METABOLIC dysfunction-associated steatotic liver disease (MASLD) has emerged as the leading cause of chronic liver disease worldwide. Despite its prevalence, the exact mechanisms driving MASLD remain unclear, limiting the development of effective treatments. One emerging area of research suggests that cellular senescence, a state of irreversible cell cycle arrest, plays a pivotal role in MASLD progression.
Aging is a major risk factor for MASLD, as older livers accumulate senescent cells, leading to fibrosis and functional decline. Senescent cells exhibit a unique phenotype known as the senescence-associated secretory phenotype (SASP), releasing inflammatory cytokines, growth factors, and proteases that exacerbate liver damage. While senescence acts as a protective mechanism in healthy tissues, its persistence in diseased organs can drive chronic inflammation and fibrosis.
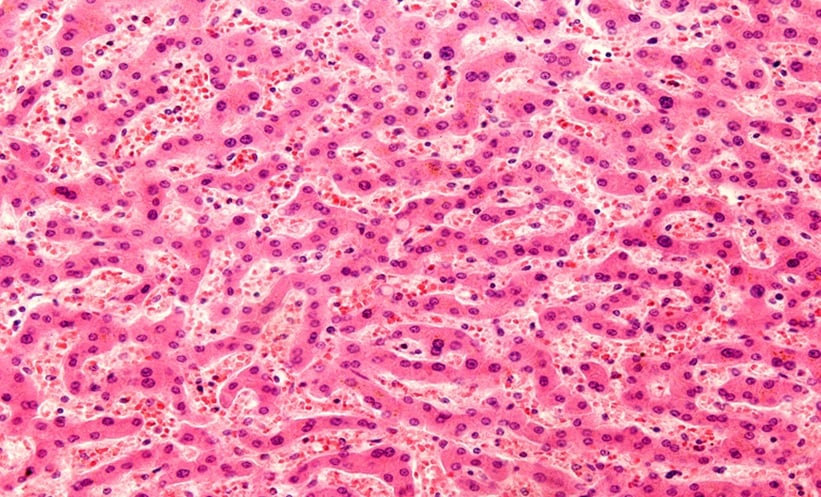
Recent studies have identified a gene signature known as SHGS (senescent hepatocyte gene signature) that tracks with MASLD progression. Researchers used in vitro and in vivo models to demonstrate that SHGS+ hepatocytes not only accumulate in diseased livers but also actively contribute to fibrosis, inflammation, and metabolic dysfunction. Single-cell analysis revealed that these senescent hepatocytes communicate with surrounding liver cells via GDF15-TGFBR2 signaling, further promoting tissue damage.
One of the most promising breakthroughs in this research is the discovery of a novel senolytic compound, DpC. This drug selectively targets SHGS+ hepatocytes, reducing fibrosis, inflammation, and cell death in preclinical MASLD models. Unlike traditional therapies, senolytics like DpC may offer intermittent ‘hit-and-run’ treatment strategies, minimizing side effects while improving liver health.
Beyond the liver, SHGS+ cells have been identified in other metabolic tissues, suggesting that senescence contributes to systemic metabolic dysfunction. The correlation between SHGS activity and damage in the pancreas, heart, and adipose tissue highlights the broader implications of cellular senescence in metabolic diseases.
By targeting senescent hepatocytes, researchers are uncovering new strategies to combat MASLD and its complications. This groundbreaking approach offers hope for more effective treatments, addressing both liver disease and its systemic consequences. Future studies will focus on refining senolytic therapies and exploring their impact on multi-organ dysfunction.
Reference
Du K, Umbaugh DS, Liuyang W, et al. Targeting senescent hepatocytes for treatment of metabolic dysfunction-associated steatotic liver disease and multi-organ dysfunction. Nat Commun. 2025;16(1):3038. Published 2025 Mar 28. doi:10.1038/s41467-025-57616-w