Abstract
Introduction: Hepatitis B virus (HBV) infection remains a worldwide public health problem. The last major review of the epidemiology and management of HBV in the Middle East was published in 2011. This paper aims to assess the current situation of the HBV care pathway in the United Arab Emirates (UAE), identify gaps in our knowledge and barriers therein, and recommend initiatives to be taken to improve the management of such patients.
Methods: A literature search was conducted in PubMed as well as through free internet searches. Interviews and group discussions were held with key opinion leaders and HBV experts.
Results: The national prevalence of HBV is estimated to be approximately 1.0–1.5%; however, prevalence is expected to be higher in those >25 years of age born before the introduction of the HBV vaccination programme. There is limited data on the burden of HBV-related hepatocellular carcinoma in the country.
Discussion: Awareness of various aspects of the disease is perceived to be low among the general population and medium among healthcare providers. There are several mandated national screening structures present; however, there are no country-specific HBV guidelines regarding diagnosis, linkage-to-care, treatment, and follow-up. Improvements have been made in the past 30 years in the UAE, evident through a decline in prevalence. The burden attributable to HBV complication and the coverage of screening and treatment remain unclear.
Conclusion: Key stakeholders in all areas of the HBV care pathway must reduce morbidity and
mortality in the UAE population, and interventions should be supported by research.
INTRODUCTION
Chronic hepatitis B (CHB) is a worldwide public health problem.1 As per the Global Burden of Disease Study, the number of hepatitis B virus (HBV) infections was estimated to be 468 million cases in 2016.1 In the World Health Organization (WHO) Eastern Mediterranean Region, an estimated 3.3% of the general population is infected with HBV. 2
The last updated review of the epidemiology, burden, and management of HBV in the Middle East was published in 2011.3 The authors observed a trend from ‘high-to-intermediate’ to ‘low-to-intermediate’ endemicity.3 Medical experts considered it imperative to assess whether this trend continued, as well as to assess the current situation in the ‘HBV care pathway’.3 The key stages and indicators to consider on the ‘HBV care pathway’ are:
- Epidemiology of the disease and the awareness of different stakeholders about various aspects of the disease.
- Screening for disease, as well as diagnosing patients presenting with symptoms, reporting of positives, and linking them to care.
- Appropriate evaluation of the disease and treatment initiation if needed.
- Compliance/adherence to treatment and periodic patient follow-up.
This paper aims to assess the current situation of the HBV care pathway in the United Arab Emirates (UAE), identify gaps and barriers therein, and recommend comprehensive initiatives to be undertaken to improve the overall situation.
METHODS
A pragmatic literature search was conducted in PubMed to identify evidence on HBV in the UAE using the key words “United Arab Emirates or UAE”, “hepatitis B or HBV”, “chronic hepatitis B or CHB”, “hepatocellular carcinoma or HCC”, “cirrhosis”, “prevalence”, “awareness”, “epidemiology”, “vaccination”, “diagnosis”, “screening”, “treatment”, “care pathway”, and “adherence”. The reference lists of those articles were scanned for any additional articles. In addition, free internet searches were conducted using similar key words to find reports, guidelines, conference abstracts, posters, and presentations. To provide context to the results from the literature review, as well as to collect diverse stakeholder perspectives on those areas for which either no or limited evidence was found in the literature, discussions were held with various healthcare professionals, including key opinion leaders and HBV experts. Different organisations are involved in healthcare provision in the various emirates; in Abu Dhabi, the Department of Health (DOH) (formerly known as Health Authority – Abu Dhabi [HAAD]) is the governing regulatory body and Abu Dhabi Health Services Company (SEHA) is a provider of health services; in Dubai, the Dubai Health Authority (DHA) is both the governing body and service provider; and in the Northern Emirates, the Ministry of Health (MoH) is active. Finally, inputs were taken from the UAE HBV Working Group which included hepatology experts practising in the UAE.4
RESULTS
Prevalence of Hepatitis B Virus Infection
HBV infection rates (HBV surface antigen [HbsAg]-positive) among women of child bearing age in the prevaccination era was 2.5%, based on a mathematical model estimating the HBV burden worldwide using global evidence.5 Since the introduction of the vaccination in 1991, six studies have been conducted to estimate the prevalence of HBV in the UAE. 6-11 From the age of the subjects enrolled, it can be deduced that most of these studies included populations that have either not been vaccinated or are from the prevaccination era.
