or making decisions. In this situation, patients aged >70 years who are prescribed ≥5 medications are most vulnerable to medical errors.5,6
ADDRESSING THE PATIENTS’ GOALS AND PREFERENCES
In a recent study survey, a group of primary care physicians who had experience with caring for the elderly population were asked how they approached treatment decision-making in patients with multiple medical conditions, taking many medications, as compared to younger patients without multiple medical conditions. In addition, the doctors were asked to consider how the clinical guidelines should be applied to these elderly patients and whether the patient’s condition influenced the patient’s decision-making.7 According to the survey results, the physicians needed much more information on the risk and benefit ratios for treatments of common comorbid diseases. In addition, they understood theoretically that the patients’ goals and preferences needed to be acknowledged by the treatment team; however, they had received no adequate practical training focussed on these issues. Furthermore, incorporating the patients’ goals and preferences into the management process would require relevant guidelines and quality measures for the patient-centred metrics, rather than for the individual diseases. Compensation for the time spent on precise communications regarding the patient’s goals of care and skilful integration of the medical and personal needs would also be necessary. It is expected that the goal-orientated model will be cost-effective in the long-term, compared to ordering expensive tests and therapies that are often unnecessary or incompatible with the patient’s wishes.8
A TRANSITION FROM DISEASE-CENTRED CARE TO A GOAL-DIRECTED MODEL OF PATIENT CARE
In most circumstances, the optimal time to transition to the goal-directed model of care is when the standard treatment becomes a burden or when it is more likely to cause harm than benefit for the patient. The transition should also be considered when there is a growing discrepancy between the provided medical care and the patient’s own healthcare priorities.8,9 At this point, identification of the most appropriate type of care is required, particularly for patients with multiple chronic conditions.8,9 In practical terms, it is necessary to focus on the patient’s functional outcomes, such as important daily activities. It is also useful to incorporate information about patient functionality into medical records so that the information is easily accessible and easily transmissible to all treatment team members. Moreover, medication reconciliation helps facilitate the goal-directed care for an individual patient since it can verify whether the medications prescribed by different specialists are appropriate, not only for medical reasons but also for achieving the patient’s goals and maintaining quality of life.8,9 However, it should be kept in mind that this approach is not free from potential problems; for example, it may be difficult to operationalise what an individual patient goal could be for personal autonomy. In additon, many patients are concerned about being a burden to their families.
It should be highlighted that disease-based goals are vital to some patients since they are disease-specific and often include specific signs and symptoms, such as dyspnoea, chest pain, or other acute medical problems, and functional or health-related quality of life outcomes (e.g., specific measures for quality of life relevant to arthritis and other chronic conditions) that can be effectively managed. On the other hand, personalised goals are particularly important for patients with multiple chronic conditions or limited life expectancy, for whom the traditional outcome measures may be insufficient; these patients are often interested in their comfort, autonomy, and independence, while their caregivers commonly focus on safety issues.8,9 In summary, both the disease-centred model and the goal-directed model have advantages and disadvantages, and, therefore, physicians should balance these two approaches according to the requirements of the individual patient.
ADVANTAGES AND BARRIERS TO GOAL-DIRECTED, PATIENT-CENTRED CARE
The goal-directed healthcare approach simplifies decision-making for patients with multiple chronic conditions.10,11 It also prompts patients to express what they want from their healthcare, and creates a common, mutually agreed upon path for both the patient and medical provider with regard to the next steps in the medical care.11 There are also many obstacles regarding goal-directed care related to the patients; for example, difficulties in articulating personal health-related goals, literacy, and cultural issues, and to the physicians, such as limited time for appointments, lack of adequate training, and/or insufficient infrastructure (Table 1).10,11 Furthermore, one of the largest barriers to goal-directed care is reductionism between the various specialists, many of whom have different beliefs about what type of specialised tests, procedures, or medications should be applied.11,12 Therefore, it is crucial to determine who is in charge of managing inter-related comorbidities (e.g., malignancy and cardiovascular diseases), or what happens when the recommendations from different specialists conflict. It is possible that many practising physicians may not be prepared for goal-directed care due to a range of factors, including a lack of inclusion in core curriculums and time constraints. Furthermore, the patient’s goals can be transient; for example, after a myocardial infarction and subsequent reduced ejection fraction, the functional goals need to be re-established. The goals can also be unrealistic; for example, a patient who suffered a stroke followed by hemiplegia who wants to drive a car. Medical practitioners need to be prepared for such dynamically changing scenarios and react in a professional manner, whilst also having a supportive and emphatic attitude.
