Abstract
Adnexal structures that can undergo torsion include the ovary, isolated fallopian tube, both tube and ovary, broad ligament leiomyoma, and pedunculated leiomyoma. Torsion of a subserosal leiomyoma, like ovarian torsion, demands prompt surgical attention to avoid further complications like infection and peritonitis. Here, the authors provide an overview of a 35-year-old patient who was suspected of having an ovarian torsion. On ultrasound, there were multiple intramural and subserosal leiomyomas with normal ovaries. One of the pedunculated subserosal leiomyomas showed altered morphology suspicious for torsion. The diagnosis for leiomyoma torsion was further confirmed on MRI and later correlated with the intraoperative findings.
Key Points
1. Torsion of a subserosal leiomyoma, such as ovarian torsion, demands prompt surgical attention to avoid further complications like infection and peritonitis.2. This case report highlights the imaging findings of torsed subserosal fibroid amongst other uncomplicated fibroids on ultrasound and MRI, and its correlation with post-operative specimen.
3. Heterogeneity with loss of whorled pattern in a pedunculated subserosal fibroid and presence of normal ovaries favour torsed subserosal leiomyoma on ultrasonogram. On MRI, heterogeneous appearance and non-enhancement, along with bridging vessel and dark fan sign increase the diagnostic confidence.
INTRODUCTION
Leiomyomas or fibroids are the most frequently encountered benign neoplasm of smooth muscle origin in women of reproductive age group.1-3 Pedunculated leiomyoma (a type of subserosal leiomyoma) is uncommon and its torsion is rare, and therefore not commonly diagnosed. Pedunculated subserosal fibroid requires immediate surgical intervention. A delay in diagnosis can lead to unfavourable outcomes like gangrene and peritonitis.1,2
CASE REPORT
A 35-year-old patient came with acute lower abdominal pain predominantly on the left side. Pregnancy test using urine yielded a negative result. Ovarian torsion was suspected, and the patient was referred for an ultrasonography examination.
Ultrasonography of the pelvis showed multiple subserosal and intramural hypoechoic lesions with a whorled appearance suggestive of leiomyomas. There was a large, well-circumscribed heterogeneously hyperechoic lesion in the left adnexa connected to the uterus via a pedicle, suggestive of a pedunculated leiomyoma. Doppler examination showed vascularity in the proximal part of the pedicle, with the absent flow in the distal part. There was patchy arterial flow with absent venous flow in the leiomyoma. Both the ovaries were normal, ruling out ovarian torsion (Figure 1 A–C).
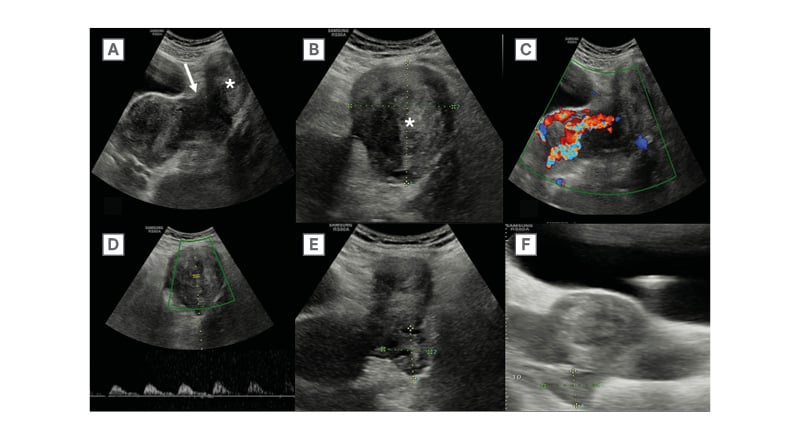
Figure 1: Transabdominal ultrasonography of pelvis on B-mode and colour Doppler.
A and B) Ultrasonography images through the left adnexa show well-circumscribed heterogeneously hyperechoic lesion (*) connected to the uterus via a pedicle (white arrow), suggestive of a pedunculated leiomyoma. C and D) Doppler ultrasound images show vascularity in the proximal part of the pedicle with absent flow in distal part.
There was patchy arterial flow with a monophasic waveform and absent venous flow in the leiomyoma.
E and F) Both the ovaries were normal.
MRI pelvis was performed subsequently to further confirm the ultrasonography findings. MRI showed multiple T2 hypointense intramural and subserosal leiomyomas. A pedunculated leiomyoma was seen in the left adnexa, showing a heterogeneous T2 hyperintense signal (Figure 2 A–D). Post-contrast sequences showed non-enhancing areas in the pedunculated leiomyoma with associated diffusion restriction (Figure 3 A–C).