The most recent study among blood donors found a HBV prevalence of 0.23%.7 With an estimated Emirati population of about 1.2 million in 2016, a prevalence of 0.23% would give an estimated 2,760 HBV cases in the country. Assuming 1.5% prevalence however, which was reported among pregnant women in 2000, would yield an estimate of 18,000 HBV cases in the country.8 Medical experts agreed that the national prevalence is plausibly between 1.0% and 1.5% among the Emirati general population, so the number of HBV infections is estimated to range between 12,000 and 18,000 cases.4
A recent systematic review by Schweitzer et al.12 pooled worldwide data published between 1965 and 2013; in the case of UAE, two studies were included in the review with a total of 1,859 people, which found a prevalence of 0.70%.12 However, it is not clear which UAE studies were included in this review. In general, local prevalence studies conducted in the UAE concentrated more on at-risk populations, such as haemodialysis/end-stage renal disease patients, and continue to show higher prevalence rates than the general population. Furthermore, it would be expected that the prevalence in the older population (>25 years) will be higher because they were born in the prevaccination era, however none of the studies provide prevalence rates by age group.6-11
The UAE started the compulsory vaccination programme for HBV for all newborns in 1991;13 all infants receive 4 doses of the vaccine at 0, 2, 4, and 6 months of age.14,15 Moreover, all school students born before October 1991 were vaccinated by the year 2000.14 One could deduce that at least all Emiratis <25 years of age would have received the first dose of vaccine at birth and hence should be protected from the disease. However, the vaccination of school students born before October 1991 was left to the compliance of students, parents, and schools. With respect to the age distribution of HBV cases, in 2015, 74% of the reported Emirati cases to DOH were >30 years of age (which is an increase from the 62% reported in 2013) and the 30–39 age group contributed the highest proportion (38%).16 Looking at cases reported to DHA, which covers cases in Dubai, the highest number of cases was reported in the 25–34 age group in 2016 (41% of all cases among Emiratis).17 The large numbers of cases in this age group could be a result of strict premarital screening interventions.
Focussing on high-risk groups, a study published in 2010 involving 994 healthcare workers found that 62% of all respondents had been immunised for hepatitis B.18 However, a more recent prospective cohort study that involved 261 (61% female) Emirati medical students conducted between 1st July 2011 and 30th May 2012 found that all students were vaccinated: 40% at birth and the remaining 60% at school.13
No information was found concerning awareness regarding HBV in the community, although this was rated low for general awareness, prevalence of disease, origin, transmission, and high-risk groups by the UAE HBV Working Group.4 This might be because no community awareness campaigns have been conducted recently, the last ones that focussed on HBV dating back to 2007 and 2008. Also, no studies were found assessing the awareness of general practitioners (GP), but medical experts rated this to be medium for general awareness, prevalence of disease, origin, transmission, and high-risk populations.4
Chronic Hepatitis B Virus Burden
People with CHB have a 15–40% lifetime risk of developing end-stage liver disease including cirrhosis, liver failure, and hepatocellular carcinoma (HCC), a primary malignancy of the liver.19 Furthermore, it was found that the health-related quality of life in patients with CHB tends to be impaired in the later stages of liver disease.20-23 In the Arab population, an estimated 6,447 deaths occurred from HBV-associated HCC in 2010, and from 1990 to 2010, the burden of HBV-associated HCC deaths increased at a much faster rate (137% increase) compared to the rest of the world (62% increase).24 Khan G et al.24 reported in 2015 that, in the UAE, the age-standardised death rate for HBV-associated HCC increased by approximately 10% between 1990 and 2010 to 3.2 per 100,000 males, and 1.2 per 100,000 females in 2010 (or 45 deaths among men and 6 among women). No specific reasons were given for the change in the UAE other than what was mentioned for Arab countries in general.
Although vaccines have been proven very effective in HBV prevention in adolescents and led to a decrease in prevalence, it takes decades to observe their effect in HCC reduction in adults.20 No research studies were found on the awareness levels of patients or high-risk populations on the chronicity and consequences of HBV. Experts of the UAE HBV Working Group rated the awareness of GP about clinical sequelae of disease to be medium.4 Genotype D HBV was found to be significantly associated with more advanced stages of liver disease.25 One study, conducted in the UAE, included serum samples of 90 HBV DNA positive subjects and the results showed that genotypes D and A accounted for 77.8% and 17.8%, respectively.26 Another study conducted among 88 HBsAg positive patients found that HBV genotype D was the most prevalent (79.5%) genotype, followed by genotypes A (18.2%) and C (2.3%). In this study, only 5.7% of patients were HBeAg positive.27
Presentation, Evaluation, and Diagnosis
There are a number of mandated screening structures (Figure 1) present in the country identifying patients through blood tests (HBsAg test, antibodies for blood donors).28
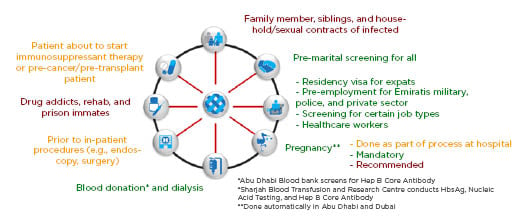
Figure 1: Potential hepatitis B virus screening points in United Arab Emirates.
