Abstract
Adrenal cortical carcinoma (ACC) is a rare malignant tumour which arises from the adrenal cortex with diverse clinical manifestations due to excessive hormone production, with Cushing’s syndrome and virilisation being the most common features. The diagnosis of ACC relies on clinical, hormonal, and imaging features before surgery and pathological examination after tumour removal. Pathological assessment of Weiss score and the Ki-67 labelling index play an important role in diagnosis and prognosis. The tumour, lymph node, and metastasis (TNM) classification, established by the European Network for the Study of Adrenal Tumors (ENSAT) is used for staging. Currently, complete surgical resection is the only treatment option for ACC that has a curative intent, with no reported difference in overall recurrence or mortality between open and laparoscopic adrenalectomy. Mitotane is used as an adjuvant therapy after surgery for high-risk patients and as primary treatment for unresectable and advanced cases; however, it has a narrow therapeutic index and regular blood monitoring is essential. The role of chemotherapy and radiotherapy in ACC is unclear with limited studies and varying results. To date, trials which have been conducted for novel agents revealed disappointing results. Currently, trials are underway for agents targeting steroidogenic factor-1, mechanistic target of rapamycin (mTOR), and Wnt signalling pathways, as well as inhibitors of acetyl-coA cholesterol acetyltransferase 1. Unfortunately, ACC has an aggressive natural course with high recurrence rate, and a reported 10-year survival of 7% after treatment.
INTRODUCTION
Adrenal cortical carcinoma (ACC) is a rare and aggressive endocrine malignancy with a reported annual incidence of approximately 1–2 cases per million.1,2 In the USA, the incidence is 0.7 cases per million per year and ACC accounts for 0.2% of all cancer deaths.3,4 It can occur at any age although there are two peak incidences: in early childhood and the 4th–5th decades of life. Women are more frequently affected with a female to male ratio of 1.5–2.5:1.4
GENETIC PREDISPOSITION
Inherited
The current understanding of the pathogenesis of ACC is incomplete and limited. Although most cases of adult ACC are sporadic, paediatric ACC can be associated with several genetic disorders, such as Li–Fraumeni syndrome (LFS), Beckwith–Wiedemann syndrome, multiple endocrine neoplasia Type 1, Carney complex, congenital adrenal hyperplasia, McCune–Albright syndrome, and familial adenomatous polyposis. Thus, TP53 mutations, seen in LFS and the alterations of the insulin-like growth factor 2 (IGF-2) of Beckwith–Wiedemann syndrome, are considered to be involved in the pathogenesis of ACC. Underlying LFS is diagnosed in 50–80% of all children with ACC, whereas it accounts for only 3.9–5.8% of adult onset ACC. In a recent study of 114 patients with ACC, 3.2% were reported to have Lynch syndrome, and germline mutations of MLH1 and MSH6 were identified in addition to MSH2 mutations detected in previous case reports of ACC with Lynch syndrome.5
Acquired
Genomic studies, such as exome sequencing, have confirmed that inactivating mutations of TP53 and activating mutations of the proto-oncogene b-catenin (CTNNB1) are implicated in the tumourigenesis of ACC.6,7 A gene involved in the Wnt signalling pathway, ZNRF3 (Zinc and ring finger protein 3), is reported to be the most frequently altered in ACC.7 In addition, comparative genomic hybridisation detects chromosomal gains at 5, 7, 12, 16, 19, and 20 as well as losses at 13 and 22. A specific CpG island methylator phenotype is found in association with hypermethylation of the promoters of specific genes, such as H19, PLAGL1, G0S2, and NDRG2. Moreover, some studies identified a significant upregulation of miR-483 and a downregulation of miR-195 and miR-335 in ACC.8
