Abstract
Objectives: This study aimed to investigate the association between the extent of focal extracapillary proliferation and the likelihood of achieving complete remission at 24 months in patients with lupus nephritis (LN).
Methods: A retrospective observational analysis was conducted on 124 patients with proliferative focal and diffuse LN. Patients were categorised into subgroups based on the extent of extracapillary involvement (Group 1: 5–24% crescents, Group 2: 25–50% crescents, Group 3: >50% crescents, and control group without extracapillary involvement). The primary outcome was the rate of achieving complete remission at 24 months, defined according to the 2021 Kidney Disease: Improving Global Outcomes (KDIGO) standards. Statistical analyses were performed using logistic regression.
Results: A total of 107 women and 17 men participated, with mean ages of 35±10 years and 34±12 years in the study and control groups, respectively. The control group exhibited a significantly higher rate of complete remission compared to the subgroups with extracapillary proliferation. Specifically, Group 1 had an odds ratio of 7.2, (95% CI: 2.3–20.2) and a p-value of 0.001, indicating a lower probability of achieving remission.
Conclusions: The presence of focal extracapillary proliferation in patients with LN was associated with a decreased likelihood of achieving complete remission at 24 months. This finding emphasises the importance of considering the extent of extracapillary proliferation in predicting treatment outcomes for LN.
Key Points
1. This study investigated the association between the extent of focal extracapillary proliferation and the likelihood of achieving complete remission at 24 months in patients with lupus nephritis.2. Patients with extracapillary involvement greater than 5% had higher proteinuria levels and reduced likelihood of achieving remission compared to those without crescents.
3. The study highlights the importance of assessing the extent of extracapillary proliferation as a critical prognostic factor in determining lupus nephritis outcomes.
INTRODUCTION
Proliferative lupus nephritis (LN) with focal extracapillary proliferation (FEP) is a common finding in renal biopsies of patients with LN, but little is known about its progression.1 It is well established that patients with more than 50% of glomeruli showing crescents, a condition known as diffuse extracapillary proliferation (DEP), have a worse prognosis.2 However, there is limited published data on the remission rate in patients with LN Class III-IV with FEP (involving less than 50% of affected glomeruli).
Despite improvements in immunosuppressive therapies, approximately 25–35% of patients with proliferative LN progress to end-stage renal disease requiring renal replacement therapy.3 Therefore, early diagnosis; a comprehensive understanding of clinical, demographic, and histological patterns in each patient; and identifying factors influencing the disease’s progression are crucial. The presence of crescents in more than 50% of glomeruli in a renal biopsy indicates a poor prognosis,4 but there are few reports on the evolution of patients with FEP.5 Moreover, it remains uncertain whether this condition affects the patients’ outcomes and prognosis.
It is important to mention that there is little or no data on the Hispanic population that identifies or characterises the renal biopsies of patients with LN, and the presence of extracapillary involvement, and also performs a statistical analysis as a predictor of non-response to current biological therapies, such as for anti-CD20. The data that have been extrapolated have been obtained from studies in the Asian population, where extracapillary involvement is clearly a determining predictor in the evolution and remission of the disease.
This study is based on pathology records taken from nephrology departments in only medical centres that have a high level of complexity in the countries Argentina, Colombia, Ecuador, and Bolivia. A retrospective analysis of renal biopsies was conducted from a cohort of 124 patients with proliferative LN, either focal or diffuse. The parameters analysed were demographic characteristics, disease progression, and their correlation with clinical and laboratory parameters comparing two groups with FEP (based on its magnitude) with DEP and a control group (Class III and IV LN without crescents). Table 1 displays some of these demographic characteristics: age at presentation, gender, presence of hypertension, and duration of symptoms until the time of biopsy.
