Abstract
Colon cancer remains one of the leading causes of cancer-related morbidity and mortality worldwide and it is generally accepted that most colorectal cancers arise from precursor adenomatous polyps. Malignant colorectal polyps should be resected en bloc, if possible, to facilitate thorough evaluation by the pathologist. This review will discuss the important parameters of malignant polyps that are prognostically important, with special emphasis on the pathological assessment of these polyps, which is important for planning further management and treatment strategies for patients.
INTRODUCTION
The word polyp simply means mucosal protrusion and it carries clinical significance only if the pathologist attaches a histopathological label. The polyp could be inflammatory, hamartomatous, serrated (hyperplastic), or neoplastic (dysplastic). Polyps assume one of two classical appearances: pedunculated polyps, which protrude for >2-fold the thickness of the adjacent mucosa and have a base smaller than one-third of the diameter of the head of the lesion; or sessile polyps, which have a base and top of the lesion that are approximately the same width. The term subpedunculated polyps is used by some specialists; these polyps are intermediate broad-based lesions that are dealt with in the same way as sessile lesions.1,2
Malignant colorectal polyps (MCRP) are common enough to warrant special attention and, with the introduction of bowel cancer screening programmes worldwide, large numbers of these polyps are being detected. Results have indicated that up to 50% of screen-detected cancers are identified in the early stages of disease progression.3,4 This article details the frequency, malignant potential of adenomas, and pathological assessment of MCRP.
EPIDEMIOLOGY OF ADENOMAS
The prevalence of colorectal adenoma in a post mortem series ranged (female to male) from 14–20% in the <54 year-old group; 20–34% in the 55–64 year group; 35–44% in the 65–74 year group; and 33–52% in the >75 years group, with the prevalence increasing with age.5 The prevalence of MCRP in a series of endoscopically removed polyps was between 0.2% and 11.0%.6
In the clinical setting, there are various statistics linking the prevalence of adenoma with cancer. Of the first 1 million individuals screened in the NHS bowel cancer screening programme in England, >17,000 patients had a positive faecal occult blood test result. Of these, 1,574 (9%) were diagnosed with cancer, of whom 155 (10%) had polyp cancer.1 Seventy-one percent of cancers were ‘early’ (32% Dukes A and 30% Dukes B) and 77% were left-sided, (29% rectal and 45% sigmoid). Only 14% of the cancers were right-sided, compared with expected figures of 67% and 24% for left and right-sided cancers, respectively, from the UK cancer registration.
The traditional question about the natural progression of adenoma was partly answered by the Mayo clinic group;7 when they radiologically followed cohorts of patients with adenoma of ≥10 mm, they found that after 5 years there was 2.5% risk of malignant transformation, which increased to 8.0% after 10 years and 24.0% after 20 years. A limitation of this study is that there was no prior histological identification of the polyp type and they were assumed to be adenomatous.
POLYP HANDLING
Appropriate handling and assessment of polypectomy specimens in the laboratory is important for adequate interpretation of data, which ultimately affects patient management. To achieve optimal preparation, once the polyp is removed, it should be received fresh, pinned onto a cork board, and left to fix for at least 24 hours. Serial slicing along the stalk will ensure satisfactory assessment. Examination at a minimum of three levels is also beneficial and highly recommended. Exact identification of different sites by placing the polyps in separate containers is also recommended. From the personal experience of the authors, in some cases there is a variance between the endoscopic assessment as pedunculated and the pathological assessment as sessile. In such cases, this is probably the result of the endoscopists not taking out the entire stalk.
