Abstract
The authors describe a rare case of a 46-year-old woman, presenting with a 1-year history of a wasting disease and widespread mediastinal lymphadenopathy on imaging. The patient had a history of pulmonary hypertension diagnosed 7 years prior and had been treated with macitentan (an endothelin receptor antagonist) and sildenafil. Following an admission to the authors’ centre with severe anaemia and workup for suspected haematological malignancy, duodenal biopsy confirmed the diagnosis of Whipple’s disease. Interestingly, the patient did not report the cardinal symptoms of arthralgia, fevers, or gastrointestinal upset, emphasising the importance of investigating for Whipple’s disease even in the absence of these symptoms, particularly in the context of malabsorption or chronic wasting disease. Whipple’s disease can be regarded as a ‘great imitator’, often with non-specific signs and symptoms, which can present a diagnostic challenge. Following diagnosis, appropriate antibiotic therapy was commenced, and the patient made a complete clinical recovery, including resolution of pulmonary arterial hypertension, which likely was the presenting feature of this case of Whipple’s Disease, a rare phenomenon associated with this infection.
Key Points
1. The prevalence of Whipple’s disease is likely to be vastly underestimated due to the symptoms presenting a diagnostic challenge, resulting in underdiagnosis.
2. In this case report, the authors report a case of Whipple’s disease where the initial presenting symptoms occurred 7 years prior to diagnosis and imitated various other multi-system diseases.
3. Clinicians should consider investigating for Whipple’s disease even if the ‘classical’ symptoms do not appear to be present, and should maintain awareness of complications such as pulmonary arterial hypertension.
INTRODUCTION
The authors present a rare case of Whipple’s disease (WD) in a patient with a background of pulmonary hypertension and on treatment that presented with chronic wasting disease and severe anaemia. The diagnosis was unexpected as there was a strong suspicion of malignancy given the nature of the presentation and investigation findings of mediastinal lymphadenopathy. WD can be seen as a ‘great imitator’ given its multisystem presentation and is often challenging to diagnose.1 Interestingly, this case was likely associated with pulmonary arterial hypertension, which had developed years prior to diagnosis, a rare but reported complication of WD.2
CASE
A 46-year-old Caucasian woman was admitted to the authors’ centre with severe symptomatic anaemia, which had required iron replacement therapy and blood transfusions over the preceding 6 months. In addition, they reported significant weight loss (20 kg), nausea, and poor appetite for 1 year prior to presentation. The patient denied any other symptoms, including diarrhoea, skin lesions, arthralgia, fevers, or neurological disturbance.
The patient had a background of learning disability and idiopathic primary pulmonary arterial hypertension (PAH). This had been diagnosed following an episode of hospitalisation with pericardial effusion and pulmonary oedema 7 years prior to presentation and was under long-term follow-up at a regional pulmonary hypertension centre after being commenced on macitentan and sildenafil. No other causes for the PAH were found at that time.
Outpatient investigations preceding admission included a CT scan that revealed mediastinal lymphadenopathy and a possible lymphoproliferative disorder. However, a bone marrow biopsy did not confirm this diagnosis, nor did endobronchial ultrasound-guided lymph needle biopsy. Their condition progressed, and they developed ascites requiring paracentesis for symptomatic relief.
Following hospital admission, a full blood count revealed haemoglobin levels of 55 g/L (reference range: 130–175 g/L). Further blood tests showed evidence of malabsorption with red cell folate 2.5 µg/L (reference range: 3.1-20 µg/L), serum iron 2.9 µmol/L (reference range 9–30.4 µmol/L), transferrin saturation 8%, serum albumin 15 g/L (reference range: 35–52 g/L), and 25-hydroxyvitamin D 22 nmol/L (reference range: <30 nmol/L; vitamin D deficiency).