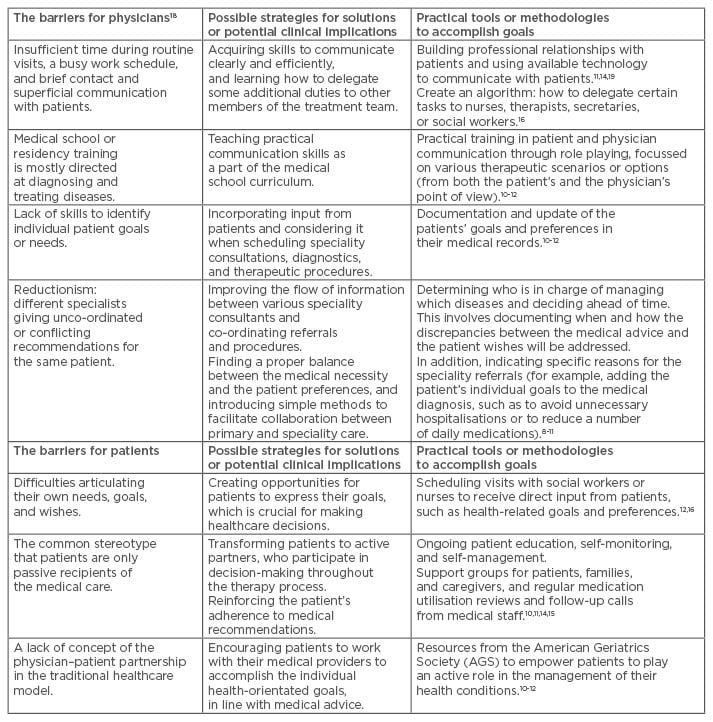
Table 1: The main barriers to goal-directed patient care from the physician’s and patient’s perspective.
POTENTIAL STRATEGIES TO ACCOMPLISH FUNCTIONAL GOALS OF INDIVIDUAL PATIENTS
One of the potential solutions to achieving patient functional goals is the Informatics Corporation of America (ICA) CareAlign® project, which aligns primary and speciality care to focus on priorities that matter most to patients with multiple chronic conditions, based on their medical preferences and goals.13 The project involves primary care and speciality physicians, patients, caregivers, healthcare experts, and organisations. The main goal is to design a flexible healthcare system that is focussed on achieving safe and effective care for better individualised outcomes, in the most economical way. In particular, CareAlign targets the gaps between primary and speciality care, and the discrepancy between addressing standard medical needs and fulfilling individual patient needs, for example, a reduction of disease symptoms, improvement of function, and/or independence.13 In essence, this means that while treating arterial HTN or heart failure for instance, the main purpose of the treatment is to meet the functional goals of the individual patient rather than to strictly manage their laboratory parameters.13
INTEGRATING INPUT FROM INDIVIDUAL PATIENTS WITH THEIR MULTIDISCIPLINARY CARE
The first step in integrating patient input into their multidisciplinary care is to document and regularly update the patients’ goals, which may be subject to change. Therefore, it is necessary to create opportunities for patients to express their goals, which will be crucial for making healthcare decisions. Physicians who have established professional relationships with their patients and are therefore familiar with their patients’ condition and prognosis, should use this relationship to come to a mutual decision, rather than an individual decision, with regard to the recommended therapy as well as other available treatment options, including the associated benefits and risks to the patient.14
Traditionally, for a patient with multiple chronic diseases, several decisions must be made during the short visit to their physician. Since this is usually not feasible and unsatisfactory to physicians and patients, there is a growing need to create a more efficient, shared decision-making model in which the patient, or the designated family member or caregiver, sets the goals, and the treating physicians, or other members of the medical team, estimate the probability that the available therapies can help the patient to achieve these goals.15 Subsequently, a shared care plan should be formulated, in which input from patients is considered when arranging referrals to speciality care (Table 1). Another critical task is to transform the patients from passive treatment recipients to active partners in their healthcare, where they will participate in the decision-making process throughout their therapy. This requires ongoing patient education, self-monitoring, adherence to recommendations, and self-management. Furthermore, since both primary care and specialist physicians do not have sufficient time to address many of these issues, it is essential for them to acquire skills on how to communicate efficiently and delegate some duties to other members of the treatment team for example, nurses, therapists, or social workers (Table 1).15,16
It should be noted that the roles and responsibilities of the team members need to be well established and then flexibly adjusted according to dynamically changing demands. Also, transmitting medical information, including preliminary decisions agreed upon by all team members, to the patients and their caregivers as promptly as possible is of utmost importance. Furthermore, when moving from disease-specific to goal-directed referrals, co-ordination of various medical tasks and optimising interactions between members of multidisciplinary teams are essential. For instance, including not only the patient’s medical diagnosis but also their goals in speciality referrals would not only facilitate collaboration between medical practitioners but also help ensure high-quality care for the patient (Table 1).17