Recently, a new international collaboration as part of The Cancer Genome Atlas (TCGA) has identified several new genes that are associated with ACC, based on samples of 91 cases from countries across four continents; these genes are PRKAR1A, RPL22, TERF2, CCNE1, and NF1. Amplification of TERF2 and telomerase was found in several samples, suggesting that telomere maintenance could be involved in the development of ACC.9 In this recent study, 16% of the samples had a homozygous deletion of ZNRF3 with 19.3% having some alteration in this gene, which is in accordance with previous findings.7,9 Profound genomic instability, such as whole-genome doubling, is associated with an aggressive clinical course in ACC.9
Though IGF-2 is overexpressed in most cases of ACC, IGF-1 receptor-mediated downstream activation of the protein kinase B Akt/mechanistic target of rapamycin (mTOR) pathway does not play a major role in carcinogenesis. Studies using inhibitors of IGF-1R/mTOR signalling pathway revealed minimal tumour responses. Expression of hepatocyte growth factor (HGF) and its receptor, cMET, is increased in ACC, and HGF/cMET activation is associated with increased cell proliferation, reduced apoptosis, tumour-related angiogenesis, chemotherapy resistance, and cell survival.10
CLINICAL PRESENTATION
Clinical presentation of ACC is heterogeneous and the natural history can be highly variable. Many ACCs are asymptomatic and non-functional as adrenal incidentalomas identified on abdominal imaging; however, approximately 60–70% of ACCs in adults present with clinical syndrome of autonomous adrenocortical steroid excess, mainly Cushing’s syndrome or worsening androgenisation in females.11 Hormonally inactive ACCs present with symptoms related to local mass effects of the tumour, such as abdominal discomfort, back pain, nausea, or vomiting. Due to their deep location in the retroperitoneum, the majority of ACCs are large and locally advanced at the time of diagnosis. Frequently, ACCs invade adjacent large vessels, such as the renal vein or inferior vena cava.12
The majority of ACCs secrete a variable combination of glucocorticoids, mineralocorticoids, and sexual steroids. While clinical Cushing’s syndrome and virilisation in females are the most common manifestations of hormonally active ACCs, they can also present with features of hyperaldosteronism, such as hypertension and profound hypokalaemia, or pheochromocytoma. Oestrogen hypersecretion is rare with gynaecomastia and testicular atrophy present in only 5–10% of male patients who are pathognomonic for ACC.13 Children tend to have more functioning ACCs than adults. Virilising tumours are more prevalent in children because ACCs originate from the persistent fetal zone of the adrenal cortex, which produces dehydroepiandrosterone sulfate (DHEA-S).14
DIAGNOSIS
Imaging
Various imaging techniques, such as ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI), have greatly increased the detection rates of adrenal masses. However, no single imaging method can identify an adrenal mass as ACC. Some radiological features that suggest the likelihood of ACC include large tumour size, irregular margin, lobulated shape, heterogeneous appearance (due to haemorrhages and/or necrotic areas), calcifications, low fat content, and high attenuation on an unenhanced CT with irregular enhancement after contrast.7,15,16 ACC is more likely if the mass is >4 cm (sensitivity 97%; specificity 52%) and >6 cm (sensitivity 91%; specificity 80%).17
Low fat concentration of malignant lesions produce high attenuation on unenhanced CT; hence, it is recommended to perform a preliminary unenhanced CT attenuation measurement followed by an intravenous contrast scan for optimal imaging of the adrenal glands.13 A cut-off value of <10 HU in unenhanced CT has been used for the diagnosis of benign lesions. However, a recent analysis from the German ACC registry suggests 13 HU is the most sensitive threshold to distinguish adenoma from carcinoma.18 If unenhanced CT is indeterminate, a contrast enhanced CT should be performed to detect the washout, which is either absolute (the pre-contrast density is known) or relative (only a portal venous phase baseline is available), where an absolute washout of >50% suggests a benign lesion.7,13