ADENOMA ARCHITECTURE
Adenomas are histologically divided into tubular, tubulovillous, or villous types according to the World Health Organization (WHO) 25% classification rule.8 At least 25% of the volume of an adenoma should be villous to be classified as a tubulovillous adenoma and 75% villous to be defined as a villous adenoma.8
The 25% rule only applies to fully excised polyps, when the entire polyp can be assessed on the slide. In cases of small and fragmented lesions or superficial polyp biopsies, the presence of any identifiable villous component would classify the polyps as tubulovillous.3,8
ASSESSMENT OF ADENOMA SIZE
Size is one of the most important risk factors for malignant transformation in an adenoma. Nusko et al.9 have shown that the incidence of polyp cancer is up to 40% in polyps >25 mm and up to 75% when the size reaches 35 mm. In the same series, the incidence of carcinoma in a polyp was around 11%.9 In addition, increasing polyp size was seen to correlate with other adverse features, such as villous morphologyand high-grade dysplasia.
In a study of 13,992 asymptomatic patients undergoing screening colonoscopy, correlation of increasing size with adverse features was confirmed, with the proportion of advanced histology (villous morphology, high-grade dysplasia, or an invasive cancer) cases being 1.7% in the 1–5 mm group, 6.6% in the 6–9 mm group, and 30.6% in polyps >10 mm.10 In view of the association with clinical outcome, polyp size is one of the factors used in decision-making regarding the need for future surveillance and assessing further management strategies. Polyp size is usually an objective parameter that is best assessed by the pathologist, because inaccurate size estimation can adversely affect a patient’s management. Histological assessment of the size on the slide, as opposed to endoscopic measurement, is preferable because it is auditable, accurate, and simple to perform unless hampered by specimen fragmentation.
Levene et al.11 conducted a study including 235 adenomtous polyps, of which 89% of adenomas had a documented endoscopic measurement and 22% a pathological measurement; the median endoscopic measurement was significantly greater, resulting in 13% of patients being misclassified as high or low risk, adversely affecting surveillance strategy.
Measuring the largest diameter on the haematoxylin and eosin-stained slide to the nearest millimetre is currently the most accurate assessment, and this should involve measuring the dysplastic component of a polyp excluding any normal component and normal stalk. If the specimen is received fragmented, it should be specifically stated in the report as not assessable and endoscopic measurements should be considered.3,12,13
GRADING OF EPITHELIAL DYSPLASIA
All adenomas are dysplastic by definition, and dysplasia is defined as epithelial changes that are unequivocally neoplastic.14 Grading of dysplasia in adenomas should be exercised according to the revised Vienna classification of gastrointestinal epithelial neoplasia, using the two-tiered system of low and high-grade dysplasia.15
Low-grade dysplasia is an unequivocal neoplastic condition confined to the epithelial glands and this should be differentiated from inflammatory or regenerative changes.14 High-grade dysplasia, in contrast to low-grade dysplasia, is characterised by complex glandular crowding and irregularity, prominent glandular budding, cribriform architecture, and ‘back-to-back’ glands with luminal papillary tufting (Figure 1A and Figure 1B).
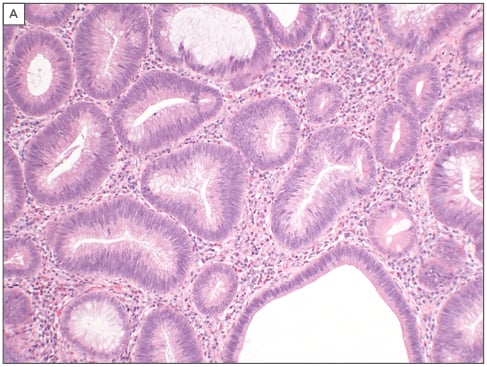
Figure 1A: Features of low-grade epithelial dysplasia with mild cellular stratification of glands.
The glands show evidence of low-grade dysplasia, with mild cellular stratification of glands and no evidence of complex architecture.
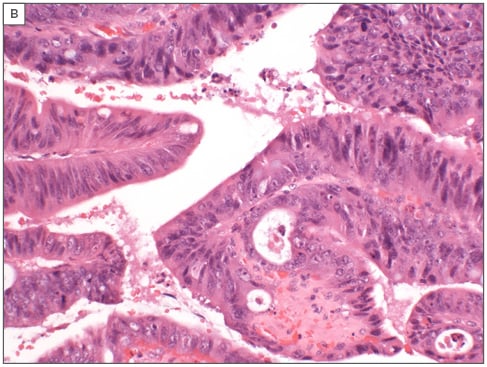
Figure 1B: Features representing high-grade dysplasia with prominent cellular stratification and complex glandular architecture.
