BACKGROUND AND AIMS
Anaemia is a public health problem. Two aetiologies of microcytic anaemia are relatively common in Tunisia: iron deficiency anaemia (IDA) and β-thalassaemia minor (βTM). To guide the clinician in discriminating IDA from βTM, several studies have developed indices and formulas based on blood count parameters determined by haematology analysers. The aim of this study was to evaluate the performance of these formulas to discriminate βTM and IDA and to identify the cut-off values adapted to the studied population for each formula.
MATERIALS AND METHODS
After reviewing the records of adult patients with IDA and βTM, two groups were formed (IDA: n=172; and βTM: n=69). Demographic and blood count data were recorded. Performances of ten formulas and indices reported in the literature in the discrimination between IDA and βTM were studied. Statistical analysis was performed using SPSS® Statistics (version 19.0; IBM, Armonk, New York, USA). Sensitivity (Se), specificity (Sp), likelihood ratios, predictive values, and analysis of receiver operative characteristic curves were carried out. For each formula, optimal cut-off values were determined according to the Youden index. The study was conducted in accordance with the Helsinki declaration. No personal identification data were collected.
RESULTS
The haemoglobin rate, the erythrocyte count, and the red blood cell distribution index by standard deviation parameters showed an excellent discriminating power (area under the curve [AUC]: 0.913, 0.971, and 0.968, respectively). Performance assessment of the various original cut-off indices showed that Green and King (G&K) index (Se: 71.01%; Sp: 97.67%; AUC: 0.96), red cell distribution width (RDW) index (Se: 78.26%; Sp: 97.67%; AUC: 0.95), and Sirdah index (Se: 76.81%; Sp: 97.67%; AUC: 0.965) were reliable. At the new cut-off, the England and Fraser (E&F), G&K, Sirdah, and RDW indices were the most effective in diagnosing βTM (Table 1). At these new thresholds, both E&F and Sirdah indices showed a gain in Se and accuracy.
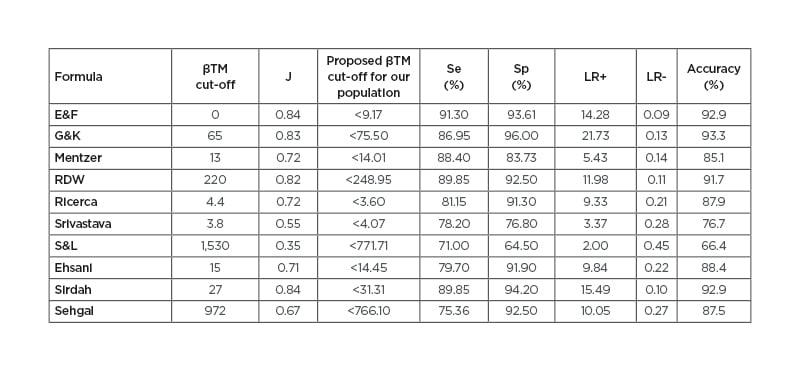
Table 1: Performance of the new respective indices cut-off values in the discrimination of β-thalassaemia minor and iron deficiency anaemia.
βTM: beta-thalassaemia minor; E&F: England and Frazer index; G&K: Green and King index; J: Youden index; LR: likelihood ratio; RDW: red blood cell distribution width; Se: sensitivity; Sp: specificity; S&L: Shine and Lal index.
In accordance to these results, recent study and meta-analysis proved that the erythrocyte count was an effective discrimination tool for IDA and βTM at a cut-off value of >5×106/mm3 with an AUC of 0.921;1,2 however, discrepant results with much lower performances were found.3 At original cut-offs, many studies showed the limited performance of the Shine and Lal (S&L) formula.3,4 In the Tunisian study of Sahli et al.5 the S&L formula provided a Se of 98% but a Sp of 50%.5 The meta-analysis of Hoffman et al.6 stated that the S&L formula would be preferred in a Mediterranean population, in addition to the Mentzer and Sirdah indices. Considering new respective cut-off values of all indices studied, only E&F, G&K, RDW, and Sirdah indices showed AUCs >0.8, high likelihood ratios, and accuracy >90%.
These findings were consistent with many studies conducted in Spanish, Iranian, and Indian populations.4,7,8 In Tunisia, there is no national thalassaemia screening programme as in some countries.9,10 Moreover, very few Tunisian studies on the assessment of these formulas are published. The reliability of Mentzer and Srivastava indices (with an accuracy of 85% and 94%, respectively) with an AUC >0.9 of the new proposed cut-offs was reported.5
CONCLUSION
The adoption of population-specific cut-offs helps to improve the performance of these formulas and indices and could considerably reduce unnecessary iron therapy and diagnostic expenses. The technology deployed by haematology analysers and some clinical data would be necessary for optimal diagnostic guidance.







