BACKGROUND AND AIMS
The prevalence and prognostic relevance of cirrhotic cardiomyopathy (CCM), as defined according with the new core criteria proposed in 20191 is still unknown. The authors investigated this relevant issue in a large cohort of cirrhotic patients in different stages of liver disease.
METHOD
The authors retrospectively interrogated a data set of 162 collected cirrhotic patients followed up for at least 6 years, which at baseline underwent standard Doppler echocardiography and were compared with 46 healthy subjects. Left ventricular (LV) geometry, systolic/diastolic function, global longitudinal strain and the main haemodynamic parameters were assessed according with current guidelines.
Systolic dysfunction was diagnosed if LV ejection fraction ≤50%, and/or GLS <18% or >22%. Advanced diastolic dysfunction was diagnosed if ≥3 of the following: left atrial volume index >34 mL/m2, tricuspid regurgitation velocity >2.8 m/sec, early diastolic peak velocity of septal mitral annulus (septal e’) velocity <7 cm/sec, early diastolic transmitral and myocardial velocity on tissue Doppler imaging ratio (E/e’) >15, as proposed in the new criteria.1
RESULTS
Adequate echocardiographic images permitting speckle tracking analysis were available in 83 patients. No patient presented LV ejection fraction ≤50%; GLS <18% or >22% was evident in 25%; advanced diastolic dysfunction was evident in 10%. Overall the prevalence of CCM was 29%. Patients with and without CCM presented similar clinical, biochemical, haemodynamic and echocardiographic features at baseline, and similar incidence of death and/or hepatorenal syndrome after 6 years follow-up (see Table 1).
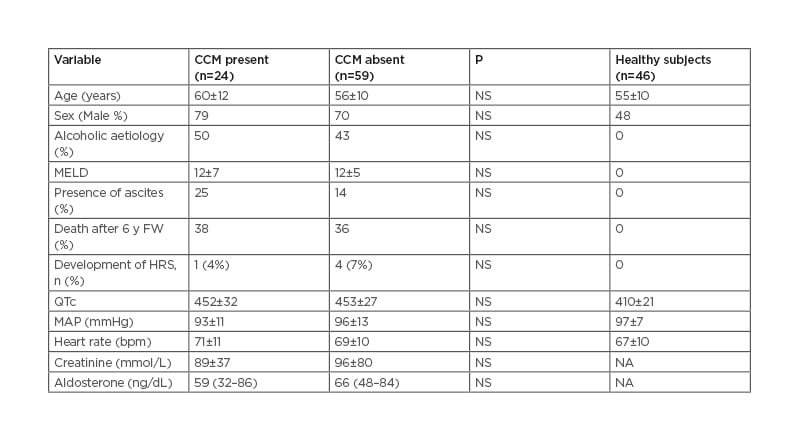
Table: Clinical, demographic, and biochemical features of cirrhotic patients with and without cirrhotic cardiomyopathy.
The data are reported as mean±SD or median (and interquartile range) as appropriate.
HRS: hepatorenal syndrome; MAP: mean arterial pressure: NA, not available; NS: non-significant.
CONCLUSION
According with the new criteria CCM was detected in 29% of patients, mainly due to altered GLS at rest, but without prognostic relevance and therefore not optimal for the clinical management of cirrhotic patients.








