Abstract
The optimal dressing is still unclear, despite hypospadias being one of the most prevalent surgical operations. Children’s dressing for hypospadias surgery was searched on PubMed as “dressing for hypospadias,” “postoperative dressing for pediatric hypospadias,” and “dressing AND hypospadias.” Experimental studies, animal studies, reviews, letters, and repetitive publications were excluded from the study. By evaluating these reviewed publications, factors affecting hypospadias dressing, such as surgeon, country, dressing type, characteristics, and why it is preferred, will be revealed. As a result, 17 articles were examined, and the advantages of each were established by examining the results. The type of hypospadias, the surgeon’s choice, and its ease of removal stand out as the crucial factors in treating hypospadias in children, along with the degree of development of the nation.
Key Points
1. There are thousands of retrospective, randomised, prospective case reports and systematic reviews in the literature comparing hypospadias surgery types, suture use, anaesthesia types, and complications. However, there are very few publications on dressing after hypospadias surgery in the post-operative period. Wrapping the penis with sterile gauze with antibiotic cream and fixing it with a plaster is the most used conventional method, and it is not often mentioned in the publications.
2. The optimal dressing is still unclear, despite hypospadias being one of the most prevalent surgical operations. Which factors affect hypospadias dressing, such as surgeon, country, dressing type, characteristics, and why it is preferred will be revealed in this study.
3. It is clear that, despite the fact that the removal of the dressing following a hypospadias surgery is quick and painless, it is still not the optimum dressing type that will satisfy the demands of both children and surgeons. The type of the dressing following a hypospadias surgery, the surgeon’s choice, and its ease of removal stand out as the crucial factors in treating hypospadias in children, along with the degree of development of the nation.
INTRODUCTION
One of the most typical congenital abnormalities found in males is hypospadias.1 Between 150–300 live babies are known to have hypospadias. The typical trio of a hooded prepuce, a ventrally advanced urethral meatus, and a ventral penile curvature indicating a stop in penile development serves as the diagnosis. Primary hypospadias repair aims to rectify penile curvature, advance the urethral meatus to allow adequate urine and sperm flow through the glans, and create an aesthetically beautiful penis. Local skin flaps, preputial and extragenital tissue grafts/flaps, and urethral tubularisation are three general categories for the repair approaches. Hypospadias repair is one of the most common surgeries performed by paediatric urologists, with over 300 types of surgery described.1,2 There are thousands of retrospective, randomised, prospective case reports and systematic reviews in the literature comparing hypospadias surgery types, suture use, anaesthesia types, and complications. However, there are very few publications on dressing after hypospadias surgery in the post-operative period. Wrapping the penis with sterile gauze with antibiotic cream, and fixing it with a plaster is the most used conventional method, and it is not often mentioned in the publications.3-8
The aim of this study is to reveal the factors affecting the hypospadias dressing in the accompaniment of the evaluated articles.
MATERIALS AND METHODS
The number of papers published on this subject was relatively low before 2000; their number is, however, gradually increasing today. Children’s dressing for hypospadias surgery was searched on PubMed as “dressing for hypospadias,” “postoperative dressing for pediatric hypospadias,” and “dressing AND hypospadias.” Experimental studies, animal studies, reviews, letters, and repetitive publications were excluded from the study. By evaluating these reviewed publications, factors affecting hypospadias dressing, such as surgeon, country, dressing type, characteristics, and why it is preferred will be revealed.
RESULTS
Seventeen studies meeting the above criteria were reviewed.3-19 By examining these studies, dressing types, their properties, and why they were preferred was revealed. In general, it has been seen that these publications are mostly made from developed or developing countries, and plastic surgeons and urologists mostly use commercialised dressing materials for dressing after hypospadias surgery. It is presented as an advantage that the dressing can disappear, or be easily removed, especially by itself. However, in underdeveloped countries, or in rural areas of developing countries, the simplest and cheapest sterile gauze with antibiotic cream is used. Recently, it has become popular to add substances that increase wound healing to dressing materials. In published articles about dressing after hypospadias surgery, the advantages of the preferred dressing, the reason for preference, country, and characteristics of the surgeon are shown in Table 1.