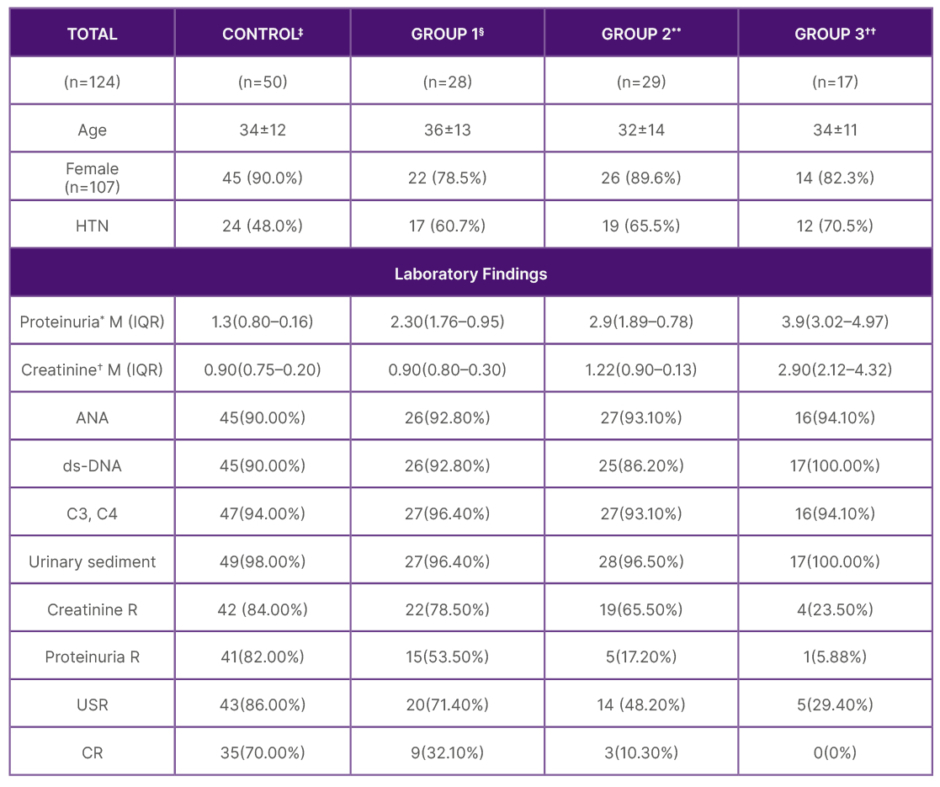
Table 1: Sociodemographic characteristics and laboratory findings of patients with lupus nephritis.
*Proteinuria expressed in g/24 hours
?Creatinine expressed in mg/dL, M, and interquartile range
‡Control group: focal or diffuse proliferative lupus nephritis without extracapillary involvement
§Group 1: 5–25% crescents
**Group 2: 25–50%
??Group 3: >50% crescents
The data is divided into a control group and three study groups based on the extent of extracapillary proliferation: Group 1 with 5–25% crescents, Group 2 with 25–50% crescents, and Group 3 with more than 50% crescents. Key characteristics such as age, gender distribution, and the prevalence of hypertension are listed alongside various laboratory findings including proteinuria, creatinine levels, ANA positivity, ds-DNA positivity, C3 and C4 levels, and urinary sediment abnormalities.
ANA: antinuclear antibodies; CR: complete regression; ds-DNA: double-stranded DNA; HTN: hypertension; IQR; interquartile range; M: mean; R: regression; SD: standard deviation expressed in absolute number and percentage; USR: urinary sediment.
METHODS
The term crescent is used to describe a lesion characterised by extracapillary hypercellularity, composed of a variable mixture of cells. Some crescents may consist predominantly of epithelial cells, while others mainly comprise monocytes and/or macrophages (Figure 1).
To distinguish crescents from the apposition of hypertrophied visceral and parietal single layers, crescents must be composed of two or more layers of cells in Bowman’s space. The International Society of Nephrology (ISN) and Renal Pathology Society (RPS) criteria define a crescent as involving 25% or more of the glomerular capsule’s circumference.8 However, in this study, it was considered a threshold of 10% or more, based on evidence from the Oxford classification of IgA nephropathy,6 considering extracapillary proliferation of more than 5%. This decision was made because not only the extension but also the pathogenic mechanism of extracapillary proliferation likely plays a significant role in the patient’s progression.
Clinical and pathological characteristics of renal biopsies from 124 patients with proliferative focal and diffuse LN who met the inclusion criteria were analysed.
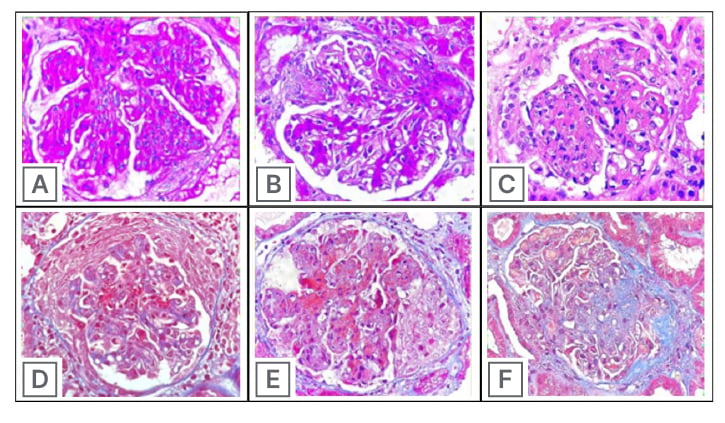
Figure 1: Glomerular lesions.