Overall, MRI is as accurate as CT in differentiating adrenal adenomas and carcinomas, with a reported sensitivity of 84–100% and a specificity of 92–100%, similar to unenhanced CT.13 The presence of isointense to hypointense signals on T1-weighted images, a hyperintense signal on T2-weighted images and a heterogeneous signal drop on chemical shift are the MRI features helpful in the diagnosis of ACC, where CT fails to characterise the adrenal lesion perfectly.19,20
In addition, imaging plays an important role in staging as well as assessing the involvement of surrounding organs and vessels to evaluate the feasibility of radical surgery, and to monitor treatment response during follow-up. MRI is preferred for assessment of vascular invasion, whereas enhanced CT is extremely useful to detect organ invasion and metastatic spread. Three-dimensional reconstruction technology of CT or MRI images provide more detailed information about morphology and the anatomical relationship of ACCs, thus helping clinicians to develop an accurate surgical strategy, particularly for performing endoscopic or laparoscopic surgery.21
18F-fluorodeoxyglucose positron emission tomography (PET) is a second-line investigation for indeterminate cases or in staging of known ACC. In patients with impaired renal function, PET/CT may be an alternative to CT. PET was reported to be more sensitive than CT in the detection of local recurrence, while CT was more sensitive in detecting small peritoneal or lung metastases.22 PET/CT also demonstrates response to chemotherapy earlier than CT, as well as predicting the chemotherapeutic response of ACC before anatomic changes are detected with CT. Moreover, PET/CT may be useful for selecting the optimal treatment in patients with advanced disease.23
Advanced imaging modalities, such as 11C-metomidate PET and 123I-iodometomidate singlephoton emission computed tomography (SPECT), use metomidate which binds to CYP11B enzymes expressed in the adrenal cortex and are taken up by adrenocortical tissue. Such techniques were recently demonstrated to be useful in differentiating ACC from metastatic carcinoma.24
Hormonal Assessment
As ACCs secrete excessive adrenal hormones, the European Network for the Study of Adrenal Tumors (ENSAT) recommends a detailed pre-operative endocrine assessment for suspected ACC including basal cortisol, adrenocorticotropic hormone, dexamethasone suppression test, urinary free cortisol, DHEA-S, 17-hydroxyprogesterone, testosterone, androstenedione, and oestradiol. Measurements of plasma free metanephrines or urinary fractionated metanephrines and the aldosterone/renin ratio is also recommended to exclude pheochromocytoma and primary hyperaldosteronism, respectively.25
Pathology
Macroscopically, most ACCs are large, heterogeneous tumours with necrosis and invasion of the tumour capsule, surrounding soft tissues, blood vessels, or lymphatics. The colour of the mass varies from brown, orange, or yellow depending on the lipid content of the cells.7 Since ACC is a rare condition with special variants (paediatric, oncocytic, myxoid, and sarcomatoid) histopathological challenges encountered include differentiation of adrenocortical from adrenomedullary tumours, as well as adrenocortical adenomas from carcinomas.26 There are no clear-cut pathognomonic histological features for a carcinoma; thus, a combination of multiple features are used to diagnose ACC. The Weiss scoring system is widely used, which is based on 9 morphological parameters on light microscopy: 3 each for tumour structure (diffuse architecture, confluent necrosis, clear cells), cytological features (nuclear atypia, mitotic index, atypical mitoses), and invasion (sinusoidal, venous, capsular) (Table 1). It is established that a Weiss score of ≥3 indicates an ACC, whereas scores between 0 and 2 define an adenoma.27,28
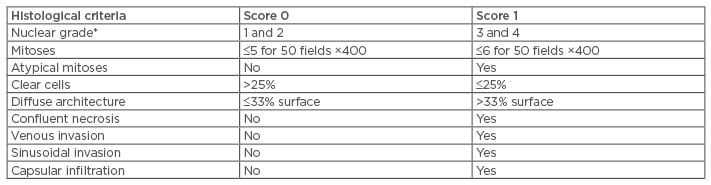
Table 1: Weiss scoring system.
*Grade 1: (round nuclei, homogenous, small size, no nucleoli); Grade 2: (nuclei slightly irregular, more voluminous, conspicuous nucleoli at ×400); Grade 3: (irregular nuclei, voluminous nucleoli at ×100); Grade 4: (the same as Grade 3 with monstrous cells and very irregular nuclei).