Blood pressure, respiratory rate, oxygen saturation, and temperature were normal. BMI at admission was 13.2 with a weight of 37.5 kg. Further investigations were performed to identify the cause of anaemia and look for evidence of lymphoproliferative malignancy. CT imaging of the abdomen confirmed anterior peritoneal thickening, raising concerns for peritoneal malignancy. Further diagnostic procedures performed included a gastroscopy with duodenal biopsies (Figure 1), a colonoscopy, peritoneal biopsy, and ascitic drainage. Ascitic fluid cytology revealed a population of clonal B cells by immunophenotyping. Significant clinical events during hospital admission included the development of a left lower limb deep vein thrombosis and a subdural haematoma.

Figure 1: Endoscopic image of duodenum.
Histological examination of the duodenal biopsies revealed foamy macrophages consistent with a diagnosis of Whipple’s disease (WD; Figure 2), and periodic acid-Schiff stain was positive (Figure 3). Tropheryma whippelei DNA was subsequently detected via PCR of the duodenal tissue, whole blood, and ascitic fluid samples. No features of malignancy were detected on histological examination of tissue biopsies and ascitic fluid.
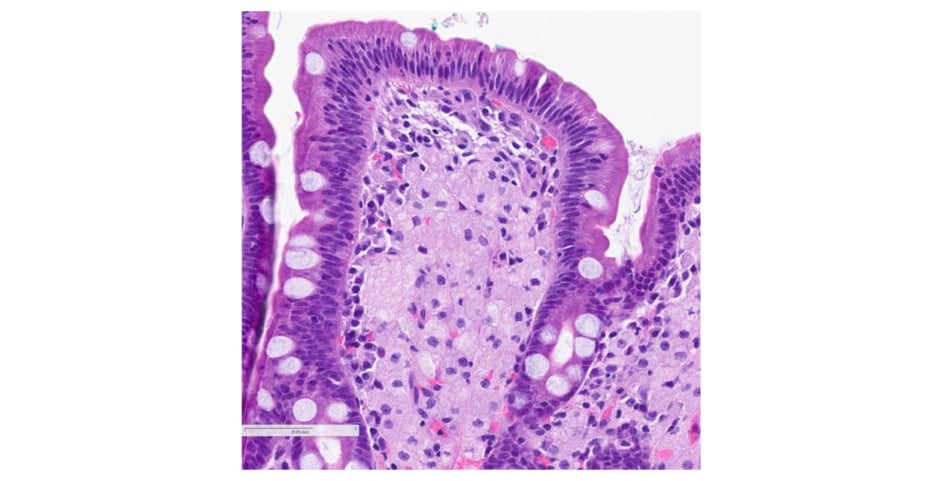
Figure 2: Haematoxylin and eosin stain of duodenal biopsy (x100).
Duodenal mucosa showing a lamina propria markedly expanded by numerous foamy macrophages.
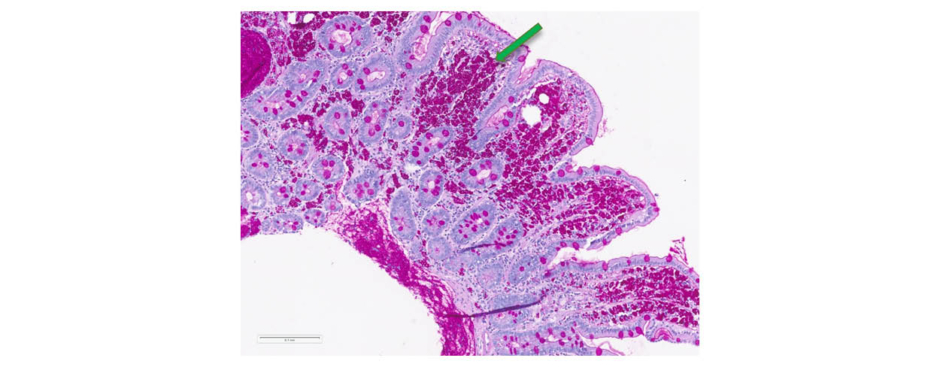
Figure 3: Periodic acid-Schiff stain of duodenal biopsy (x10).
Green arrow identifies T.whipplei bacteria.