PAS staining of A) endocapillary hypercellularity; B) mesangial hypercellularity and segmental sclerosis; C) karyorrhexis (HE stains), masson trichrome staining; D) cellular crescent; E) Fibrinoid necrosis and cellular crescent; and F) Segmental sclerosis.
HE: Haematoxylin and eosin stain; PAS: periodic acid–Schiff.
Inclusion Criteria
- Diagnosis of systemic lupus erythematosus according to the 1982 American College of Rheumatology (ACR) criteria;7
- renal biopsies showing focal lupus nephritis Class III and diffuse lupus nephritis Class IV, based on the ISN and RPS classification from 2003; and8
- similar induction and maintenance treatment.
Exclusion Criteria
- Heterogeneity in treatments: patients who received different induction or maintenance treatments were excluded to maintain treatment uniformity;
- follow-up period of less than 24 months; and
- renal biopsy not processed by nephropathologists: this was considered to ensure the accuracy of histological assessment.
Data Collection
Data were collected from medical records, including demographic characteristics (age, gender, presence of hypertension), clinical presentation, laboratory findings (proteinuria, creatinine levels, antinuclear antibodies, ds-DNA, C3, C4 levels, urinary sediment analysis), and treatment details. Renal biopsies were evaluated for the presence and extent of extracapillary proliferation.
Renal Pathology
Patients underwent a renal biopsy at the time of LN diagnosis and were classified according to the 2003 ISN/RPS criteria for LN.8 Activity index and chronicity index were calculated following the Austin criteria.9
Complete remission was considered when:
- urinary sediment was inactive (defined as less than five dysmorphic red blood cells per high-power field 40X and the absence of RBC casts);
- proteinuria was less than 500 mg in 24 hours; and
- evidence of serological inactivity (defined as the normalisation of complement factors C3, C4, CH50, and anti-DNA).
Statistical Analysis
Out of the 220 renal biopsies with proliferative focal or diffuse LN initially analysed, 96 were excluded due to lack of follow-up until 24 months or heterogeneity in induction and maintenance treatment, leaving a total of 124 histological samples.
The normality of variables was determined using the Kolmogorov-Smirnov test. The Kruskal-Wallis test with Bonferroni post hoc analysis was performed. The chi-square test was used for categorical variables, with post hoc analysis using standardised residuals. Univariate logistic regression analysis was conducted to determine complete remission of LN, calculating odds ratios (OR) and 95% CI. Dummy variables were encoded for categorical variables and incorporated into the logistic regression. Multivariate analysis was performed for statistically significant variables. A p-value of <0.05 was considered statistically significant, and data were presented as means and standard deviation.
RESULTS
A total of 124 patients diagnosed with Class III or IV+V LN from multiple Latin American countries were included in this retrospective observational analysis. The majority of participants were female (107/124, 86.2%) with a mean age of 35±10 years (Table 1). The control group consisted of 50 patients with LN Class III and IV, without extracapillary involvement. Patients were further categorised based on the extent of extracapillary involvement into Group 1 (5–24% crescents, n=28), Group 2 (25–50% crescents, n=29), and Group 3 (>50% crescents, n=17), or control group without extracapillary involvement.
Baseline Characteristics
Sociodemographic characteristics including age, gender, and hypertension prevalence were compared among the control group and the three extracapillary involvement subgroups. Laboratory findings, including proteinuria, creatinine levels, antinuclear antibodies, ds-DNA, C3, C4 levels, and urinary sediment analysis, were analysed for the different patient groups (Table 1).
Primary Outcome Assessment
The primary outcome of achieving complete remission at 24 months was assessed based on the 2021 Kidney Disease: Improving Global Outcomes (KDIGO) standards. Univariate analysis revealed a significantly higher rate of complete remission in the control group compared to patients with extracapillary involvement. The control group had an OR of 0.04 (95% CI: 0.11–0.31), p=0.001 (Table 2), indicating a lower probability of complete remission for patients with extracapillary proliferation.