The glands show more evident cellular stratification, with hyperchromatic nuclei and more complex architecture.
High-grade dysplasia in an adenoma is a risk factor for frank malignant transformation, but there are exceptions to this rule because sometimes invasive carcinoma arises from low-grade dysplasia. However, it is standard to use the term malignant polyp on malignancy complicating adenomas and this is the term the authors will use in this paper. Although there are other forms of malignant polyps, like metastatic tumours, specifically malignant melanoma, neuroendocrine tumours, and various connective tissue cancers, including stromal tumours and polypoidal lymphomas, these are more rare. This paper will focus on malignancy complicating adenoma.
A number of studies have shown good concordance for the recognition of adenomatous features, but much lower levels of agreement for the assessment of histological type and grade of dysplasia, with interobserver variability higher among general pathologists than specialist gastrointestinal pathologists.16,17
ADVANCED ADENOMA
Advanced adenoma refers to adenomatous polyps that are either ≥10 mm in size, containing high-grade dysplasia, or villous in architecture, since these polyps are at a higher risk of malignant transformation. The term advanced adenoma should be avoided in pathology reports, and instead the pathologist should accurately describe each of the high-risk features, especially high-grade dysplasia, since increasing size is closely linked with the presence of high-grade dysplasia and is the most practical determinant of subsequent colorectal cancer risk.3,12,17,18
MALIGNANT COLORECTAL POLYPS
MCRP are adenomatous polyps in which cancer has developed and invaded through the muscularis mucosae (which acts as a protective biological basement membrane) into the submucosa. The lamina propria has a limited effective network of blood vessels and lymphatics, and, hence, invasion within the lamina propria does not carry metastatic risk; however, once the neoplasm breaches the muscularis mucosa into the submucosa, to be in a region rich with lymphatic and vascular channels, the metastatic risk becomes a real clinical threat.19
The experienced endoscopist can strongly suspect or even accurately diagnose MCRP from the following parameters: large and/or flatter polyps, ulceration, firmness, Paris Type 0–IIc, Kudo pit pattern type V, lateral non-granular spreading, or non-lifting. These parameters are not available to the pathologist and often it is a surprise diagnosis.20
HIGH-RISK HISTOLOGICAL FACTORS FOR REGIONAL AND DISTANT METASTASIS IN MALIGNANT COLORECTAL POLYPS
The overall frequency of lymph node metastasis in MCRP is around 10%;21,22 once the diagnosis of MCRP is established, the risk of local and distant spread depends on certain risk factors.23-25 A study by Hassan et al.23 looked at looked at pooled data from 1,900 cases in 31 studies and assessed risk factors and their associations and found that poor differentiation, including signet ring pattern, was associated with increased mortality, positive resection margin associated with presence of residual disease, and lymphovascular invasion with high nodal metastasis. However, there is often a combination of these factors. Beaton et al.26 added tumour budding and depth of invasion of >1 mm as risk factors for lymph node metastasis. In addition, Haggitt level 4 and Kikuchi level 2 and 3 of invasion have been found to carry risks for loco-regional and distant metastasis.27,28
HISTOLOGICAL TUMOUR TYPE AND DIFFERENTIATION
It is estimated that >95% of colorectal cancers are adenocarcinomas29 and the conventional adenocarcinoma is characterised by glandular formation, which is the basis for tumour grading. Signet ring cell carcinoma has stage-independent adverse prognostic significance relative to conventional type adenocarcinoma, including mucinous adenocarcinoma, which has a better prognosis.8
Tumour grade and differentiation is regarded as a stage-independent prognostic factor; thus, high-grade or poorly differentiated tumours are associated with poorer prognosis.8 Between 4 and 7% of MCRP show poor differentiation and this is usually an indication, combined with other factors, for surgery as the risk for nodal involvement is up to 70%.23 There is a lack of universally agreed criteria for assessing poor differentiation and several guidelines recommend that when any area of the lesion shows poor differentiation, the tumour should be regarded as poorly differentiated.3,13 The Royal College of Pathologists (RCPath) states that poor differentiation should be based on the worst area until the situation is clarified by further research.13