Per DOH and DHA regulations, HBV reporting is mandated for all healthcare practitioners and facilities licensed by the respective regulator.29,30 Despite reporting being mandatory, gaps in the reporting are still seen. The typical HBV patient journey in the UAE is illustrated in Figure 2.4
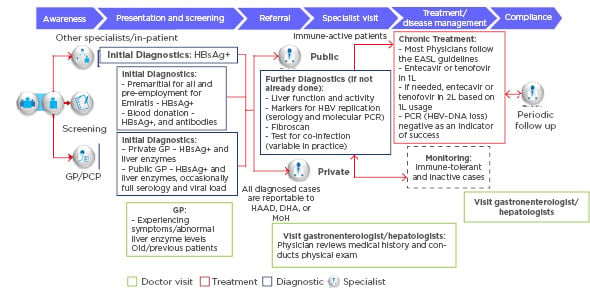
Figure 2: Hepatitis B virus patient journey in United Arab Emirates.
DHA: Dubai Health Authority; EASL: European Association for the Study of the Liver; GP/PCP: general practitioner/primary care providers; HAAD: Health Authority – Abu Dhabi; HBsAg+: hepatitis B surface antigen positive; HBV: hepatitis B virus; MoH: Ministry of Health; PCR: polymerase chain reaction.
Figure 3 shows the number of reported HBV cases over a 10-year period in Abu Dhabi and Dubai.16,17 The number of cases reported to DOH (Abu Dhabi) for both Emiratis and expatriates has increased in the past few years (from 699 in 2013 to 1,121 in 2015). However, in the same period, the number of cases reported to DHA (Dubai) has decreased. Increasing numbers of cases in Abu Dhabi, despite the existence of a vaccination programme, might be attributable to a combination of various factors such as:
- Increased reach and effectiveness of mandated screening interventions.
- Double counting of previously diagnosed cases that were lost to follow-up.
- Double counting of cases attributable to the migration of people from Dubai to Abu Dhabi (and vice versa).
- Emiratis from the Northern Emirates increasingly approaching public hospitals in Abu Dhabi (and Dubai) for treatment.
It is unclear how many cases are diagnosed in the Northern Emirates because no publications could be found on HBV statistics from the MoH. In 2015 only, the total number of reported cases in Abu Dhabi and Dubai was 1,889, of which 322 (17.0%) were Emiratis and 1,567 (83%) were expatriates.
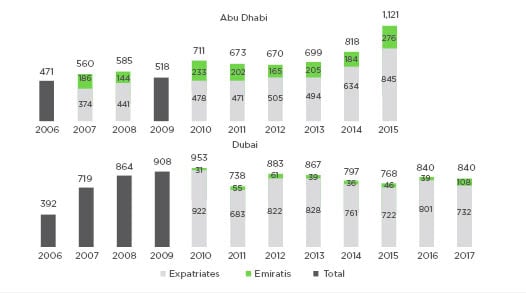
Figure 3: Cases of hepatitis B virus reported to Department of Health (2006–2015)16 and Dubai Health Authority (2006–2017).17
Knowing that approximately 60% of the Emirati population live in Abu Dhabi and Dubai and the remaining live in the Northern Emirates, it could be assumed that the total number of reported HBV cases among Emiratis across the country in 2015 is around 537.
When screened positive or diagnosed positive by a GP in a primary care facility based on symptoms, signs, and abnormal diagnostic tests, patients will be referred to a specialist for further diagnosis.
Treatment and Disease Management
Treatment is delivered to patients in the public sector (Emiratis only) and private sector (both Emiratis and expatriates). In the public sector, specialists/hepatologists and gastroenterologists receive the referrals in their outpatient or hospital-based clinics affiliated to DHA in Dubai, to SEHA in Abu Dhabi, and to MoH in the Northern Emirates. Private sector specialists are available in outpatient ambulatory centres or outpatient clinics in private hospitals. The predominant proportion of HBV care and treatment is delivered in the public sector as it contributes approximately 81% of the HBV prescription share, considering only nucleos(t)ide analogues (NA).28 The majority of the treatment centres are concentrated in Dubai and Abu Dhabi.
Of the approximate 12,000–18,000 prevalent cases in the country, only 21–32% are estimated to be diagnosed (although this may well be an underestimation of the proportion that knows their status, as people could have been diagnosed in previous years).4 Of the diagnosed cases, only 21% are currently on treatment with the majority in the public sector.31 While only a minority of all patients need to be treated as per the current guidelines (approximately 25%),27 the smaller number of treated patients in UAE could be attributed to breaks in the care continuum. It is assumed that some screened and/or diagnosed patients do not reach the specialists and are not linked to care, owing to the lack of a system for monitoring, tracking of patients, and/or proper longitudinal follow-up.