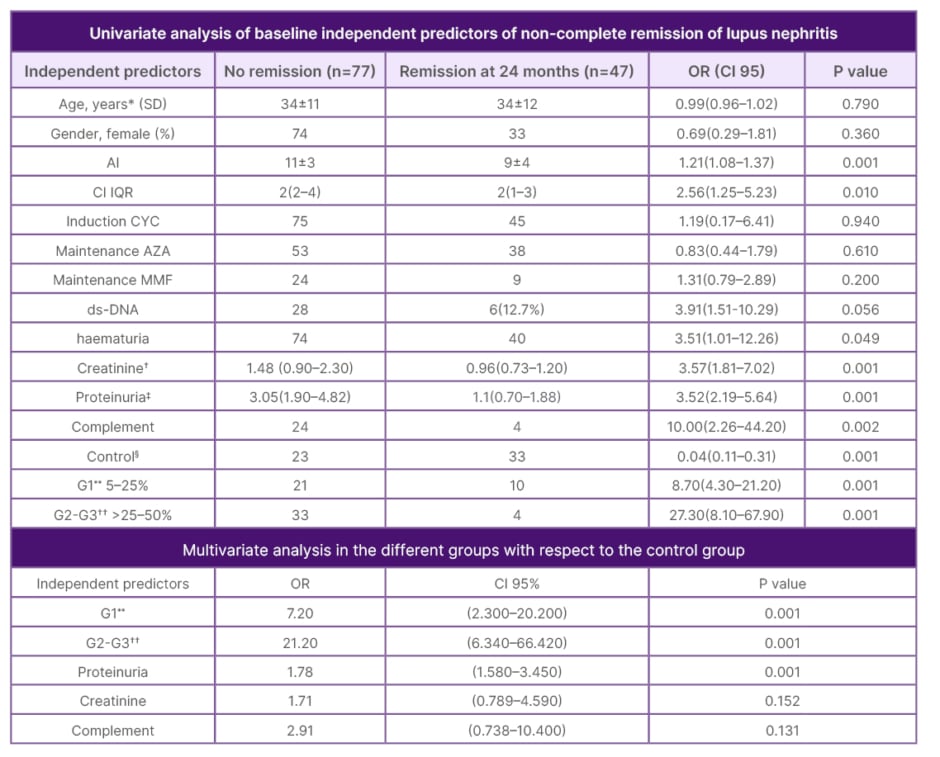
Table 2: Combined analysis of independent predictors for non-complete remission in lupus nephritis at 2 years.
*Age expressed with SD and IQR
?Creatinine expressed in mg/dL
‡Proteinuria expressed in gr/L
§Control: Lupus nephritis class III-IV without extra capillary involvement
**G1: crescents 5–25%
??G2-G3: crescents 25–50%
This table presents both univariate and multivariate analyses of baseline independent predictors for non-complete remission in 124 patients with lupus nephritis over a period of 2 years. The univariate analysis compares patients who did not achieve remission with those who did, highlighting factors such as age, gender, activity index (AI), chronicity index (CI), ds-DNA positivity, haematuria, creatinine levels, proteinuria, and low complement levels.
The multivariate analysis focuses on the relationship between different patient groups and the likelihood of non-complete remission, with particular emphasis on the extent of extracapillary proliferation. It shows that higher levels of crescents (both Group 1 and Group 2–3) and increased proteinuria are significant predictors of non-complete remission.
AI: activity index; AZA: azathioprine; CI: confidential interval; CYC: cyclophosphamide; ds-DNA: double-stranded DNA; IQR: interquartile range; MMF: mycophenolate mofetil; OR: odds ratio; SD: standard deviation.
Association of Extent of Extracapillary Proliferation with Remission
Patients presenting with crescents or extracapillary involvement ranging from 5–25% demonstrated a 7.2 times lower probability of achieving complete remission at 24 months (OR: 7.2; 95% CI: 2.3–20.2; p=0.001). Similarly, patients with >25–50% crescents (Group 2) and >50% crescents (Group 3) had substantially lower probabilities of achieving remission (OR: 21.2; 95% CI: 6.34–66.42; p=0.001) (Table 2).
Multivariate Analysis
A multivariate analysis was performed to evaluate the independent predictors of not achieving complete remission. The extent of extracapillary proliferation remained a significant predictor, with Group 1 having an OR of 7.2 (95% CI: 2.3–20.2; p=0.001) and Group 2 and 3 having an OR of 21.2 (95% CI: 6.34–66.42; p=0.001).