RESECTION MARGIN
Involvement of the resection margin in MCRP represents an adverse outcome and is considered a high risk factor.12,13,30 Involvement of the mucosal margin may necessitate further local excision, while involvement of the deep stromal margin is usually an indication for a wider surgical excision. There is considerable discussion in the literature on the status of the margin clearance and what is considered acceptable to classify the tumour as completely excised. Most of the guidelines on this issue recommend that clearance of ≤1 mm signifies a positive and involved margin and is considered a higher risk factor.3,13 In a recent study, Lopez et al.30 showed that the outcomes following polypectomy in patients with a pathological margin ≥1 mm were similar to those following surgery in the general population. In the same study, the authors recommended that endoscopic resection needs to be completed by surgery if pathological margins are <1 mm30 and other studies have also shown that resection was more likely to follow polypectomy if polypectomy margins were positive.25,31
EXTENT OF TUMOUR INVASION (STAGING)
There are several staging systems devised to assess the depth of tumour invasion in a MCRP, since increasing depth of invasion has been associated with adverse effects and higher risk of lymph node involvement. The most commonly used systems to date are those devised by Kikuchi et al.27 and Haggitt et al.,28 although other systems have been used on a smaller scale, such as those investigated by Kudo,32 Ueno et al.,33 and Nascimbeni et al.34 In pT1 MCRP, the frequency of lymph node metastasis in sessile tumours that involve the superficial, middle, and deep thirds of the submucosa (Kudo and Kikuchi levels sm1, sm2, and sm3, respectively) has been reported to be 2%, 8%, and 23%, respectively.27,34 On the other hand, in polypoid tumours, the level of invasion into the stalk of the polyp has been identified as important in predicting outcome. For example, Haggitt28 found that ‘level 4’ invasion, in which the tumour extended beyond the stalk of the polyp into the submucosa, but not into the muscularis propria, was an adverse factor. However, neither Kikuchi nor Haggitt systems are easy to use in practice and can both be subjective. The Haggitt level is particularly difficult to use in polypoid specimens lacking a clearly defined stalk (‘sub-pedunculated’) or if the specimen is poorly orientated. The Kikuchi method is not suitable for assessing samples in which the muscularis propria is not present. In addition, these systems depend on the subjective assessment of the pathologist, hence it is liable to significant observer variation.
Ueno et al.,33 in their study of 292 patients with early invasive cancer, proposed that assessment of the width and depth of tumour invasion in millimetres is a better predictor of clinical outcome. They showed that when submucosal invasion width was <4 mm, the incidence of nodal metastasis was 2.5%. However, incidence of nodal metastasis was 18.2% when the width was ≥4 mm. When the submucosal invasion depth was <2 mm, the incidence of nodal involvement was 3.9%, but was 17.1% when the depth was ≥2 mm. Work from the Oxford Group35 showed significant interobserver variation among pathologists when measuring polyp width using Ueno’s staging method. However, the study highlighted a better agreement in measuring the depth of invasion and the researchers concluded that Ueno’s method has the advantage of being independent of polyp morphology.
The authors’ research group investigated 56 cases of polyps thought to be endoscopically benign but were malignant.36 Four gastrointestinal pathologists scored the slides independently according to an agreed proforma and the results were collated. Significant variation in the assessment of agreed-upon important prognostic parameters using the various published staging systems was observed.27,28,33 There was poor or fair agreement on the assessment of histological differentiation, Haggitt levels, lymphovascular invasion, and width of invasion measured in millimetres, similar to findings in other studies.37 The best agreement was in the assessment of tumour invasion depth in millimetres according to Ueno classification. The conclusion that none of the staging systems used are suitable for all polyp types or had good reproducibility was drawn, leading to the recommendation to use all suitable systems when reporting MCRP samples.