There is no local guideline for HBV; hence most specialists follow the European Association for the Study of the Liver (EASL) guideline.4 However, experts indicate that there are minor variations in specialists’ interpretation of phasing of the disease (HBV DNA levels and serum alanine aminotransferase upper limit of normal); therefore, subsequent variations in the timing of treatment initiation might exist.4 The primary goal of HBV therapy is to improve survival and quality of life by preventing disease progression and death.32 The recommended antiviral therapies for CHB treatment in the country are entecavir (ETV) and tenofovir disoproxil fumarate (TDF). Other treatments, such as pegylated interferon (Peg-IFN-alfa-2a), lamivudine (LAM), telbivudine, and adefovir, have also been approved but are prescribed to a much lesser extent.31 While all drugs have market authorisation in the country, ETV, TDF, and LAM are available in public sector formularies and are provided free of charge to Emirati patients based on specialist prescription.4 Physicians indicate that LAM usage is decreasing and that they prefer ETV over TDF; data show that ETV holds roughly 73% of the patient share for HBV treatment, considering only NA, followed by TDF (approximately 19%) and LAM (8%).31 Physicians’ low prescription of LAM emanates from their poor experience with it because patients developed resistance and had to be eventually shifted to TDF.4 A systematic review found that resistance to LAM emerges in approximately 20% of patients after 1 year and in 70% of patients after 5 years of treatment.33
The main limitation of current antiviral therapy is that the long-term toxicity and health effects are unknown, in a context in which lifelong treatment might be needed.4 Furthermore, disease progression is likely to occur when the suppressive effect of NA is removed; especially in cases of treatment cessation attributable to drug-related adverse events or drug resistance.32,34 There is a significant unmet need for a treatment that can cure HBV. In the absence of such a curative therapy, there is an unmet need for new effective treatment options, with a higher barrier to resistance and with fewer treatment-related adverse events than the currently available treatment options.
Compliance and Adherence
It is recommended that all patients treated with NA should be followed with periodical assessments.32 Nonadherence with recommended follow-up visits is a major barrier for completing treatment and is consequently associated with unfavourable clinical outcomes. Experts in the UAE rate the compliance and adherence to treatment among Emirati patients to be high: approximately 80–90% of the patients who start treatment remain compliant.4
RECOMMENDATIONS
The following recommendations are based on inputs from experts of the UAE HBV Working Group and evidence from the literature review.
There is a need for a nationally representative (including all Emirates) population-based prevalence study (using HBsAg and core antigen screening). Only then can an accurate overall disease prevalence be estimated; in addition, an epidemiology stratification should be made by citizenship status, age (especially the population 25+ years), and gender. Other suggested variables include sociodemographic characteristics, vaccination status, HBeAg status, and mode of transmission, all of which can inform prevention and treatment strategies. It is also advised to establish a national HBV registry, because current data originates from DOH and DHA separately (and reporting systems do not work optimally), with no data available from the MoH in the Northern Emirates. Furthermore, it would be prudent to initiate a broader liver registry, because currently there is limited data on the complications of HBV to inform treatment interventions.
Experts suggest that more research should be conducted on the status of the awareness regarding HBV in the general population and, specifically, in high-risk groups including the elderly, surgery patients (who are not always screened), and medical staff. Use of technology (e.g., social media) and public spaces (e.g., shopping centres) are suggested as key channels.
The WHO advocacy brief highlights that certain prevention and diagnosis targets should be achieved to reach HBV elimination.35 It is important that GP and primary healthcare workers conduct screening of at-risk persons including family members and close contacts of infected Emirati patients and the older population (>40 years old) at high risk of exposure to HBV from the prevaccination era. Hence, with respect to healthcare staff, it is anticipated that establishing training programmes as well as tools and algorithms for GP and public health physicians, to assess high-risk patients visiting their clinics, will lead to improved rates of diagnosis and referral to specialists.
Linkage to care will be maintained only when a system is in place to follow patients through the successive phases of the care pathway. Follow-up of patients is needed along with increased patient awareness (through counselling) to improve treatment compliance and reduce morbidity and mortality. It is recommended that screening for HCC should be increased through simple measures such as the alpha-fetoprotein test and the abdominal ultrasound.
CONCLUSION
In conclusion, significant improvements have been made in the UAE over the past 30 years to reduce HBV prevalence. However, challenges regarding CHB management and long-term follow-up of the disease persist. Specific healthcare initiatives are needed to address these challenges, including the conduct of a population-based prevalence study, launch of educational and awareness campaigns, and improvement of screening and linkage to care. Continuous efforts must be made by all key stakeholders across the care pathway (hepatology specialists, GP, policy makers, and public health specialists) to reduce both morbidity and mortality of HBV in the UAE population.