DISCUSSION
The analysis of data from 124 patients with proliferative focal and diffuse LN in various Latin American countries, considering racial differences and a 24-month follow-up, revealed significant findings. Patients with extracapillary involvement greater than 5% demonstrated higher levels of proteinuria and a reduced likelihood of achieving remission compared to patients without evidence of crescents in renal histology (Table 2). The most prevalent clinical presentation was microhaematuria, and the extent of extracapillary involvement correlated with greater renal dysfunction and higher proteinuria levels. Regarding remission outcomes, no significant differences were observed in chronicity indices between the group that achieved remission and the group that did not. However, there were notable differences in activity indices, particularly concerning the achievement of complete remission at 1 year. Patients with lower activity indices exhibited a higher frequency of remission (Table 2).
Glomerular crescents serve as a histopathological indicator of severe renal injury, characterised by the disruption of the glomerular capillary wall, resulting in the accumulation of macrophages and T cells in Bowman’s space, along with damage to the glomerular capsule’s parietal cells.10,11 It is generally assumed that a higher percentage of crescent formation in glomeruli correlates with more severe clinical and pathological manifestations.12 This study’s findings support this assumption, as patients with higher extracapillary involvement exhibited more pronounced renal insufficiency and greater proteinuria compared to the control group. Although there were no significant differences in the age of patients, blood pressure levels were more frequently elevated in Groups 2 and 3. Additionally, glomerular microhaematuria was present in all groups.
Patients presenting with crescents or extracapillary involvement of more than 5% demonstrated a substantially reduced likelihood of achieving complete remission at 24 months, as indicated by a 7.2 times lower probability (Table 2). Conversely, patients without histological evidence of extracapillary proliferation had a statistically significant 70% chance of achieving complete remission at 2 years (Figure 2).
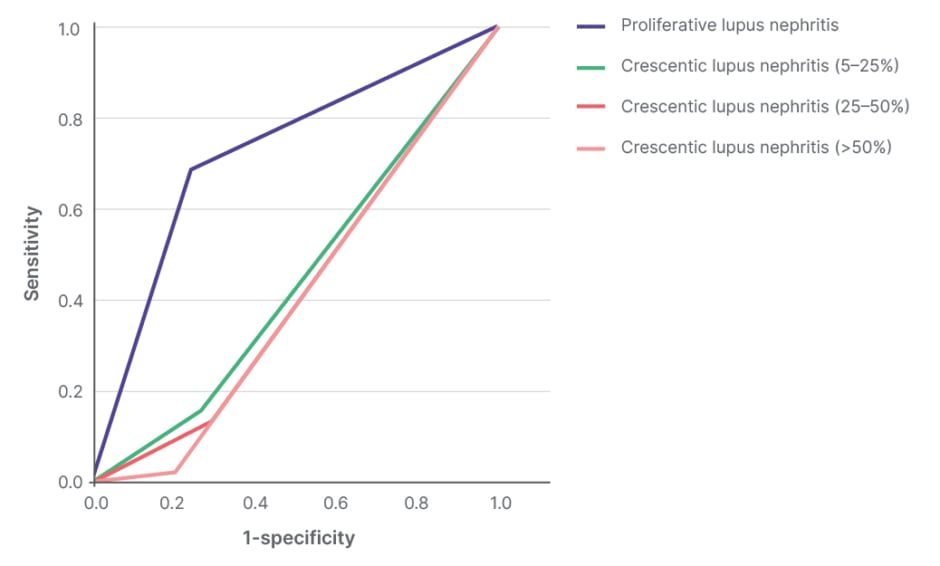
Figure 2: Receiver operating characteristic curve lupus nephritis.
Prediction of remission at 24 months of proliferative lupus nephritis without extracapillary involvement (crescents) after a specific treatment is 70% p-value 0.01, while if the patient has crescents regardless of the extension the probability of remission at 24 months is less than 50%.
These observations emphasise the significance of evaluating extracapillary involvement in glomerular crescents as a critical prognostic factor in determining disease outcomes and response to treatment in patients with proliferative focal and diffuse LN.