There is an urgent need to make pathological assessment of MCRP easier and more reproducible; however, the authors recommend that pathologists adhere to agreed parameters and apply them rigidly while also making use of more than one staging system.
LYMPHOVASCULAR INVASION
The other important issue is the problem of combining lymphatic and vascular invasion under the term lymphovascular invasion. Although in simple haematoxylin and eosin stains it is more often than not the pathologist who finds it difficult to differentiate lymphatic from venous channels, the combination approach lacks scientific credibility as the final destination of the lymphatic drainage is different from venous drainage, with totally different clinical outcomes and requiring different therapeutic applications. The authors have argued along these lines38 and suggested that the use of the currently available immunohistochemical stains (e.g., podoplanin and CD34) to differentiate lymphatic from venous and vascular invasions would significantly advance our knowledge in this area.
TUMOUR BUDDING
Tumour budding is an established independent prognostic factor in colorectal cancer but a standardised method for its assessment has been lacking. In the literature, tumour budding is defined as isolated single cancer cells or small clusters (<5 cells) of cancer cells at the infiltrating edge of the tumour and when there are 5 or more buds per 20 power field.33 Studies of part 1 cancers have shown that the presence of tumour budding is associated with increased frequency of lymph node metastasis and also correlates with other adverse histological features.26,33 This was confirmed by a recent study that showed that the presence of a higher number of tumour budding foci is associated with an increased risk of nodal metastasis.25
There are various methods in the literature to report and assess tumour budding and there is no one preferred or recommended method to define budding, including the use of immunostains; hence, routine reporting of tumour budding is currently not recommended as standard.12,13 This is despite a report from the International Tumour Budding Consensus Conference (ITBCC), which was established to find standardised criteria to define this phenomenon.24 The overall consensus of the meeting supported the strong evidence for this important prognostic parameter and proposed that this method be incorporated into colorectal cancer guidelines/protocols and staging systems.
PITFALLS IN THE PATHOLOGICAL ASSESSMENT OF MALIGNANT COLORECTAL POLYPS
The main issues that face pathologists in the interpretation of adenomatous polyps are inaccurate sampling, recognition of muscularis mucosa in invasive malignancy, and the phenomenon of epithelial misplacement/pseudoinvasion.
Inaccurate Sampling
If the polyp is incompletely removed, the biopsy may not reveal the entire story because superficial biopsy may not include the muscularis mucosa or, as is often the case, the biopsy hits the benign part of the polyp and the malignant component is not included; therefore, the pathologist will give the report as benign and the authors think this is inappropriate. The authors have investigated this area39 and showed that there was a false-negative report of 18.5% of MCRP when the original biopsies were compared with the subsequently completely resected specimens. The authors have since started using a template polyp report as follows: this is a tubular (or tubulovilous, or villous) neoplasm showing low-grade dysplasia (or high-grade dysplasia). If this is representative of the lesion then this is an adenoma; however, if this is part of a larger lesion then a more sinister pathology cannot be excluded. The authors feel that they have been honest with the clinician and the patient. Subsequently a Spanish group40 showed a 18.8% false-negative pathology report on incompletely removed rectal polyps. Furthermore, the same study showed that 30.7% of the cohort were, in fact, T2 and 17.3% were T3, while the original biopsy was reported as benign.
The Recognition of Muscularis Mucosa in Invasive Malignancy
The issue of invasion beyond the muscularis mucosa is crucial, but characteristically the invading neoplastic cells secrete metaloprotein 9, which has been shown to destroy the muscularis mucosa.41 Subsequently, Haboubi and Farroha42 reported that when applying strict histological criteria, such as desmoplasia, irregularity of glands, high mitotic activity, tumour necrosis, and brisk inflammatory cell infiltrate, an experienced histopathologist can accurately diagnose cancer in the absence of muscularis mucosa, even from superficial biopsies.
