Accurate diagnosis of essential thrombocythaemia (ET) and differentiation between ET and pre-fibrotic stages of primary myelofibrosis (PMF) can be challenging.1,2 Although bone marrow (BM) biopsy examination is the gold standard necessary for accurate classification, in clinical practice it might be helpful to identify, among patients with a working diagnosis of ET, those most likely to have early PMF or unclassifiable MPN (MPN-U).3 Recent clinicopathological studies revealed that laboratory parameters like sex-matched haemoglobin (Hb; <120 g/L for females and <130 g/L males), white blood cell (≥13 x109/L) count, and lactate dehydrogenase (LDH; >200 mU/mL) values are significantly different in PMF and ET. To that end, Carobbio et al.4 developed a simple diagnostic algorithm that, based on these parameters, might alert clinicians of early PMF in a patient presumably presenting with ET.
The Personal Practice Assessment (PPA) programme is a means of collecting routine practice patient and treatment-related information. Participating clinicians were asked to review charts of their patients who met specific clinical parameters. The primary objective of this PPA initiative was to assess the applicability of Carobbio et al.’s4 algorithm in daily Canadian practice and its potential to identify MF suspects among ET patients. The initiative was conducted in nine Canadian institutions. Nine haematology/pathology pairs reviewed charts of ˜10–20 patients with thrombocytosis suspected to have ET. The first 5 of 10–20 cases who met the Carobbio algorithm were selected for BM evaluation. To avoid the impact of treatment and/or disease evolution on accurate classification, the requirement was for the BM biopsy to be collected within a year from the patients with thrombocytosis.
A total of 127 patients (53 males and 74 females; 57% >5 years of age; 67% with LDH ≥200 mU/mL) with a clinical history indicative of ET were initially assessed. The presence of blasts or other immature myeloid cells (promyelocytes, myelocytes, or metamyelocytes) were detected in 9 (7%) of these patients, nucleated red blood cells (erythroblasts) were present in 5 (4%), and leukoerythroblastosis in 2 (2%) of patients. Out of 127 patients, 44 (35%) met the criteria outlined in the Carobbio algorithm: 20 out of 53 (38%) males and 22 out of 74 (30%) females. The BM examination was performed on 35 patients who met pre-specified criteria for the timing of BM biopsy.
Roughly one-third of the 35 patients met the WHO classification for ET and one-third for PMF. While 1 of the remaining patients met the criteria for polycythaemia vera, it was uncertain whether the rest represented true ET or early PMF, i.e. they represented MPN-U (Figure 1). Patients who met the World Health Organization (WHO) criteria for PMF were more likely to have anaemia and/or leucocytosis than those classified as ET (Table 1).
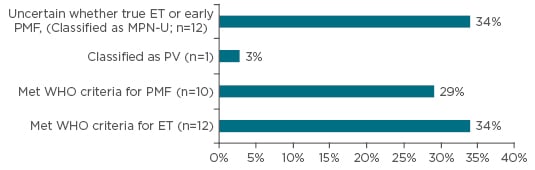
Figure 1: Reclassification based on bone marrow examination (n=35).
ET: essential thrombocythaemia; PMF: primary myelofibrosis; MPN-U: unclassifiable primary myelofibrosis;
PV: polycythaemia vera; WHO: World Health Organization.
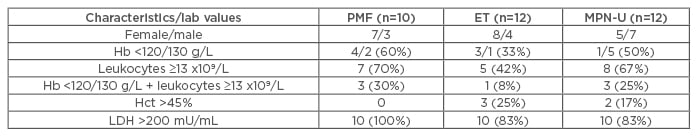
Table 1: Clinical parameters of patients who met specific WHO classification.
PMF: primary myelofibrosis; ET: essential thrombocythaemia; MPN-U: unclassifiable primary myelofibrosis; WHO: World Health Organization; Hb: haemoglobin; Hct: hematocrit; LDH: lactate dehydrogenase.
Despite its methodological limitations, this innovation confirms that the Carobbio algorithm can be used in clinical practice to identify cases of early PMF and MPN-U among patients suspected to have ET. It suggests a need for educational initiatives on using the algorithms to separate ET from PMF. It does, however, confirm the importance of haematologist–pathologist collaboration in reaching a final integrated diagnosis based on the WHO classification. These findings warrant further investigation in larger prospective studies.