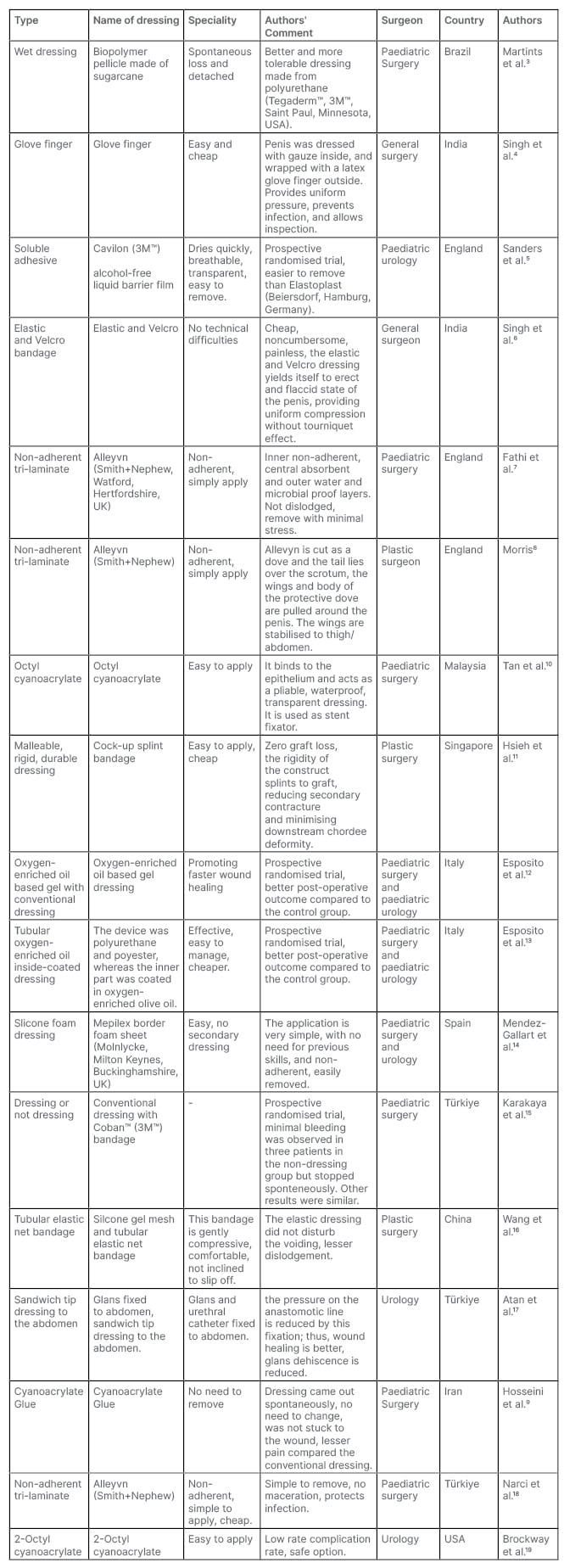
Table 1: Dressing type and characteristics for hypospadias surgery.
DISCUSSION
Although one of the most performed operations by paediatric surgeons and urologists, the scarcity of reports on wound dressing in hypospadias could be related to the surgeons’ consideration on the sufficiency of conventional dressing methods. Furthermore, studies on appropriate wound dressing for these cases are either controversial or absent. Multiple dressing types and materials have been defined. These materials include silastic foam, elastic bandage, glove finger, Tegaderm™ (3M™, Saint Paul, Minnesota, USA), Opsite (Smith+Nephew, Watford, Hertfordshire, UK), Cavi-care (Smith+Nephew), silicon foam sheet, topical ozone, and superglue. Related reports have focused on ease of removal or biodegradable, self-eliminating materials in paediatric patients.3,5,6,12-14
The ideal dressing should be flexible and adaptable to the penis during a child’s movements, while also being rigid to stabilise the penis during the dynamic changes occurring in physiological erections. It should also be affordable, straightforward, dependable, stable, snug-fitting, transparent, waterproof, non-adherent, and nonallergenic. Additionally, it should avoid faecal and urine contamination of the penis, which continually happens in infants under the age of 2–3 years old who wear diapers. The dressing should also guard against external wounds caused by children’s frequent scratching of the penis throughout the healing process. Even more care is required in the dressing of patients undergoing preputioplasty and urethroplasty surgery. It should also allow for simple maintenance examination, accommodate both the erect and flaccid phases of the penis, and provide modest compression throughout. In addition to preventing haematoma development, leaking, or infection, it should improve tissue adhesion, oedema resolution, and wound healing. It should not contain any adhesives, sutures, casts, or allergic materials, and it should not restrict the patient’s mobility, or create ischaemia or a tourniquet effect. Finally, the optimal dressing should be simple to apply and remove without any pain.3-19
There is no hypospadias surgery dressing closure technique that satisfies all ideal requirements, according to a review of 17 papers. Applications that are self-disappearing, transparent, and unclothed have been found to be more effective, particularly in cases of distal hypospadias.3,5,9,10,15,19 For example, applying octyl cyanoacrylate to challenging hypospadias shapes is simple. It is a powerful urethral stent fixator and the best dressing for hypospadias surgery, because it forms a strong, watertight adhesive bond that separates from epithelial surfaces in 7–10 days.8 Due to their low cost and accessibility, gloves with fingers, elastic and velcro, tubular net elastic bandages, and Alleyvn (Smith+Nephew) bandages are utilised in several developed and developing nations.4,6-8,16,18 With its inner non-adherent, central absorbent, and outside water- and microbial-proof layers, Alleyvn, a hydrocellular foam, has a distinctive tri-laminate structure. In 83 children, most of whom underwent hypospaias surgery, and were dressed with Alleyyn, premature dressing removal was not observed in any patient. On the ward, all dressings were removed with little discomfort to the patients. No early wound infection occurred. This tri-laminate dressing is non-adherent, easy to use, and suitable for hospital early discharge.The authors have used Alleyvn dressing following hypospadias surgery “in the shape of a dove,” the tail lying over the scrotum, and the wings lying on either side of the penis.7,8 The traditional dressing used following hyposdias surgery may not offer homogeneous compression, and a watertight barrier against outside infection-contamination. Due to its instability over the sensitive organ, the dressing may potentially come off following surgery. When dressing a child’s penis, which has a smaller penile girth and length, it is simple to use a gloved finger because it is inexpensive, widely accessible, easy to use, uniformly presses the penis, and makes it possible to inspect the wet dressing with ease. While the authors do not recommend