The patient was transferred to the care of the infectious diseases team and received four weeks of intravenous ceftriaxone 2 g once a day. Cerebrospinal fluid examination was not possible due to the potential complications of concurrent subdural haematoma and anticoagulation associated with lumbar puncture; therefore, the initial phase of treatment was selected to provide cover for probable central nervous system involvement. Echocardiogram confirmed no features of infective endocarditis were present.
Inflammatory markers and haemoglobin were normalised during the 8-week admission. The patient was discharged with a follow-on regimen of oral co-trimoxazole 960 mg twice a day for 12 months. At the time of discharge, the patient’s BMI was 16.2 with a weight of 38.9 kg (with no ascites). At a 6-month follow-up appointment, the patient’s weight had increased by a further 14 kg, with no side effects of the antibiotic course and a complete clinical recovery.
DISCUSSION
WD is caused by the gram-positive bacteria T.whippelei and is characterised by progressive malabsorption, usually accompanied with gastrointestinal symptoms such as diarrhoea, abdominal pain, and weight loss, often for many years before diagnosis. It is a multisystem disorder with fever and arthralgia being cardinal symptoms in many cases.1 Anaemia and hypoalbuminaemia are often present as a manifestation of malabsorption syndrome. Lymphadenopathy can also be seen.3 Cardiac involvement is thought to be present in one-third of patients, with endocarditis an acknowledged manifestation. Pericarditis has also been reported at autopsy in up to two-thirds of cases.4
Host factors are thought to play an important role in the pathogenesis of WD. Patients with WD are thought to have impaired immune function of monocytes and macrophages, resulting in a muted inflammatory response to the organism that is carried in the gastrointestinal tract.2 Reduced expression of CD11b, the α-chain of the phagocytic receptor CR3, has been implicated in particular.2 The organism has a predilection for small-bowel macrophages; hence, duodenal biopsy with periodic acid-Schiff staining is the gold-standard method for diagnosis.1An important consideration in this case is the onset of PAH 7 years prior to the diagnosis of WD. This was treated with macitentan and sildenafil. Macitentan is an endothelin receptor antagonist approved for use for PAH. It works by occupying a pocket in the endothelin A receptor, blocking the action of endothelin-1, a potent vasoconstrictor which is found in increased levels in the plasma and pulmonary vascular endothelium of patients with PAH.5 PAH has been reported, although thought to be exceedingly rare in WD. At the completion of antibiotic treatment, clinical resolution of PAH symptoms was noted, and repeat echocardiogram revealed no evidence of PAH. It is likely that this was the initial presentation of WD given the apparent reversal of PAH with targeted antibiotic treatment. The pathophysiology of WD-PAH is poorly understood; however, evidence of bacterial invasion of the tunica media has been reported on histological examination, which may play a role in vascular resistance.6,7 Following the resolution of PAH with WD treatment, sildenafil and macitentan were gradually stopped with careful monitoring for recurrence.
The time to diagnosis from symptom onset in this case was approximately 18 months. WD is regarded as a rare diagnosis; however, the exact prevalence is unknown. One European epidemiological study estimated a prevalence of three in one million.8 The diagnosis can be challenging owing to the variety of clinical signs and symptoms that can mimic other systemic disorders, in particular malignancy, as in this case. This can result in a considerable delay between presentation and diagnosis. This case demonstrates the importance of considering investigating for WD in patients who present with evidence of severe systemic inflammation, anaemia, or malabsorption of chronic duration, even if the cardinal symptoms of arthralgia, fever, or diarrhoea are not reported.
The authors believe that this is the first reported case of WD with initial presentation of pulmonary arterial hypertension years prior to WD diagnosis.
Patient Perspective
I have found taking antibiotics for a long time very hard. I feel very happy the treatment has worked, and I feel normal again. My family said I am much better and have put on weight. I am glad my life is back to normal again.
Evidence of Patient-Informed Consent
The authors obtained written, informed consent from the patient to publish the case report and any accompanying images prior to publication.