The Ki-67 labelling index (Ki-67 LI), a marker of proliferation, plays a pivotal role in differential diagnosis of adrenocortical carcinomas from adenomas, with a cut-off value of 2.5–5.0%, although a cut-off of 5% was reported to yield high sensitivity (87.5%) and specificity (97.5%). It is also one of the important prognostic indicators of survival in ACC patients, with a value of >10% leading to shorter overall survival (OS) and more recurrences.29 As ACCs show significant intratumoural heterogeneity, the Ki-67 LI in ‘hot spots’ is significantly higher than that in average areas, by both manual and digital image analyses. In addition, it correlates with the Weiss criteria (oeosinophilic cytoplasm, nuclear atypia, atypical mitoses, and sinusoidal invasion).30
Staging
The tumour, lymph node, and metastasis (TNM) classification system, proposed by ENSAT, is used to assess the local extension of primary tumours, lymph node involvement, and the presence of distant metastasis (Table 2). Both the Weiss system and TNM staging are useful in predicting the prognosis of ACCs and correlate with each other, with patients at TNM Stages III and IV having a high Weiss score.31
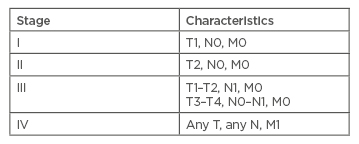
Table 2: Tumour, lymph node, and metastasis staging system for adrenal cortical carcinoma.
T1: tumour ≤5 cm; T2: tumour >5 cm; T3: tumour infiltration into surrounding tissue; T4: tumour invasion into adjacent organs or venous tumour thrombus in vena cava or renal vein; N0: no positive lymph nodes; N1 positive lymph node(s); M0: no distant metastases; M1: presence of distant metastasis.
TREATMENT
Surgery
The treatment of ACC requires a multidisciplinary management, and surgery is the key therapeutic option that offers a possibility of cure for resectable ACCs: either open adrenalectomy (OA), or minimally invasive surgery. Therefore, staging prior to surgery is essential to rule out invasion of adjacent organs and distant metastases as one-third of patients present with distant metastases, especially lung and liver.11 Based on a retrospective study of 201 patients who underwent adrenalectomy for primary ACC, there is no difference in R0 (negative resection margin) status, tumour recurrence, intraoperative tumour rupture, evidence of microvascular or capsular invasion, overall morbidity, or complications between minimally invasive surgery and OA.32 Similarly, a meta-analysis of data from nine retrospective case-control studies reported no difference in the overall recurrence rate, time to recurrence, cancer specific mortality between open and laparoscopic adrenalectomy. ACCs treated laparoscopically were of small size and more localised (Stage I–II) than OA. Laparoscopic adrenalectomy can offer a shorter hospital stay and a faster recovery; however, it is associated with higher development of peritoneal carcinomatosis (that may possibly be attributed to violation of the tumour capsule during manipulation).33
Complete surgical resection is critical in the management of ACCs and approximately two-thirds to three-quarters had lymph node involvement in autopsy studies.34,35 Moreover, regional lymph node metastasis is an established predictor of poor long-term outcome; however, routine lymphadenectomy during surgical resection of ACC is not commonly performed and its therapeutic role remains controversial. In a multi-institutional study of 120 ACC patients undergoing complete RO resection, peritumoural lymph node dissection (performed in 27%) was independently associated with improved OS. For the study peritumoural lymph node dissection was performed in 27% and associated with large tumours, macroscopically involved lymph nodes, or invasion of adjacent organs.36 Similarly, in a study from the German ACC registry of 283 non-metastatic ACC patients who underwent complete, margin-negative resection, lymphadenectomy was performed in 17% of cases, and was associated with improved disease specific survival.37 On the contrary, a larger population study of data from 18 registries involving 1,525 patients failed to prove the survival benefit of lymphadenectomy, performed in 8% of the population. However, lymphadenectomy should be considered in patients with locally advanced tumours (T3 and T4) which have a higher rate of lymph node metastasis.38