glove finger dressing for scrotal and perineal hypospadias surgery, they state that removing this dressing is easy and painless (Figure 1).4 Due to its elasticity, the tubular elastic net bandage is able to create a little compression and perfectly fits the penis shaft. The wound could be examined through the dressing since the tubular net bandage is a network. The authors stated that dressing gauze is not suitable for the erect and flaccid phases of the penis, and that the dressings slip off in nearly half of cases, and do not provide uniform compression. They stated that this tubular elastic net bandage was well tolerated in children, while providing comfortable and gentle compression, and did not affect normal voiding, even after removal of the urethral catheter.16 It is debatable whether pressure should be used during the dressing after hypospadias correction. Lack of pressure can result in haematoma, oedema, and infection, which increases the likelihood of problems, while excessive pressure can impair the flap and skin’s blood supply, and cause tissue necrosis. According to the authors, a dressing is necessary to manage post-operative oedema, avoid haematoma development, which increases the risk of infection, and act as a barrier from the environment, particularly in developing nations, where ward cleanliness and hygiene may not be the best. To avoid problems, and provide appropriate compression, particularly in cases of severe hypospadias, several authors have employed specialised dressing materials or dressings.11,14,17 Hypospadias surgery significantly benefits from the use of a self-adherent, gentle silicone-foam dressing that reduces unpleasant removal.The Mepilex Border foam sheet (Molnlycke, Milton Keynes, Buckinghamshire, UK) is cut to match the length and circumference of the penis. The dressing’s lower border is divided into three flaps, allowing self-adhesion to the pubic and scrotal region. To cover the penis, the foam dressing must be rolled into a cylinder, wrapped around it, and sealed on the dorsal side with an adhesive lateral border. In order to observe the colour of the glans and pass the urine catheter through the dressing during the post-operative period, the top of the dressing must be left open. No further dressings are required. This dressing is simple to apply, does not prolong operating time, and removal does not cause anxiety for the child or family. It is easily removed without any analgesics.14 For wound healing and infection, some authors employed dressing materials containing ozone and comparable substances.7,12,13 Because it was stable and maintained the penis straight, while having a lower incidence and shorter duration of post-operative swelling than the conventional dressing, as described in Esposito et al.’s study,13 this innovative device seemed to satisfy all the requirements of an ideal hypospadias dressing. They used a tubular finger oxygen enriched oil inside coated dressing device for wound closure after distal hypospadias surgery. This device was a mechanical barrier that was effective through two mechanisms: firstly, the device’s exterior, which was not impregnated, was moderately water-repellent and protected the penis from contamination by urine and faeces, as well as traumatic injuries brought on by the child scratching the area where the wound had been, as in their experience. Secondly, a microenvironment that was adverse to the growth of the pathogens usually seen on skin lesions was established by the interior half of the device, which was coated with oxygen-enriched greasy gel. This allowed the microcirculation to be activated. The reduction of microbial infection, the debridement effect, the control of the inflammatory phase, the stimulation of angiogenesis, as well as biological and biochemical processes that favour oxygen metabolism increasing wound healing are all associated with the favourable effects of ozone on wound healing. It serves as an insulator, generating heat that speeds up the healing process by increasing local peripheral vasodilation, blood flow, oxygenation, and cellular metabolism. They also stated that this device is cheap, easy to apply, and has fewer skin and urethral complications compared to other applications13 (Table 1).
