Interviewees: Wolfgang Popp,1 Klara Szondy2
1. Döbling Doctor’s Center, Privatklinik Döbling, Vienna, Austria
2. Törökbálint Medical Hospital, Department Of Pulmonology, Törökbálint, Hungary
Disclosure: Popp and Szondy have declared no relevant conflicts of interest.
Acknowledgements: Medical writing assistance provided by Amanda Barrell, Brighton, UK.
Disclaimer: The opinions expressed in this article belong solely to the named interviewees.
Support: The publication of this article was supported by Philip Morris International.
Citation: EMJ. 2022;7[4]:28-34. DOI/10.33590/emj/10044289. https://doi.org/10.33590/emj/10044289.
Interview Summary
The negative impact of smoking on the lung is well documented. Cigarette smoke is the cause of 90% of cases of chronic obstructive pulmonary disease (COPD), which includes chronic bronchitis and emphysema. COPD is a progressive and debilitating condition with morbidity and mortality rates similar to myocardial infarction (MI) and stroke. Despite the widely recognised risks, millions of people continue to smoke, in some cases even after receiving a diagnosis of COPD and despite knowing that the habit will accelerate disease progression. While there is no doubt that smoking cessation is the most important health intervention for all cigarette smokers, it can be challenging. Nicotine addiction, social norms and culture, and the length of time it can take smokers to feel the adverse consequences of the habit all contribute to the high cessation failure rate. However, increasing clinical and epidemiological evidence indicates that for those who are unwilling or cannot stop smoking, harm reduction strategies can help reduce exposure to the harmful chemicals and carcinogens released during tobacco combustion. Electronic devices heat processed tobacco without combusting it to deliver an aerosol containing fewer toxic products or harmful and potentially harmful constituents (HPHC) than cigarette smoke. Clinical evidence to support their use is growing. In Japan, for example, a decrease in hospitalisations due to COPD exacerbation after the introduction of such heat-not-burn (HNB), or tobacco heating systems (THS), has been reported.
In this article, Wolfgang Popp, Döbling Doctor’s Center, Privatklinik Döbling, Vienna, Austria, and Klara Szondy, Semmelweis University, Budapest, Hungary, discuss the impact of cigarette smoke on the lung, and how to support smoking cessation in those willing and able to quit smoking. They also explain when strategies that reduce the harmful effects of smoking may be useful, and outline the latest evidence supporting the use of HNB systems.
SMOKING AND PULMONARY HEALTH
The harmful effects of cigarette smoke on human health are well documented and supported by evidence from preclinical, clinical, and epidemiological studies. Cigarette smoking damages multiple organs and leads to 8 million global deaths per year from direct use and passive exposure of cigarette smoke to non-smokers.1 Smoking is associated with the development of at least 15 types of cancer,2 including 80% of all cases of lung cancer,3 and also laryngeal, oral, oesophageal, kidney, and bladder cancer.2 Explaining that the habit reduced an individual’s lifespan by an average of 10 years,4 Popp said: “A heavy smoker has a one in eight chance of developing lung cancer, and smoking is an important risk factor for cardiovascular diseases. The risk of infections (bacterial infection and viral disease) is increased in smokers. We see so many problems with smoking.”
Outlining its impact on pulmonary health, Szondy stated that cigarette smoke, which is generated when tobacco is ignited to temperatures of up to 900 °C in the burning tip,5 contains many toxic substances that are harmful to the human body. “Since the majority of them enter the lung, they understandably damage the lung’s mucous membrane, which leads to emphysema and damage to flagella, resulting in worse lung clearance,” Szondy said, explaining that emphysema and poor lung clearage were characteristic of COPD.6 “When entering the alveolar space, these materials are absorbed and damage other organs as well via oxidative stress and an incidental inflammatory pathomechanism,” they added.
Smoking-related structural lung changes are responsible for an estimated 90% of all cases of COPD,7 a chronic and progressive lung disease that includes chronic bronchitis and emphysema.8 Long-term exposure to the toxic substances released during tobacco combustion, or HPHCs, contributes to chronic inflammation that causes airway narrowing and reduced lung expansion. COPD is characterised by progressive airflow limitation and lung tissue destruction, which results in dyspnoea, chronic cough, and expectoration.9 Popp described COPD as “a hard disease to live with.” Popp also stated that COPD “is something that really decreases health-related quality of life (HRQoL).”