PATIENT ENGAGEMENT AND ACTIVATION
Patient engagement is the willingness and practical knowledge that is necessary for a patient to take a major part in his or her own healthcare. For medical personnel, patient engagement means that the patient is playing the role of the responsible partner, so that the treatment team can best achieve mutually agreed upon goals.18 In this partnership collaboration, the patients are encouraged to develop skills to accomplish their individual health-orientated goals. According to the Society for Participatory Medicine (SPM), engaged patients are not only well educated but also empowered as they move from being passive ‘passengers’ to active ‘drivers’ of their health conditions. Patient activation includes four levels: a) a belief that the physician is completely in charge of the health condition, b) an opinion that, in addition to the physician’s care or guidance, making lifestyle changes will result in better outcomes, c) the patient has a participatory role in the healthcare team, and d) the patient has a driver position and is in control of making healthcare decisions.18 Some patients actively search for healthcare providers who will consider them as partners in their own care.
BENEFITS OF THE PARTICIPATORY MEDICINE MODEL
Patient engagement and active participation in medical care makes a significant difference for both the health of patients and the work of physicians. For instance, in some specialities, like cardiology, oncology, palliative care, or geriatrics, there should be particularly close communication with patients, since there is no single right answer to their complex levels of care. From a physician’s perspective, it is more likely that certain clinical goals will be achieved when the goals have been previously discussed with the patients. Therefore, inviting patients to participate in the care process is superior to solely prescribing medications.19 Moreover, many patients can provide invaluable feedback that will guide further therapeutic choices.20 Participatory medicine has practical implications, especially in the management of chronic diseases, such as T2DM, HTN, coronary heart disease, or congestive heart failure. According to a recent study, a higher patient activation was associated with a reduction of glycated haemoglobin levels.21
CONCLUSION
In summary, implementation of goal-directed healthcare should facilitate the achievement of specific goals that matter most to the individual patients, their families, and their caregivers, and improve their functional outcomes and quality of life. This involves articulating, recording, and forwarding these goals to the entire medical team so that goal-based shared decisions can be made accordingly. Subsequently, integration of patients’ goals with medical recommendations, as well as co-ordination of care between various physicians and medical settings, needs to be well documented and maintained. The two aforementioned virtual patient case studies are commonly encountered in a daily practice setting, and they illustrate how individual situations could be improved using goal-directed therapies. It is possible that certain patients would benefit more from the goal-directed care than the disease-centred care; however, at present, there are not sufficient outcome measures available to evidence this (e.g., patient satisfaction data). To conclude, patient engagement and activation have become a major focus of healthcare, both in clinical and research medicine. Therefore, further studies in patients with multiple chronic conditions, especially older patients, aimed at person-centred care, are definitely warranted.