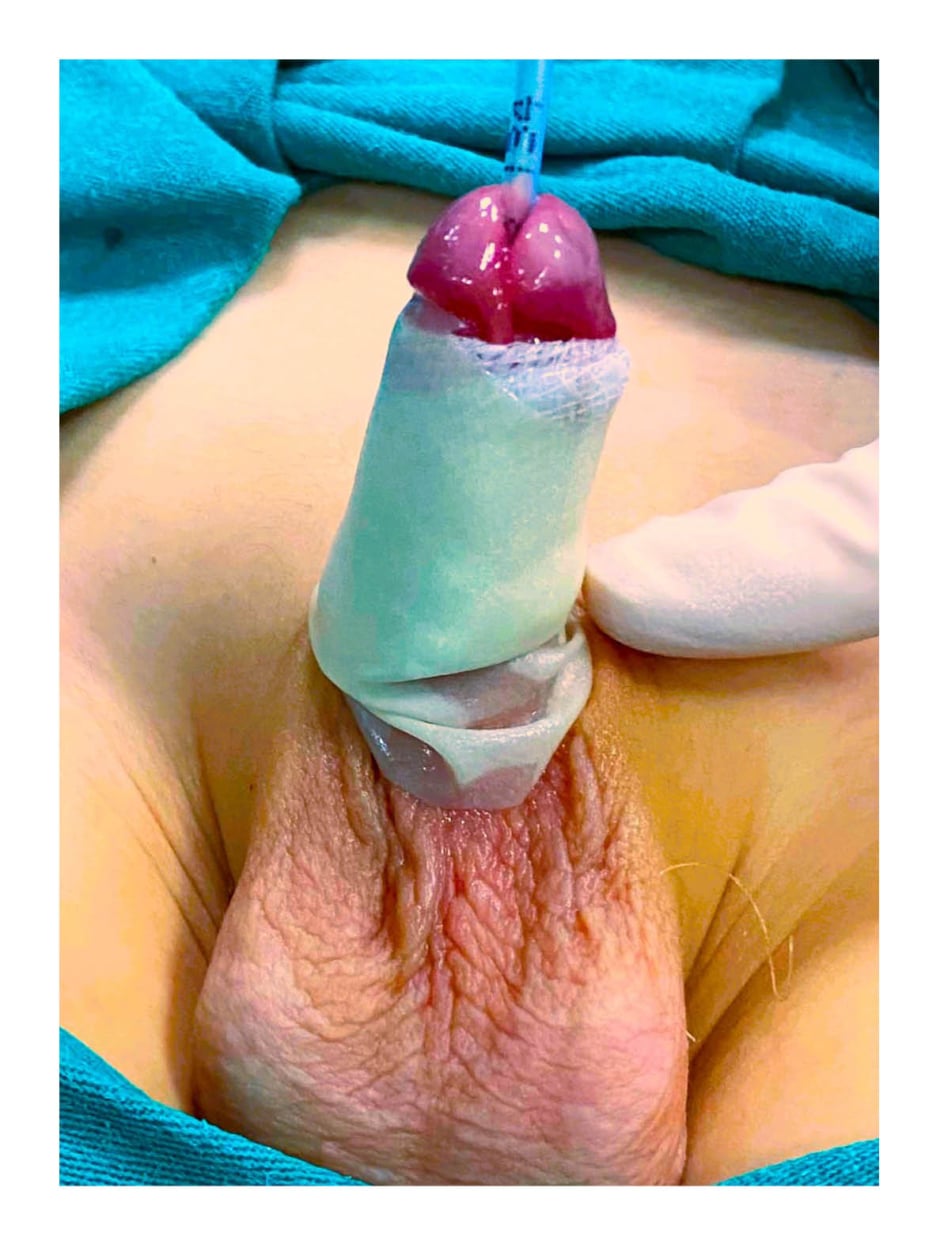
Figure 1: Photographed form of glove finger dressing for hypospadias surgery.4
The patient’s consent was obtained from his parents for this image to be used in publications.