Popp also stated that “people will have these problems for the rest of their life. They have the sputum production, the shortness of breath, the difficulties breathing in the morning. Then there are the social problems; people do not go out because they will be out of breath for the rest of the day. They have to use inhalers and other medicines and experience the side effects.” The chronic course of COPD includes exacerbations, which can significantly impact HRQoL and health outcomes. Exacerbations of COPD are defined as acute episodes of clinical instability characterised by worsening respiratory symptoms, which often require hospitalisation.10 Exacerbations of COPD tend to become more common in the moderate and severe stages of disease (Global Initiative for Chronic Obstructive Lung Disease [GOLD] Stages II–IV) and are associated with increased morbidity and mortality.10 Explaining that hospitalisation for COPD exacerbation has a lower survival rate than MI, Popp stated that “COPD is more dangerous than MI.”11
The economic burden of the healthcare costs and social consequences of lung disease associated with smoking, including COPD, are also significant. Szondy stated that “the illnesses represent a great burden on healthcare, not only because the treatment is costly, but also due to their impact on hospital wards and the healthcare system.” According to a 2017 report from the British Lung Foundation (BLF), the annual economic burden of COPD in direct healthcare and indirect societal costs to the UK economy alone is 1.9 billion GBP.12 In Europe, the annual costs of healthcare and lost productivity due to COPD are estimated at 48.4 billion EUR.13 “In addition to the financial implications for family members, emotional stress is also a huge factor, partly due to their concern for a loved one and partly because they must carry the burden of the illness together,” Szondy added.
Despite the well-documented consequences of tobacco use and the clear medical and economic incentives to cease smoking, an estimated 1.3 billion people worldwide still smoke, which includes many smokers with a diagnosis of COPD.1,14 For people living with the condition, smoking cessation is the most effective intervention for halting progression, increasing survival, and reducing morbidity. However, approximately 54–77% of patients with mild COPD (Stage I) and 38–51% of patients with severe COPD (Stages III and IV) continue to smoke.14 Popp stated that “many very severe patients, those with Stage III and IV disease stop because they cannot breathe anymore. They have to use oxygen, and that makes it hard to smoke. Unfortunately, many patients with COPD Stage II, who could modify the course of their disease, continue to smoke.”
SUPPORTING SMOKING CESSATION
Physiological, psychological, and societal factors are all barriers to smoking cessation. “Smoking brings some people together; when we smoke together, it is a social situation,” said Popp, adding that it was simply part of the culture in some places. “It has a psychotropic effect that amplifies the current situation,” Popp said. However, many smokers want to stop. “I believe that more than one-half want to give up, and about 80% have already tried. The real problem is the addiction itself. Nicotine reaches the brain, activating dopamine neurons in just a few seconds, making it highly addictive,”15 said Popp. Unsuccessful cessation attempts are often attributable to the “well-known and barely tolerable symptoms of nicotine withdrawal,” added Szondy. “Irritability, unease, poor concentration, headaches, fatigue, excessive perspiration, weight gain due to slow metabolism, anxiety, and cravings are all among the symptoms of nicotine withdrawal,” Szondy said.
“Supporting cessation can be challenging,” said Popp, adding that the first step is a willing patient. “You have to have a motivated patient, that is the most important thing. As a doctor, you cannot give motivation, you can only take it away,” Popp said. They also stated that “education and awareness are the keys to building this motivation. Doctors have to help the patient to understand that they are addicted, that this addiction is doing them harm, and that they do not need the addiction to be happy.”
Popp highlighted the European Society of Cardiology (ESC) ‘Five As’ stepwise approach to supporting patients who are trying to stop smoking:16
- Ask: systematically inquire about smoking status at every opportunity
- Advise: unequivocally urge all smokers to quit
- Assess: determine the person’s degree of addiction and readiness to quit
- Assist: agree on a smoking cessation strategy, including setting a quit date, behavioural counselling, and pharmacological support
- Arrange: schedule a follow-up appointment to discuss progress, and offer any additional support that might be necessary
Szondy made clear that ongoing education programmes, one-to-one counselling, and raising awareness of health and social issues are the most effective means of smoking cessation support. However, this approach may not work for everyone. “Despite our best efforts, a mere 5–8% of smokers are able to quit,17 even with all the help provided,” Szondy said.
HARM REDUCTION
Smoking cessation remains the first-line intervention, but harm reduction strategies provide a practical second-line intervention for people unwilling or unable to stop completely. The concept is well established in substance and alcohol misuse fields, and has shown to be effective in reducing morbidity and mortality where abstinence is not feasible.18 When applied to smoking, harm reduction strategies can include encouraging those unwilling or unable to quit to switch to smoke-free products, such as e-cigarettes or HNB systems.19 “Thanks to advances in science and technology, nowadays there are alternative tobacco products, which provide an opportunity for nicotine intake without combustion and smoke alongside the mental pleasure of smoking for those who are unable or unwilling to quit smoking,” said Szondy.20
HNB systems heat tobacco to create an aerosol that contains nicotine and a tobacco flavour, but with significantly fewer HPHCs and toxic agents than cigarette smoke.21 Studies suggest these systems have the potential to reduce the risk to health when compared with traditional, combustible cigarettes.22-25 “For example, participants in a 6-month clinical study who predominantly used Philip Morris International’s (PMI [New York City, New York, USA]) HNB product (≥70% HNB) had biomarker levels indicating substantially reduced exposure to a broad range of HPHCs,”22 said Szondy. “Significantly less HPHCs associated with smoking are released when such products are used, meaning less harmful substances enter the bodies of adult smokers who cannot quit and the people around them,” Szondy said.
