Abstract
Radiographic axial spondyloarthritis is a chronic autoimmune disorder primarily affecting the axial skeleton, causing pain, stiffness, and, in advanced cases, structural damage. Its varied clinical presentation complicates diagnosis, particularly in resource-limited settings like secondary-level hospitals in Ecuador. This report details the case of a 34-year-old female initially misdiagnosed with seronegative rheumatoid arthritis and treated with methotrexate, hydroxychloroquine, and corticosteroids. Despite treatment, her symptoms persisted until an MRI, limited by unavailable STIR sequences, confirmed left-sided sacroiliitis. The case was further complicated by idiopathic sudden hearing loss, severe hip involvement, and osteopenia. Cultures were negative, and the diagnosis was ultimately based on clinical criteria and imaging findings. This case highlights the challenges of diagnosing radiographic axial spondyloarthritis in resource-limited settings, and underscores the importance of interdisciplinary evaluation to avoid diagnostic delays and long-term disability.
Key Points
1. Early diagnosis of radiographic axial spondyloarthritis is crucial for comprehensive management and long-term disability prevention, especially in resource-limited settings such as primary and secondary healthcare facilities in Ecuador.2. Interdisciplinary collaboration and access to advanced imaging techniques, such as MRI with STIR sequences, are essential to avoid diagnostic delays in complex autoimmune diseases.
3. Strengthening local training programmes for healthcare providers on the clinical recognition of axial spondyloarthritis can enhance diagnostic accuracy in emerging economies with limited access to specialised resources.
INTRODUCTION
Radiographic axial spondyloarthritis (r-axSpA), formerly known as ankylosing spondylitis (AS), is a chronic inflammatory disease that primarily affects the sacroiliac joints and axial skeleton. It leads to pain, stiffness, and, over time, structural deformities such as thoracolumbar kyphosis.1 The prevalence of r-axSpA globally ranges from 0.1–1.4%, and the condition is closely associated with the HLA-B27 gene, although environmental and microbial triggers also play a role in its pathogenesis.2,3 Diagnosing r-axSpA in the early stages is crucial to preventing permanent damage; however, this is often delayed, especially in settings with limited access to advanced imaging techniques.
In about 25.8% of cases, extra-articular manifestations such as uveitis, psoriasis, or inflammatory bowel disease accompany axial symptoms.4
The paradoxical occurrence of bone destruction and new bone formation, driven by inflammatory mediators like TNF and IL-17A, characterise the disease. In advanced stages, this can lead to the formation of a ‘bamboo spine’ due to syndesmophytes.5 Early diagnosis and targeted therapy, such as TNF-α and IL-17 inhibitors, are essential to prevent long-term disability.6 However, in secondary-level healthcare settings, especially in developing regions, diagnosis is often delayed due to limited access to specialised tests and imaging techniques.
Although non-HLA genes also contribute to the development of this condition, HLA-B27 is the primary genetic factor.6-8 In r-axSpA, there is a paradoxical occurrence of inflammatory bone destruction and new bone formation at the entheses, leading to the formation of syndesmophytes and, in severe cases, a rigid ‘bamboo spine’ characteristic of r-axSpA.2,5
Proinflammatory mediators, such as cyclooxygenase (COX), TNF, IL-17A, and JAK, have been validated by clinical observations.5 Effective therapies focus on targeting these mediators, particularly TNF- and IL-17A, which are crucial in inflammation. The gut microbiome is also important, particularly when weakened mucosal barriers permit microbial invasion and trigger systemic immune responses. Interactions between the gut microbiome, genetic factors, and environmental factors result in diverse clinical presentations of spondyloarthritis (SpA).5
SpA is an umbrella term covering a group of diseases, including psoriatic arthritis, reactive arthritis, and enteropathic arthritis.9 Early diagnosis and targeted therapies, such as TNF-α and IL-17 inhibitors, are crucial to prevent long-term disability.10-14
This report presents the case of a young adult female from Ecuador, initially misdiagnosed with seronegative rheumatoid arthritis (RA) and later diagnosed with r-axSpA. The case underscores the diagnostic difficulties in Ecuador, where healthcare providers often face equipment limitations and a lack of access to specialised tests such as MRI with STIR sequences.
CASE PRESENTATION
A 34-year-old female presented to a secondary-level hospital in Guayaquil, Ecuador, with a 6-month history of joint pain, lower extremity oedema, and episodic hypochromic skin lesions. The lesions were non-specific and did not persist long enough to establish a diagnosis of psoriasis. Initially diagnosed with RA in November 2022, she was treated with prednisone (10 mg daily), methotrexate (12.5 mg weekly), and hydroxychloroquine (200 mg daily). Despite treatment, her symptoms persisted, and her right hip pain worsened, significantly limiting her mobility by March 2023, necessitating the use of a walker. She also reported recurrent episodes of childhood hip pain.
Radiological Findings
Initial X-rays revealed severe bilateral destruction of the femoral heads and chronic hip subluxation (Figure 1). These changes were suggestive of significant inflammatory damage, potentially exacerbated by prolonged corticosteroid use, contributing to avascular necrosis. A DEXA scan, though unavailable, was inferred based on clinical interpretation and osteopenia observed on the X-rays. The radiological findings pointed to a T-score of -2.4 in the L1-L4 vertebrae and the femur, suggesting reduced bone mineral density, which further complicated the case.

Figure 1: Bilateral anteroposterior hip X-ray.
The X-ray shows significant destruction of the femoral heads, indicative of possible inflammatory changes. Arrows highlight areas of concern.
MRI and diagnostic reassessment.