In light of the information previously provided, it is clear that, despite the fact that the removal of the dressing following a hypospadias surgery is quick and painless, it is still not the optimum dressing type that will satisfy the demands of both children and surgeons. While dressing after hypospadias surgery in developing countries is generally done in the cheapest and simplest way with sterile gauze with antibiotic cream (Figure 2), dressing materials are becoming more commercialised, even if the surgeon is a plastic surgeon. In fact, depending on whether the centre where the hospital is located is metropolitan, and in developing or underdeveloped countries, more expensive or commercial products may be preferred.
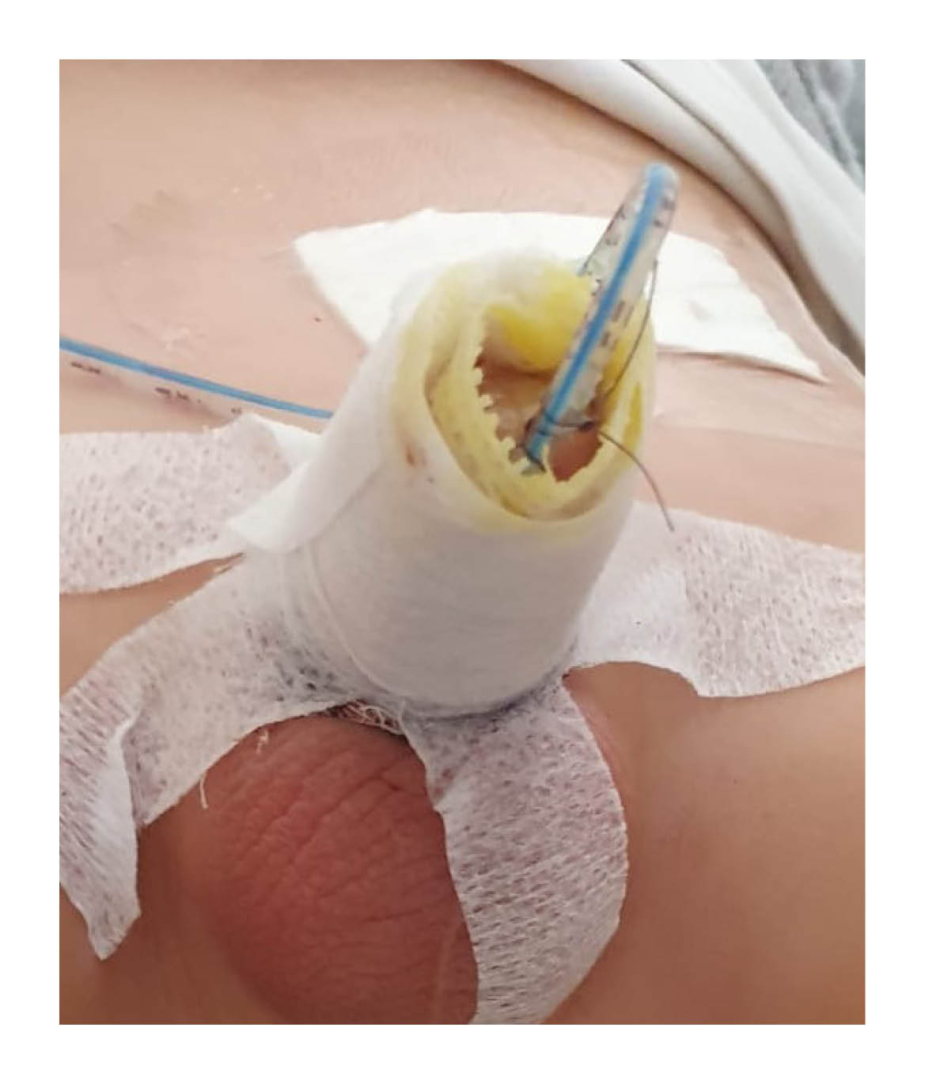
Figure 2: Standard closure technique with sterile gauze with antibiotic cream.
The patient’s consent was obtained from his parents for this image to be used in publications.
The type of dressing used following a hypospadias surgery, the surgeon’s choice, and its ease of removal, stand out as the crucial factors in treating hypospadias in children, along with the degree of development of the nation.