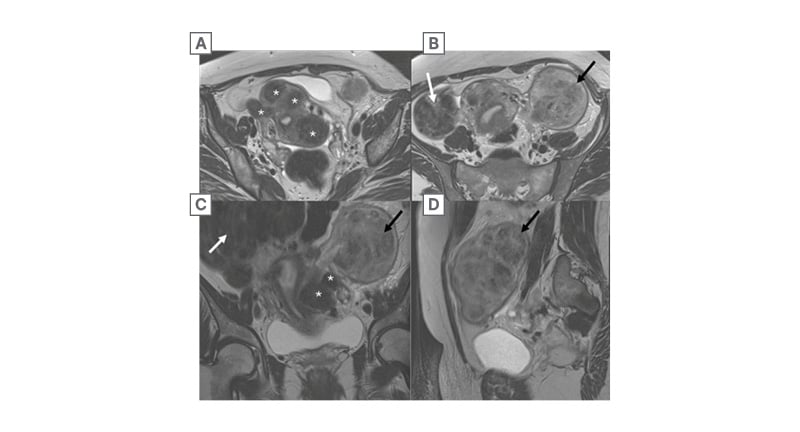
Figure 2: MRI pelvis T2W sequence.
A) T2 weighted axial image of the MRI pelvis at a lower level, B) T2 weighted axial image of the MRI pelvis at a higher level , and C/D) T2 weighted coronal and sagittal images of the MRI pelvis show multiple T2 hypointense intramural and subserosal leiomyomas (*). Large subserosal leiomyoma is noted in the right adnexa (white arrow), with a pedunculated leiomyoma in the left adnexa (black arrow) connected to the uterus via pedicle. The pedunculated leiomyoma shows heterogenous T2 hyperintense signal.
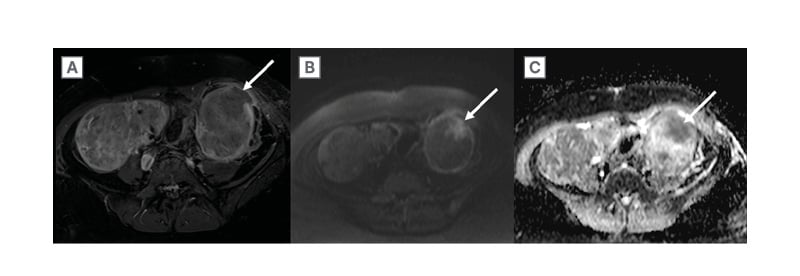
Figure 3: MRI pelvis post contrast T1FS, and diffusion weighted with apparent diffusion coefficient map.
A) Axial post-contrast T1 fat saturated, B) diffusion weighted, and C) apparent diffusion coefficient images show non-enhancing area in the pedunculated fibroid on the left, with corresponding hyperintense signal on diffusion weighted and drop in signal on apparent diffusion coefficient images suggestive of diffusion restriction (white arrows).
Pre-operative blood parameters revealed mild leukocytosis (white blood cell counts 13,000 /μL) and low haemoglobin levels (-9 gm/dL). The patient was taken up for an emergency open myomectomy in view of urgent exploration of torsed fibroid and the need for fertility preservation. A twisted pedicle of the leiomyoma was observed intraoperatively. The torsed leiomyoma was dark and dusky in appearance as compared to other uncomplicated leiomyomas that were pink on gross morphology (Figure 4 A and B).
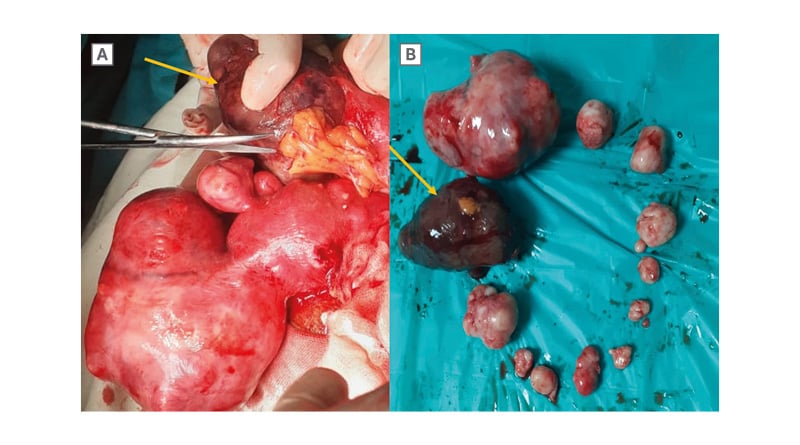
Figure 4: Post myomectomy intraoperative specimens.
A) Intraoperative and B) post-myomectomy specimen images show multiple intramural and subserosal leiomyomas of variable sizes. The torsed leiomyoma (yellow arrow) is dark and dusky as compared to other uncomplicated leiomyomas which are pink on gross morphology.