Most literature and guidelines suggest that the presence of a desmoplastic stromal reaction to dysplastic glands is often considered acceptable for a diagnosis of invasive malignancy, as this phenomenon is rare in ‘intramucosal adenocarcinoma’.3,13 However, in biopsies taken from polypoid lesions, caution should be exercised as these can occasionally show desmoplastic stroma without the presence of submucosal invasion due to the effect of the previous endoscopic biopsies or partial polypectomy from the same site.13
A retrospective study for detection of desmoplastic reaction in biopsy specimens of early colorectal cancer from 359 patients with resected submucosal invasive colorectal cancers, who had undergone surgical or endoscopic mucosal resection, were analysed. For pedunculated, resected, submucosal, invasive colorectal cancers, the prevalence of desmoplastic reaction was not significantly related to submucosal depth. However, for non-pedunculated cancers, the prevalence of desmoplastic reaction in pre-treatment biopsy specimens was significantly related to submucosal depth.43 In addition, the desmoplastic reaction positivity rate in pretreatment biopsy was significantly higher in those with a submucosal depth of ≥1,000 μm than those with a submucosal depth of <1,000 μm.
Epithelial Misplacement/Pseudoinvasion
Epithelial misplacement, first described by Muto et al.45 in 1973, refers to the misplacement of the mucosa into the submucosa that mimics invasive cancer and, in many cases, leads to diagnostic difficulty for pathologists. Even for experienced gastrointestinal pathologists, this phenomenon poses diagnostic difficulty in differentiating invasive carcinoma from pseudoinvasion.21,44-46 It is commonly seen in prolapsed polyps in the sigmoid colon and is perceived to be one of the most difficult areas in the interpretation of polyps and in the context of a bowel cancer screening programme.
With the introduction of bowel cancer screening in many countries, there has been an improvement in the detection of early-stage cancer (e.g., Dukes A) in screened versus nonscreened populations (45.3% versus 10.1%, respectively).2 In addition, adenomas are the most common type of polyp found during bowel cancer screening, comprising >60% of all polyps detected in the UK,46 with the sigmoid adenomas being larger than similar polyps detected elsewhere in the bowel, and many of these tend to tort, bleed, and ulcerate. Despite this being a common and well-recognised phenomenon, this is still perceived as the most difficult area in the interpretation of polyps in the context of bowel cancer screening.47-49 Recognising this difficult area, the British bowel cancer screening programme has created the ‘Expert Board’ in the UK, financed by the British programme, to deal with these difficult cases, and case referral is free. Since its establishment in 2009, >200 cases have been assessed by this board, which consists of three gastrointestinal pathologists to ensure a majority diagnosis, since agreement is by no means universal, emphasising the difficulty of this process. A recent paper describing difficult cases referred to the bowel cancer screening programme Expert Board showed that around 78.9% of the polyps referred were from the rectosigmoid junction and in 50% of cases the diagnosis was reversed from the opinion of the original reporting pathologist, in which the main issues were around epithelial misplacement.49
The main histological features that favour epithelial misplacement are:21
- The displaced epithelial is usually similar to that of the surface adenomatous component.
- Haemosiderin deposition.
- The presence of lamina propria around misplaced glands.
- Mucosal prolapse changes often present.
- Absence of budding, desmoplastic reaction, and lymphovascular invasion.
The bowel cancer screening programme recommends that all MCRP (part 1 polyp cancer) are to be reported by two pathologists with experience in gastrointestinal pathology to prevent overtreatment and unnecessary resections.12,13 For consistency of reporting important data in a MCRP, the RCPath dataset is represented in Figure 2.
