BACKGROUND
Cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) have evolved as promising treatments for patients with peritoneal carcinomatosis. When a concomitant resection is performed, a stoma might be employed in an attempt to mitigate risk of anastomotic leakage. The primary aim of this study was to evaluate the factors regarding the decision making and outcomes of performing a stoma during CRS/HIPEC.
METHODS
An Institutional Review Board (IRB)-approved database from November 2009 to February 2018 was used to identify patients with appendiceal and colorectal cancer whose diagnosis of peritoneal carcinomatosis was suspected or confirmed. The authors divided the sample between two groups of patients: with stoma and without stoma. Comparison was made for demographics, surgical parameters, and postoperative outcomes.
RESULTS
In the study, 110 consecutive patients underwent CRS/HIPEC due to appendiceal or colorectal cancer; a stoma was performed in 32 patients (29.1%) (Table 1). Preoperative factors associated with stoma formation included rectal tumour (21.9% versus 7.7%; p=0.031), BMI <30 (81.3% versus 58.4%; p=0.023), chemotherapy (78.1% versus 57.7%; p=0.043), hypoalbuminaemia (12.5% versus 2.6%; p=0.036), and peritoneal carcinomatosis index ≥10 (59.4% versus 29.5%; p=0.002). A greater cytoreduction surgery (87.5% versus 32%; p<0.001), residual disease (50.0% versus 20.5%; p=0.002), estimated blood loss (662.5±687.4 versus 250.0±305.6; p<0.001), red blood cell transfusions (43.7% versus 11.5%; p<0.001), multiple small bowel (71.9% versus 34.6%; p<0.001), and multi-visceral resections (59.4% versus 25.6%; p<0.001) were intraoperative factors that significantly led to more stoma formation. Patients with stomas exhibited significantly higher morbidity (Clavien–Dindo class 3 and 4: 25.0% versus 7.7%, 21.9% versus 7.7%, respectively; p=0.017) and mortality (50.0% versus 20.5%; p<0.002).
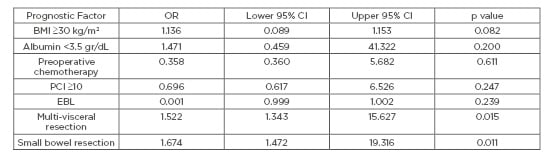
Table 1: Multivariate analysis of perioperative factors associated with stoma formation.
BMI: body mass index; CI: confidence interval; EBL: estimated blood loss; OR: odds ratio; PCI: peritoneal carcinomatosis index
CONCLUSIONS
Patients with appendiceal or colorectal cancer with higher carcinomatosis burden requiring major CRS and red blood cell transfusions are more likely to have stoma constructed. These patients with stoma could have more morbidity and mortality. However, there is a need for further evaluation of the prognostic significance of these factors, ideally in large prospective trials.