With the growing evidence to support smoking harm reduction strategies, regulators and policy leaders are increasingly backing them. For example, the authors of the ESC smoking cessation guidelines26 identified evidence that e-cigarettes were “probably less harmful than tobacco”27 and more effective than nicotine replacement therapy.28 The guidelines also noted that HNBs are lower in toxic agents when compared with regular cigarettes, although a warning was given that these systems do still contain tobacco.26 In the USA, the U.S. Food and Drug Administration (FDA) has authorised the marketing of PMI’s HNB product IQOS™ (Philip Morris International) as a modified-risk tobacco product.29,30 Heating rather than burning tobacco significantly reduces the production of HPHCs, and scientific studies showed that completely switching from conventional cigarettes to the IQOS system reduced exposure to toxic agents.29,30
Of course, it is important to note that such approaches are not risk-free. Most of the new products contain nicotine, which is addictive. The long-term effects are not yet known, but potential side effects of e-cigarettes include cough, trouble breathing or chest pain, nausea, vomiting, diarrhoea, fatigue, fever, or weight loss.31 There is also evidence to suggest that HNB systems can lead to oxidative stress, atrial stiffness, elevated heart rate and blood pressure, and vascular endothelial dysfunction.32
However, Popp and Szondy said they had seen how smokers were impacted by switching to HNB products. “In our experience,” said Szondy, “those suffering from smoking-related respiratory diseases stop coughing soon after switching to heated tobacco products, with a rapid improvement in lung clearance.”
Popp said that this effect helped them to use harm reduction strategies as a tool to aid complete smoking cessation. “Heated tobacco products reduce risk by producing a lower level of harmful substances. Carcinogenic substances and carbon monoxide are reduced immediately,” they said. Popp confirmed that using these supportive products allows people to feel the benefits of cessation, whether they be increasing fitness levels or improvements in taste, and helps people better appreciate the reasons to stop completely.
CLINICAL EVIDENCE BASE
A growing number of clinical studies on the effects of HNB systems on pulmonary health have been published in recent years, further supporting their use. Szondy stated that “while previously the only results available for the impact assessment of tobacco heating system technologies essentially came from in vitro research and in vivo animal model studies, the most recent publications contain the results of follow-up studies at the population level.”
For example, HNB technologies were first introduced to the Japanese market in 2014, allowing for a real-world study of hospitalisations for COPD before and after their use.33 Analyses of real-word evidence provided the first evidence that HNB technologies could considerably reduce the consumption of conventional cigarettes among active smokers (p<0.01), and may also significantly reduce hospitalisations due to acute exacerbations of COPD.33
A 5-year follow-up cohort study from Kazakhstan evaluating exacerbations, symptoms, and lung function in people who used IQOS (n=400) compared with cigarette smokers (n=801) has published preliminary data from the 2-year follow-up.34 Szondy said: “Persons aged between 40 and 59 years who had been smoking for at least 10 years and had switched to using mainly HNB products (>70%) were recruited as subjects, while the control group consisted of persons in the same age groups who smoked conventional cigarettes.”34 Szondy also explained that “according to the study results, tests of pulmonary function, such as the forced expiratory volume in the first second and forced vital capacity measured before and after bronchodilation, showed improved results for THS users compared to people smoking conventional cigarettes (both p<0.05 [ Table 1 ]). There were some positive effects among people who used THS in terms of conditions associated with metabolic syndrome, with the most significant improvement being related to blood pressure.”34
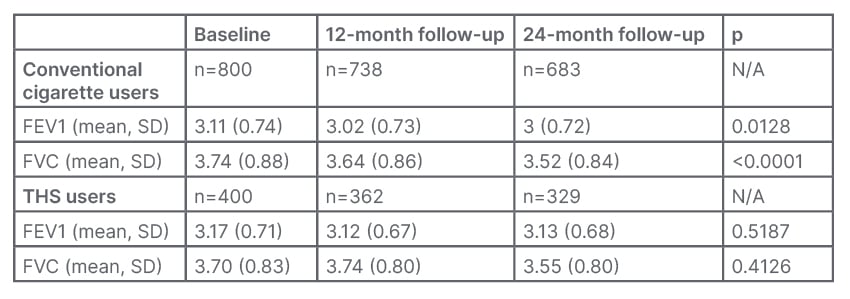
Table 1: Forced expiratory air volume and forced vital capacity among conventional cigarette and heat-not-burn users at baseline, 12- and 24-month follow-ups.34
P values were calculated with one-way analysis of variance for comparison of conventional cigarette and THS users at baseline and the two follow-up visits.