The formation of glomerular crescents in LN is indeed common, and previous studies have shown a significant prevalence. In a cohort of 62 patients with rapidly progressive glomerulonephritis, 50% of them were found to have LN.13 In this current study, it was also observed that a considerable proportion of patients, more than 50%, showed extracapillary involvement of more than 5%, indicating the substantial impact of crescent formation in this cohort.14
It is crucial to emphasise that the crescent score was incorporated, which includes C0 (no crescents), C1 (crescents in less than 25% of glomeruli), and C2 (crescents in at least 25% of glomeruli), into the mesangial hypercellularity, endocapillary hypercellularity, segmental glomerulosclerosis, and tubular atrophy/interstitial fibrosis (MEST) score of the Oxford classification of IgA nephropathy.15 This addition was based on robust data and evidence derived from multicentre studies,16 ensuring the comprehensive and accurate assessment of renal histology in this investigation.
By including the crescent score, the authors aimed to enhance the precision of this evaluation and provide a more thorough analysis of the renal pathology in patients with proliferative focal and diffuse LN, considering the extent of crescent formation as an important prognostic factor.
These findings strongly indicate that the presence of extracapillary proliferation of more than 5% in glomeruli independently predicts a failure to achieve complete remission at 24 months with statistical significance. This suggests that not only the extent of the damage but also the pathogenic mechanism of extracapillary lesions may play a crucial role in determining disease outcomes. To establish the validity of this assertion, further prospective studies are necessary.
Severe kidney involvement at diagnosis is a key risk factor for poor remission in patients with LN. Regarding the paediatric population, a recent study developed by De Mutiis C. et al.17 in a cohort of 382 patients with LN Class ≥III evaluated variables such as clinical presentation, treatment, and 24-month kidney outcomes. The study concluded that severe kidney involvement at diagnosis is a key risk factor for poor remission as LN Class III patients had a higher rate of complete remission compared to Classes IV or V.17
To the authors’ knowledge, this is the first study that evaluates the association between the extent of FEP and the likelihood of achieving complete remission at 24 months in patients with LN. However, it is worth mentioning other studies that have demonstrated specific associations among Latin American patients with LN and their outcomes.
Vinicki J. et al.18 conducted a retrospective study to evaluate treatment response in patients with proliferative and membranous LN in a cohort of 37 Latin American patients with a follow-up of 10 years. It was demonstrated that just 19% of patients could achieve complete remission after induction therapy and 30% after maintenance therapy.
In 2023, Rodelo J. et al.19 assessed the prognostic value of other pathological features such as interstitial fibrosis, tubular atrophy, and tubulointerstitial inflammation in 285 Latin American patients with LN. Moderate-to-severe interstitial fibrosis and tubular atrophy were found in 34.7% of biopsies and were linked to poorer kidney survival compared to mild or no severe interstitial fibrosis and tubular atrophy (p=0.018).19 Furthermore, patients with fibrous crescents experienced significantly worse kidney outcomes.
These studies underscore the unique challenges faced by Latin American patients with LN, highlighting lower rates of complete remission and worse kidney outcomes.
LIMITATIONS
It is essential to acknowledge the limitations of this study. First, the study design is retrospective and observational in nature, which may introduce inherent biases and limitations in the interpretation of the results. Secondly, evaluating the interobserver and intraobserver reproducibility of the anatomopathological diagnosis is necessary to ensure the reliability and consistency of the findings. Lastly, in this study, only complete remission was evaluated, and different degrees of partial remission were not analysed, which may provide further insights into treatment responses and disease progression.
Despite these limitations, this study provides valuable insights into the relationship between extracapillary proliferation and remission outcomes in patients with proliferative, focal, and diffuse LN. Further research and well-designed prospective studies are warranted to confirm and expand upon these findings, which could potentially lead to more targeted and effective therapeutic approaches for this challenging condition.
CONCLUSION
In conclusion, the presence of glomerular crescents or extracapillary proliferation is a clinically relevant finding and is not uncommon in patients with LN. This study’s proposed cutoff point of extracapillary proliferation of more than 5% is of particular significance, as it indicates that patients with this extent of involvement had a substantially reduced likelihood of achieving complete remission, with a 6.8 times lower probability. This finding has crucial implications for therapeutic decisions, particularly in Hispanic patients, where the presentation of this pathology can be more aggressive.20,21
These results strongly suggest that not only the extent of the damage but also the pathogenic mechanism of extracapillary lesions play a pivotal role in determining disease outcomes. Further prospective studies are essential to validate and expand upon these findings, which could potentially lead to more targeted and effective therapeutic approaches for patients with proliferative, focal, and diffuse LN.