In November 2023, an MRI was ordered to confirm sacroiliitis using STIR sequences, but due to equipment malfunction and the limited availability of imaging resources, these sequences were not available. The MRI still revealed unilateral left-sided sacroiliitis, coccygeal erosions, and joint widening (Figure 2). While bilateral sacroiliitis is more common in r-axSpA, this case presented with unilateral involvement, raising the need to consider other differential diagnoses such as psoriatic arthritis or an infectious cause. However, cultures for tuberculosis and bacterial infections returned negative, ruling out these aetiologies. No biopsy was performed on the sacroiliac joint due to the limitations of the hospital’s resources.
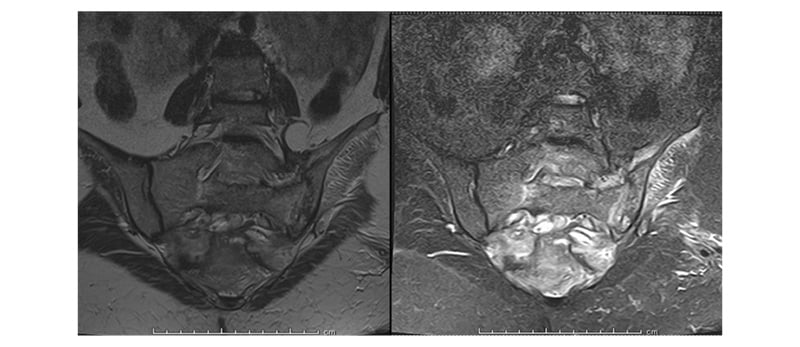
Figure 2: Lumbar magnetic resonance imaging.
MRI findings indicate unilateral sacroiliitis and erosive changes, warranting further investigation for differential diagnoses.
Given the persistence of symptoms, elevated C-reactive protein levels (Table 1), and clinical findings, the diagnosis was primarily based on clinical criteria for r-axSpA, despite the lack of bilateral sacroiliitis and without definitive support from STIR sequences.
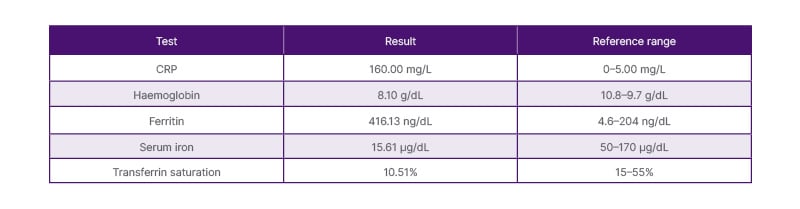
Table 1: Relevant laboratory results.
CRP: C-reactive protein.
Ethical Considerations
Informed consent was obtained from patients to use their clinical information for this study.
DISCUSSION
This case underscores the diagnostic challenges faced in diagnosing r-axSpA in Ecuador, particularly in secondary-level hospitals with limited resources. The patient’s initial misdiagnosis with seronegative RA delayed the correct diagnosis and led to treatment with corticosteroids, which likely contributed to avascular necrosis of the femoral heads. The absence of STIR sequences on the MRI and the unusual presentation of unilateral sacroiliitis added further complexity to the case.
Although the presentation of unilateral sacroiliitis is atypical for r-axSpA, this diagnosis was supported by the exclusion of infectious causes, the patient’s clinical history, and the elevated inflammatory markers. The episodic hypochromic skin lesions were not consistent with psoriatic arthritis, and their transient nature precluded a definitive diagnosis of psoriasis. This case also highlights the importance of recognising the limitations of healthcare settings when interpreting clinical and imaging findings, particularly in regions with restricted access to advanced diagnostics.
The discussion also considered the impact of prolonged corticosteroid use, which may have contributed to avascular necrosis, further complicating the clinical picture. Access to therapies such as TNF-α inhibitors and IL-17 blockers remains limited in these settings, emphasising the need for healthcare reforms to improve diagnostic and treatment options for patients with spondyloarthropathies.
r-axSpA frequently presents with significant axial skeleton involvement but may also manifest with extra-articular symptoms, such as sudden hearing loss, as seen in this patient.1,2 The presence of severe hip involvement and reduced bone mineral density further complicated the clinical picture.
r-axSpA belongs to the broader category of spondyloarthropathies, which also includes psoriatic arthritis, reactive arthritis, and enteropathic arthritis.9 The association between r-axSpA and the HLA-B27 genotype has been well documented; however, only 24.4% of the disease’s genetic basis is attributable to HLA-B27.11 In recent studies, novel genetic variants, such as mutations in the RELN gene, have offered additional insights into the pathogenesis of r-axSpA.13
Therapeutic strategies involving TNF-α inhibitors such as infliximab, adalimumab, etanercept, golimumab, and certolizumab are now the gold standard for active disease management.12 However, access to these treatments remains limited in secondary-level hospitals in developing regions. The use of MRI in this case was pivotal for diagnosis, as sacroiliitis was not evident in initial radiographs, underscoring the importance of advanced imaging techniques in detecting early-stage r-axSpA.5
Robotic-arm-assisted total hip arthroplasty has been proposed as an option to manage severe hip ankylosis and improve recovery in complex cases.15 Despite recent advances in treatment, public awareness of r-axSpA remains low, leading to delays in diagnosis and poorer outcomes.16
CONCLUSION
This case illustrates the complexities of diagnosing r-axSpA in resource-limited settings, such as secondary-level hospitals in Ecuador. Limited access to advanced imaging techniques and the potential for misdiagnosis increase the likelihood of delayed recognition of r-axSpA. Early interdisciplinary evaluation, along with improved diagnostic resources, is essential to prevent long-term disability and improve patient outcomes in these settings.