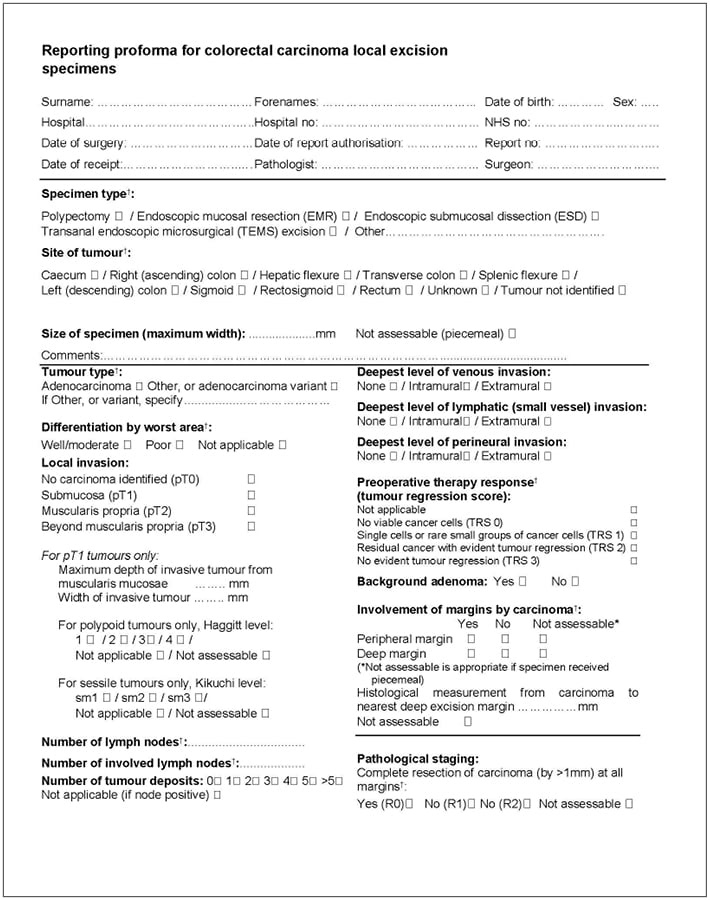
Figure 2: The RCPath dataset for reporting of local colorectal cancer excision specimens.13
Currently, the options to treat a MCRP are local excision or major surgical excision, while some institutions adopt a ‘wait and see’ protocol. Major resection includes removal of lymph nodes, which provides therapeutic and staging benefits by identifying patients that may benefit from receiving adjuvant therapy.
Conclusion
The introduction of bowel cancer screening around the world has created unique difficulties in the interpretation of polyps, with epithelial misplacement being one of the most difficult areas. The authors propose that the histopathology report should include the grade of the tumour, completeness of excision, depth of invasion in millimetres, different staging systems whenever possible, and the presence of budding with lymphatic and vascular invasion. Once all these data become available, discussion of the report among the multidisciplinary management team is strongly recommended. The Association of Coloproctology of Great Britain and Ireland (ACPGBI) prepared a position statement,22 with questions to consider should the endoscopist be faced with a suspected MCRP: ‘Can the lesion be removed endoscopically?’, and ‘Should it be removed endoscopically?’, ‘Can I remove it endoscopically?’, ‘Can I remove it in one session?’. The position statement also attempted to draw together the risk factors into a global assessment of risk of residual disease and suggested a course of action to be discussed with the patient in a chart that can be modified as more data are collected (Table 1).
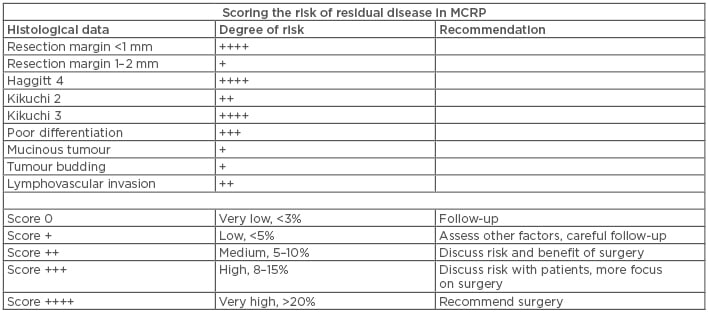
Table 1: Risk factors for residual disease and suggested management plans in patients with malignant colorectal polyps.
MCRP: malignant colorectal polyps.
Adapted from Williams et al.22