Debulking surgery is utilised for the removal of large tumours with mechanical signs and to reduce hormone excess; however, the median survival is <12 months.13 Between 30% and 40% of ACC are metastatic at the onset, and surgical treatment of liver or lung metastasis is associated with long-term survival.39,40 Recurrence of ACC is relatively common even after curative resection and can be detected in 40–65% within 2 years with a median time to recurrence of 19 months.41 Repeat curative-intent resection for recurrent ACC in carefully selected patients with two or more factors (solitary tumour, disease-free interval >12 months, and locoregional or pulmonary recurrence) could result in a favourable long-term survival.42
Mitotane
Mitotane (Lysodren®, o,p’-DDD) is an adrenocorticotropic drug used for adjuvant therapy after surgical resection, for primary therapy of unresectable cases, and for advanced ACC as a single treatment or in combination with chemotherapy.6 The 2012 European Society for Medical Oncology (ESMO) guidelines recommend adjuvant mitotane therapy in high-risk surgically treated patients, defined as Stage III, Ki-67 LI >10%, R1 or Rx resection. However, it is not mandatory for low-risk patients with Stage I or II, R0 resection and Ki-67 LI ≤10%.43 Adjuvant mitotane is routinely started within 3 months of surgery with appropriate monitoring of blood levels and titrating the dose to a concentration of 14–20 mg/L.2 A recent retrospective analysis demonstrated that blood mitotane concentrations of ≥14 mg/L were associated with a prolonged recurrence-free survival in patients receiving mitotane adjuvant therapy following macroscopically radical surgery.44 Side effects include gastrointestinal upset, elevation of liver function tests, leucopenia, and confusion.45
Radiotherapy
The role of adjuvant radiotherapy in ACC is unclear and the benefits or recommendations cannot be well established due to the lack of prospective large studies. In a retrospective study, radiotherapy prolongs 5 year recurrence-free survival, with no effect on OS and disease-free survival.46 Another study showed no difference in local recurrencefree rate at 5 years between surgery with adjuvant radiotherapy and surgery alone.47 Radiotherapy was associated with a 4.7-fold reduction in the risk of local failure compared to treatment regimens without radiotherapy.48 Thus, adjuvant radiotherapy should be considered in patients with incomplete, R1, or Rx resection, who are at high risk for local recurrence.13 CyberKnife® treatment, a stereotactic radiosurgery which deliver high-dose radiation beams to tumours with extreme accuracy, can also be safe and effective for advanced adrenocortical carcinoma, though there are only a few case reports currently available for this option.49
Chemotherapy
According to the first international randomised trial in locally advanced and metastatic adrenocortical carcinoma treatment (FIRM-ACT trial), patients who received mitotane plus a combination of etoposide, doxorubicin, and cisplatin (M-EDP) had a higher response rate than those in the streptozocinmitotane group (23.2% versus 9.2%), although there was no significant difference in the OS.50 For failed cases with M-EDP, second-line chemotherapy using a combination of gemcitabine and capecitabine is proposed which leads to disease stabilisation for at least 6 months in 29% of patients.51
Targeted Therapy
Trials on monoclonal antibodies against various angiogenic receptor tyrosine kinases, such as bevacizumab, sorafenib, sunitinib, and axitinib, yielded disappointing results. Similarly, inhibitors of epithelial growth factor receptor (erlotinib and gefitinib) and IGF-1 (linsitinib, cixutumumab) are not promising in ACC. Recently, novel agents to target steroidogenic factor-1, mTOR, and Wnt signalling pathways have been developed. Inhibitors of acetyl-coA cholesterol acetyl transferase 1, an enzyme for intracellular cholesterol handling, have gained some interest as a potential therapy. With trials underway, these novel targeted agents might be useful for clinical applications in the future.52
PROGNOSIS
Even after complete surgical resection with negative margins, the rate of recurrence is high with a 5-year survival rate of 32–45%.53,54 In a recent study completed in 13 institutions in the USA over a 20-year period, from 1993–2014, there were 49 5-year survivors (27%) and 12 10-year survivors (7%) among 180 patients who underwent resection for ACC. The factors associated with early mortality include positive margins, capsular invasion, distant metastasis, and vena cava involvement.55