No post hoc tests were performed. FEV1: forced expiratory air volume; FVC: forced vital capacity ratio; N/A: not applicable; SD: standard deviation; THS: tobacco heating system.
In Italy, a retrospective study by Polosa et al.35 looked at the effects of HNB product use on changes in COPD status between 2017 and 2020. Daily cigarette consumption, yearly exacerbation events, pulmonary function, patient-reported health outcomes, and the results of a 6-minute walk test (6MWT) test were measured in 19 adult smokers with COPD who reduced conventional smoking (dual users) or achieved abstinence by switching to heated tobacco products at months 0, 12, 24, and 36.35 The age- and sex-matched control group comprised of 19 patients with COPD who used conventional cigarettes. Over the course of the study, dual users reduced daily conventional cigarette smoking by at least 70%.35 “All in all, the number of acute exacerbations dropped by more than 40% while using THS,”35 said Szondy. No significant pulmonary function changes were observed in either group. However, in many cases, the THS users moved from GOLD Stages IV and III to GOLD Stages II and I, while disease classification remained essentially the same in the control group.35 When recording the COPD Assessment Test (CAT) score, which measures patient-reported disease burden on parameters including cough frequency, chest tightness, and restrictions to daily living, patients with COPD using THS reported significant improvements at all follow-up assessments. However, no changes were seen in the control group (Table 2).35 Popp said the “most important medical results” from the study were those that had the most impact on patients’ wellbeing (i.e., the reduction in exacerbations and CAT score improvements).
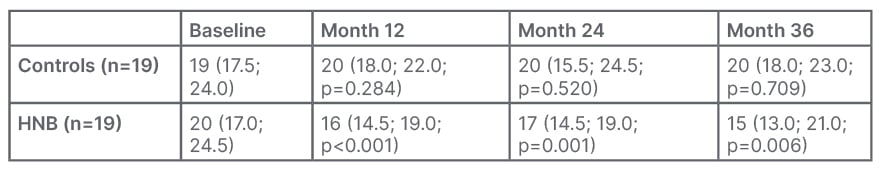
Table 2: Comparison of chronic obstructive pulmonary disease assessment test (CAT) score between controls and heat-processed tobacco users at baseline, 12-, 24-, and 36-month follow-up visits.35
P values were calculated through within-group comparisons vs baseline.
HNB: heat-not-burn.
In terms of physical endurance, an improvement was observed in the THS cohort, as recorded by the 6MWT (p=0.005). Those in the control group recorded a median distance of 250 m at baseline and 270 m at 3 years. In comparison, a median distance of 281 m was recorded among THS users at baseline, and this had increased to 350 m at a 3-year follow-up. The average improvement among the THS users was 69 m.35 Szondy said: “According to the results of the trial, smokers who were patients with COPD and stopped consuming or at least significantly reduced their consumption of conventional cigarettes while using THS reported long-term improvement of numerous objective and subjective parameters during the 3-year follow-up period. All of this seems to demonstrate how smokeless technologies achieve harm reduction. The reduction in disease burden is most likely attributable to the lack of chronic exposure to combustion products.” No long-term harmful effects caused by THS were identified during the trial.35 Szondy added: “The first impact assessment involving patients with COPD and other results accumulated in recent years seem to indicate that switching to smoke-free HNB technologies offers significant improvement in terms of HRQoL and physical activity among patients who are unable or unwilling to quit smoking for some reason.”35
However, it should be noted that the study conducted by Polosa et al.35 indicated that while harm reduction can slow down disease progression, the deterioration of pulmonary function caused by COPD is an irreversible effect of smoking. In addition, despite the overall reduction of the harmful effects of consuming tobacco products for those who do not quit smoking, THS “definitely cannot be regarded as risk-free,” emphasised Szondy. “Additional studies are required in order for us to draw valid conclusions,” they said, explaining that the long-term effects of glycerine, a compound present in heated tobacco products, on the bronchial mucous membrane are not yet known.
CONCLUSION
The fact that smoking kills has been proven. Studies published over the last six decades have built an indisputable evidence base demonstrating that cigarette smoke leads to multiple conditions including cancers and pulmonary diseases such as COPD. “Fully refraining from using nicotine and tobacco products continues to be the most effective way of reducing the harm caused by smoking,” said Szondy.
However, harm reduction strategies, including using HNB products, provide another option to help people. “I believe this is a much better way to save people than to say: ‘quit or die’. Harm reduction in cigarette smoking, just the same as in alcohol or drugs, is a more holistic, more humanistic approach,” said Popp.