DISCUSSION
A woman at reproductive age with lower abdominal pain can present as an acute surgical emergency with obstetric or non-obstetric causes. Obstetric causes include ectopic pregnancy, uterine dehiscence, and abruptio placenta. Non-obstetric causes are ovarian torsion, urinary tract calculi, appendicitis, and leiomyoma degeneration/torsion.3
Patients with uterine leiomyomas are usually asymptomatic, but may sometimes present with dysmenorrhoea, menorrhagia, or infertility. Various possible complications related to leiomyomas are degeneration, urinary retention, uterine prolapse, and torsion.1-4 Pedunculated leiomyoma is uncommon, and its torsion is rare. The risk of torsion is higher when the stalk of the pedunculated subserosal fibroid is slender and elongated.1
Leiomyoma torsion initially causes venous stasis, congestion, and oedema. There is subsequent arterial compromise that leads to gangrene and haemorrhagic necrosis.1 Since there is an overlap with the imaging findings of fibroid degeneration, most of the time the diagnosis is made intraoperatively by confirming the vascular pedicle that has undergone twisting.1,2,4
On ultrasonography, a normal uterine leiomyoma appears as a hypoechoic solid mass with a whorled pattern and peripheral vascularity. Torsed subserosal fibroid appears heterogeneously hypoechoic to hyperechoic with loss of whorled pattern and absence of vascularity on colour Doppler. The presence of the twisted pedicle differentiates heterogeneity in torsed leiomyoma from degenerative fibroid and leiomyosarcoma. The pedicle often shows a twist with a resultant abrupt vascular cut-off. Sometimes on colour Doppler, due to congestion, only arterial waveforms are elicited with absent venous flow.1,2
A typical leiomyoma shows a T1 and T2 hypointense signal on MRI. A torsed leiomyoma is heterogeneously hyperintense on T2W imaging and intermediate/heterogeneous on T1W imaging. It shows a peripheral rim of enhancement (due to oedema and obstructed venous channels) with a central non-enhancing necrotic core. Table 1 differentiates between a torsed subserosal fibroid and an uncomplicated fibroid. There are flow voids between the subserosal leiomyoma and uterus, which is described as the ‘bridging vessel’ sign in the literature.1 This helps to differentiate whether the lesion originates from the uterus or adnexa. Another sign called the ‘dark fan sign’ is appreciated in the post-contrast sequence, where the uterus adjacent to the twisted leiomyoma shows poor enhancement.1 An increase in the size of the subserosal fibroid on serial imaging with altered perfusion is another clue in the cross-sectional imaging.4 CT can help in diagnosis by demonstrating a twisted vascular pedicle with non-enhancement of the pedunculated leiomyoma. It also rules out other causes of acute abdomen.5
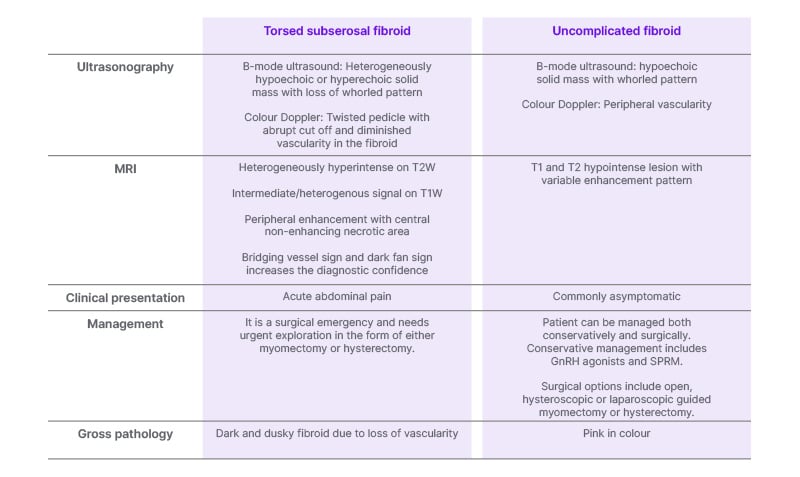
Table 1: Torsed subserosal fibroid versus uncomplicated fibroid.
GnRH: gonadotrophin-releasing hormone; SPRM: selective progesterone receptor modulators.
Management of uterine leiomyoma can be both surgical and conservative. It depends on the patient’s age, symptoms, and desire to preserve the fertility, as well as on surgeon’s experience and technology available in the institution. For an asymptomatic uncomplicated uterine leiomyoma various medications like gonadotrophin-releasing hormone agonists or selective progesterone receptor modulators can be used. Surgical options available are open, hysteroscopic, or laparoscopic guided myomectomy or hysterectomy. Minimally invasive/non-invasive procedures for leiomyomas are uterine artery embolisation and high-frequency magnetic resonance-guided focussed ultrasound surgery. Large fibroid (10–12 cm) and multiple fibroids are contraindications to laparoscopic myomectomy. Laparoscopic hysterectomy is preferred in the elderly symptomatic women who do not wish to preserve fertility.6
CONCLUSION
With clinical presentation similar to ovarian torsion, torsion of a leiomyoma, although a rare diagnosis, is an important differential in reproductive age group women with acute lower abdominal pain. The presence of a stalk between the uterus and the leiomyoma with absent vascularity and normal ovaries is key in the diagnosis. Prompt diagnosis and management is essential to avoid ischaemic gangrene, infection, and subsequent peritonitis.







